妊娠晚期B族链球菌感染患者敏感性抗生素预防性治疗时机对母婴结局的影响
舒艳子 陈星 张秀果


【摘要】 目的:探究妊娠晚期B族鏈球菌感染(GBS)患者敏感性抗生素预防性治疗时机对母婴结局的影响。方法:选取2019年4月1日-2020年3月31日在本院收住的GBS感染者70例为研究对象,将其分为A、B组,每组35例。A组于妊娠35~37周给予青霉素G预防治疗,B组于临产或胎膜早破后给予青霉素G或氨苄青霉素治疗,并以2018年4月1日-2019年3月31日在本院行产检并确诊GBS感染者但未进行抗生素治疗的孕妇35例为C组,比较三组母婴不良结局发生率、自然分娩率、分娩时间及产后出血量,比较三组给药前后凝血功能[血清纤维蛋白原水平、凝血酶原时间(PT)]。结果:A组产妇及新生儿不良妊娠结局发生率低于C组(P<0.05),B、C组产妇及新生儿不良妊娠结局发生率对比差异无统计学意义(P>0.05);A组的自然分娩率高于C组,分娩时间短于B组、C组,产后出血量少于B组、C组(P<0.05),B组分娩时间短于C组,产后出血量少于C组(P<0.05);分娩后,A组血清纤维蛋白酶原含量低于B组、C组,PT值小于B组、C组(P<0.05),分娩后,B组PT值小于C组(P<0.05)。结论:在妊娠晚期GBS患者35~37周基于抗生素预防,可降低产妇及新生儿不良妊娠结局发生率,减少产后出血量,改善凝血功能。
【关键词】 妊娠晚期 B族链球菌感染 敏感性抗生素 治疗时机
[Abstract] Objective: To investigate the effect of the timing of prophylactic treatment with sensitive antibiotics on the outcome of pregnant women with group B streptococcus infection (GBS). Method: From April 1, 2019 to March 31, 2020, 70 patients with GBS infection in our hospital were selected as the study objects, they were divided into groups A and B, 35 cases in each group. Group A was given Penicillin G prophylactic treatment at 35-37 weeks of gestation, group B was given Penicillin G or Ampicillin after parturition or premature rupture of membranes, 35 pregnant women with GBS infection diagnosed in our hospital from April 1, 2018 to March 31, 2019 were taken as group C to compare the incidence of adverse maternal and infant outcomes; the natural delivery rate, delivery time and postpartum delivery time of the three groups were compared Blood loss, blood coagulation [serum fibrinogen level, prothrombin time (PT)] before and after administration were compared among the three groups. Result: The incidence of adverse pregnancy outcome in group A was lower than that in group C (P<0.05), and there was no significant difference between group B and group C (P>0.05); the natural delivery rate in group A was higher than that in group C, the delivery time was shorter than that in group B and group C, the postpartum hemorrhage was less than that in group B and group C (P<0.05), the delivery time in group B was shorter than that in group C, and the postpartum hemorrhage was less than that in group C (P<0.05). After delivery, the serum fibrinogen content in group A was lower than that in group B and C, and the PT value in group B was lower than that in group C (P<0.05). After delivery, the PT value in group B was lower than that in group C (P<0.05). Conclusion: antibiotic based prophylaxis can reduce the incidence of adverse pregnancy outcