世界卫生组织急性白血病分型2016版与2008版区别
杨晓阳,万梦婕,陈方平
·全科医生知识窗·
世界卫生组织急性白血病分型2016版与2008版区别
杨晓阳,万梦婕,陈方平
时隔8年世界卫生组织(WHO)对急性白血病分型进行了修改,本文介绍了WHO急性白血病分型2016版与2008版的区别,结合细胞遗传学和预后等分析了2016版对2008版进行删除或增加的原因。WHO急性白血病分型2016版能更好地结合和指导临床。为了临床医生能及时掌握最新急性白血病分型,并积极为医学创新做准备,本文比较分析WHO急性白血病分型2016版与2008版的区别。
白血病;世界卫生组织;分型
杨晓阳,万梦婕,陈方平.世界卫生组织急性白血病分型2016版与2008版区别[J].中国全科医学,2016,19(26):3253-3256.[www.chinagp.net]
YANG X Y,WAN M J,CHEN F P.Difference between the classification of acute leukemia by world health organization in 2016 and 2008 editions[J].Chinese General Practice,2016,19(26):3253-3256.
世界卫生组织(WHO)对急性白血病进行分型后,明显提高了对急性白血病的诊断和预后的认识。但自2008年WHO急性白血病分型[1]公布后,对于急性白血病分型的认识一直处于摸索和探讨中,尤其是鉴于新一代基因测序技术的突飞猛进。为能更准确描述诊断和预后,2016年WHO又对急性白血病分型进行了修改[2]。此次修改只是对于2008版的完善,此次工作是由100位病理学家、血液学家、肿瘤学者以及遗传学者共同参与完成。由于对2008版比较熟悉,本文主要对2016版(见表1)和2008版的变化进行阐述。
1 急性髓系白血病(AML)伴重现型遗传异常
此种类型的白血病主要出现于儿童患者,此次修改主要是:
1.1MLL基因的命名更改为KMT2A,inv(3)(q21.3q26.2)或t(3;3)(q21.3;q26.2)不代表融合基因,而被定义为激活MECOM表达的远端GATA2增强子以及协同GATA2单倍剂量不足(haploinsufficiency)[3]。
1.2由于PML/RAR基因除了t(15;17)(q24.1;q21.2)外还有其他类型的染色体异常,故只保留了急性早幼粒细胞白血病伴PML/RAR,暂不对染色体异常进行单列。
1.3临时新增AML伴BCR-ABL1突变,此种疾病是新发现的AML,可以从络氨酸激酶抑制剂的治疗中获益[4]。此种命名如缺乏病史,和慢性粒细胞白血病转化的AML有时难以区分,仅有初步报道认为有IGH、TCR、IKZF1和/或CDKN2A基因缺失,支持AML伴BCR-ABL1,可排除慢性粒细胞白血病转化型[5]。
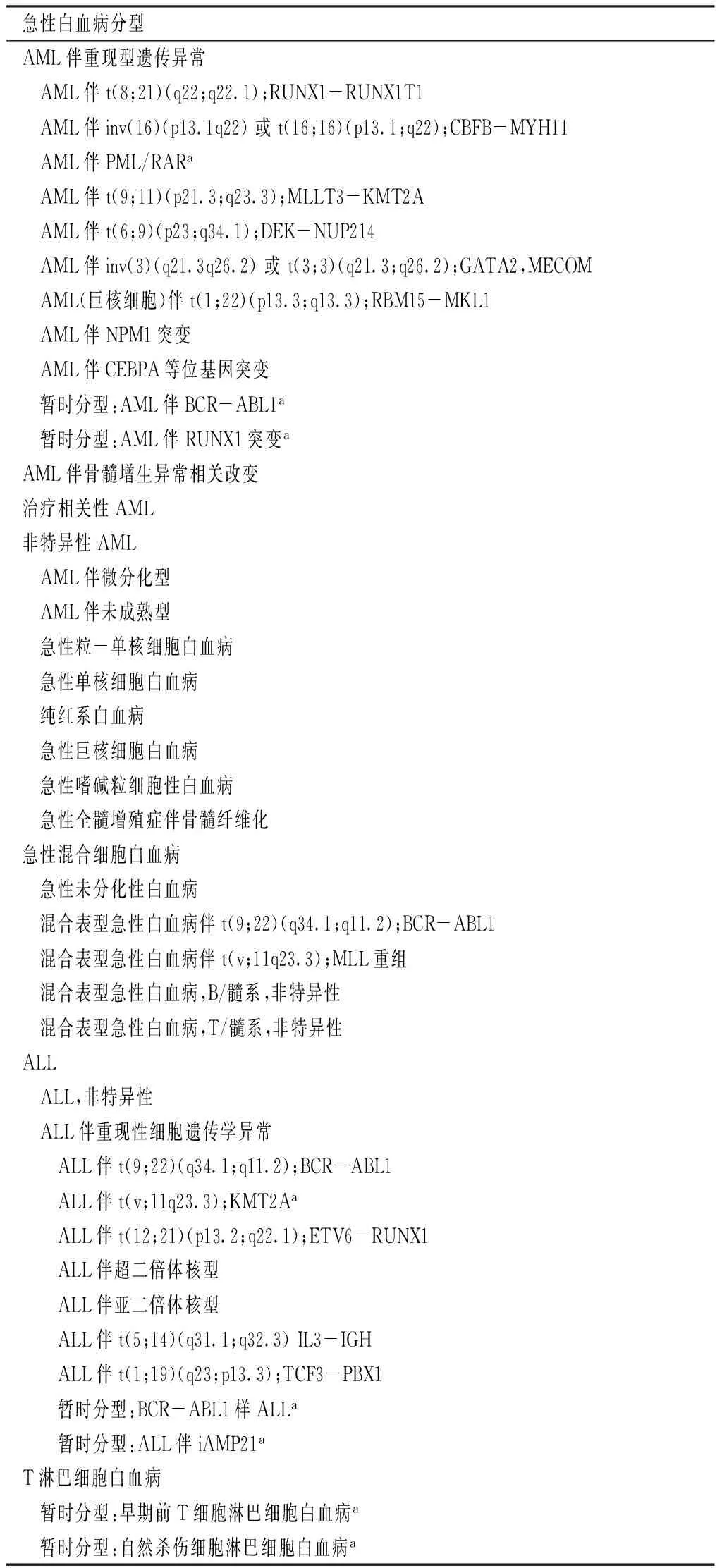
表1 世界卫生组织急性白血病分型2016版
注:AML=急性髓系白血病,ALL=B淋巴细胞白血病;a为新增加分型
1.4暂时新增AML伴RUNX1突变,因RUNX1突变与骨髓增生异常综合征不具有相关性,但如初治的AML患者有该突变,常提示预后不良[6]。
2 AML伴骨髓增生异常相关改变
与2008版相比,此种类型急性白血病未做更改,只是再次强调AML伴骨髓增生异常相关改变预后不良。而有NPM1或者等位基因CEBPA突变的急性白血病[7-8],尚不能提示预后不好,即使有多系病态造血,亦不能归为AML伴骨髓增生异常相关改变,应归为AML伴重现型遗传异常类型。如果没有以上基因的突变,形态学发现有两系50%及以上的病态造血,取消了红白血病的诊断,仍提示为AML伴骨髓增生异常相关改变,并且预后不良[2]。有骨髓增生异常综合征相关的细胞基因学异常可以归为AML伴骨髓增生异常相关改变,但是有del(9q)除外,因为AML伴骨髓增生异常相关改变常伴有NPM1或者等位基因CEBPA突变[9]。
3 治疗相关性AML
与2008版相比,此种类型急性白血病未做更改。
4 非特异性AML
≥20%的髓系原始+幼稚细胞不属于其他类型才能归入此种分型[10]。非特异性AML分型仅有急性红白血病有更改。急性红白血病2008版归为非特异性AML,目前属于AML伴骨髓增生异常相关改变,其诊断标准为≥50%的骨髓幼红细胞以及≥20%的髓系原始+幼稚细胞[11]。
5 急性混合细胞白血病
与2008版相比,此种类型急性白血病未做更改。2008年以来的临床数据支持,有t(9;22)改变对络氨酸激酶抑制剂有效[12]。
6 B淋巴细胞白血病(ALL)
6.1同以上AML分型,MLL基因的命名更改为KMT2A,即ALL/淋巴瘤伴t(v;11q23.3);KMT2A。
6.2暂时新增BCR-ABL1样ALL。此种类型急性白血病常提示预后不良,部分患者对络氨酸激酶抑制剂治疗有效。对于此种类型急性白血病的定义仍存在困难,主要不同研究组分别报道了预后不良的ALL伴有与BCR-ABL1类似的基因表达[13-14],但是不同研究组的定义规则,用于相同的疾病并不能得出相同的结果[15]。BCR-ABL1样ALL共同的特性是包括其他的络氨酸激酶易位,或者包括激酶受体样因子2(CRLF2)易位,或者不常见的重排导致截短和红细胞生成素受体激活[16-17]。出现基因易位的类型有包含络氨酸激酶的ABL1基因(不含BCR基因)的突变,还有其他激酶如ABL2、PDGFRB、NTRK3、TYK2、CSF1R和AK2[18]。超过30种基因突变已经被报道,其中有EBF1-PDGFRB易位,对于络氨酸激酶抑制剂效果好,及时常规化疗无效[19]。BCR-ABL1样ALL常出现IKZF1和CDKN2A/B缺失,但是此种缺失在其他类型的ALL中亦有出现[15]。
6.3暂时新增ALL伴iAMP21。此种类型急性白血病主要是21染色体内某一成分的扩增,通过荧光原位杂交(FISH)探针探测RUNX1基因可以发现5个或者更多的基因复本,或者有3个及以上的不正常的21号染色体的额外复本产生[20]。此种类型急性白血病占儿童ALL的2%,尤其是年龄较大的儿童,临床常有低白细胞计数。成年人中此种类型急性白血病并不多见。ALL伴iAMP21常提示预后不良,但对于部分患者,侵袭性的治疗可能有效[20]。
6.4删除Burkitt白血病,即FAB L3,将其归入其他类型ALL。
7 T淋巴细胞白血病
7.1暂时新增早期前T细胞淋巴细胞白血病(ETP ALL),此种类型急性白血病大多预后不良,但有部分研究得到可喜的治疗效果[21-22]。其有特征性改变,如表达CD7、CD2和胞质CD3,缺少CD1a和CD8,有1个或多个髓系或者干细胞标记,比如CD34、CD117、HLADR、CD13、CD33、CD11b或者CD65,CD5经常阴性表达[23],常有髓系相关基因突变,如FLT3、NRAS/KRAS、DNMT3A、IDH1和IDH2等[23],亦可表现T淋巴细胞白血病基因突变,如NOTCH1或CDKN1/2[23]。

当许多临床医生对WHO急性白血病分型2008版还未完全应用时,最新的2016版又出现在我们面前。更好地给患者提高诊疗和判断预后,是每个医务工作者不可推脱的责任和义务。此文只是抛砖引玉,希望我国的医务工作者,能为下一次WHO急性白血病分型更新添砖加瓦。
作者贡献:杨晓阳进行课题设计与实施、资料收集整理、撰写论文、成文并对文章负责;万梦婕、陈方平进行课题实施、评估、资料收集;陈方平进行质量控制及审校。
本文无利益冲突。
[1]CAMPO E,SWERDLOW S H,HARRIS N L,et al.The 2008 WHO classification of lymphoid neoplasms and beyond:evolving concepts and practical applications [J].Blood,2011,117(19):5019-5032.
[2]ARBER D A,ORAZI A,HASSERJIAN R,et al.The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia [J].Blood,2016,127(20):2391-2405.
[3]GROSCHEL S,SANDERS M A,HOOGENBOEZEM R,et al.A single oncogenic enhancer rearrangement causes concomitant EVI1 and GATA2 deregulation in leukemia [J].Cell,2014,157(2):369-381.
[4]KONOPLEV S,YIN C C,KORNBLAU S M,et al.Molecular characterization of de novo philadelphia chromosome-positive acute myeloid leukemia [J].Leuk Lymphoma,2013,54(1):138-144.
[5]NACHEVA E P,GRACE C D,BRAZMA D,et al.Does BCR/ABL1 positive acute myeloid leukaemia exist? [J].Br J Haematol,2013,161(4):541-550.
[6]MENDLER J H,MAHARRY K,RADMACHER M D,et al.RUNX1 mutations are associated with poor outcome in younger and older patients with cytogenetically normal acute myeloid leukemia and with distinct gene and MicroRNA expression signatures [J].J Clin Oncol,2012,30(25):3109-3118.
[7]FALINI B,MACIJEWSKI K,WEISS T,et al.Multilineage dysplasia has no impact on biologic,clinicopathologic,and prognostic features of AML with mutated nucleophosmin(NPM1) [J].Blood,2010,115(18):3776-3786.
[8]BACHER U,SCHNITTGER S,MACIJEWSKI K,et al.Multilineage dysplasia does not influence prognosis in CEBPA-mutated AML,supporting the WHO proposal to classify these patients as a unique entity [J].Blood,2012,119(20):4719-4722.
[9]SCHLENK R F,TASKESEN E,VAN NORDEN Y,et al.The value of allogeneic and autologous hematopoietic stem cell transplantation in prognostically favorable acute myeloid leukemia with double mutant CEBPA [J].Blood,2013,122(9):1576-1582.
[10]WALTER R B,OTHUS M,BURNETT A K,et al.Significance of FAB subclassification of "acute myeloid leukemia,NOS" in the 2008 WHO classification:analysis of 5848 newly diagnosed patients [J].Blood,2013,121(13):2424-2431.
[11]WANG S A,HASSERJIAN R P.Acute erythroleukemias,acute megakaryoblastic leukemias,and reactive mimics:a guide to a number of perplexing entities [J].Am J Clin Pathol,2015,144(1):44-60.
[12]SHIMIZU H,YOKOHAMA A,HATSUMI N,et al.Philadelphia chromosome-positive mixed phenotype acute leukemia in the imatinib era [J].Eur J Haematol,2014,93(4):297-301.
[13]DEN BOER M L,VAN SLEGTENHORST M,DE MENEZES R X,et al.A subtype of childhood acute lymphoblastic leukaemia with poor treatment outcome:a genome-wide classification study [J].Lancet Oncol,2009,10(2):125-134.
[14]CLAPPIER E,GRARDEL N,BAKKUS M,et al.IKZF1 deletion is an independent prognostic marker in childhood B-cell precursor acute lymphoblastic leukemia,and distinguishes patients benefiting from pulses during maintenance therapy:results of the EORTC children′s Leukemia group study 58951 [J].Leukemia,2015,29(11):2154-2161.
[15]BOER J M,MARCHANTE J R,EVANS W E,et al.BCR-ABL1-like cases in pediatric acute lymphoblastic leukemia:a comparison between DCOG/Erasmus MC and COG/St.Jude signatures [J].Haematologica,2015,100(9):e354-357.
[16]ROBERTS K G,MORIN R D,ZHANG J,et al.Genetic alterations activating kinase and cytokine receptor signaling in high-risk acute lymphoblastic leukemia [J].Cancer Cell,2012,22(2):153-166.
[17]HUNGER S P,MULLIGHAN C G.Redefining ALL classification:toward detecting high-risk ALL and implementing precision medicine [J].Blood,2015,125(26):3977-3987.
[18]ROBERTS K G,LI Y,PAYNE-TURNER D,et al.Targetable kinase-activating lesions in Ph-like acute lymphoblastic leukemia [J].N Engl J Med,2014,371(11):1005-1015.
[19]WESTON B W,HAYDEN M A,ROBERTS K G,et al.Tyrosine kinase inhibitor therapy induces remission in a patient with refractory EBF1-PDGFRB-positive acute lymphoblastic leukemia [J].J Clin Oncol,2013,31(25):e413-416.
[20]HARRISON C J,MOORMAN A V,SCHWAB C,et al.An international study of intrachromosomal amplification of chromosome 21(iAMP21):cytogenetic characterization and outcome [J].Leukemia,2014,28(5):1015-1021.
[21]PATRICK K,WADE R,GOULDEN N,et al.Outcome for children and young people with early T-cell precursor acute lymphoblastic leukaemia treated on a contemporary protocol,UKALL 2003 [J].Br J Haematol,2014,166(3):421-424.
[22]WOOD B L,WINTER S S,DUNSMORE K P,et al.T-Lymphoblastic Leukemia(T-ALL) shows excellent outcome,lack of significance of the Early Thymic Precursor(ETP) immunophenotype,and validation of the prognostic value of end-induction Minimal Residual Disease(MRD) in Children′s Oncology Group(COG) Study AALL0434 [J].Blood,2014,124(21):1.
[23]JAIN N,LAMB A V,O′BRIEN S,et al.Early T-cell precursor acute lymphoblastic leukemia/lymphoma(ETP-ALL/LBL) in adolescents and adults:a high-risk subtype [J].Blood,2016,127(15):1863-1869.
(本文编辑:陈素芳)
Difference between the Classification of Acute Leukemia by World Health Organization in 2016 and 2008 Editions
YANGXiao-yang,WANMeng-jie,CHENFang-ping.DepartmentofHematology,CentralSouthUniversityXiangyaSchoolofMedicineAffiliatedHaikouHospital,HaikouPeople′sHospital,Haikou570208,China
Correspondingauthor:YANGXiao-yang,DepartmentofHematology,CentralSouthUniversityXiangyaSchoolofMedicineAffiliatedHaikouHospital,HaikouPeople′sHospital,Haikou570208,China;DepartmentofHematology,XiangyaHospitalCentralSouthUniversity,Changsha410008,China;E-mail:y108108@126.com
After eight years,the World Health Organization(WHO) has made amendments on the classification of acute leukemia.The differences between classification of acute leukemia by WHO in 2016 and 2008 editions are introduced in this paper.The reasons for deleting or adding contents in the 2016 edition based on the 2008 edition are analyzed in combination with cytogenetics and prognosis.The classification of acute leukemia by WHO in the 2016 edition can better combine and guide clinical practices.The differences between the classification of acute leukemia by WHO in the 2016 and 2008 editions are reviewed to help clinical doctors understand the latest types of acute leukemia and prepare for medical innovation.
Leukemia;World health organization;Classification
570208海南省海口市,中南大学湘雅医学院附属海口医院暨海口市人民医院血液科(杨晓阳,万梦婕);中南大学湘雅医院血液科(杨晓阳,陈方平);中南大学湘雅三医院血液科(陈方平)
杨晓阳,570208海南省海口市,中南大学湘雅医学院附属海口医院暨海口市人民医院血液科,中南大学湘雅医院血液科;E-mail:y108108@126.com
R 733.7
A
10.3969/j.issn.1007-9572.2016.26.026
2016-06-06;
2016-07-20)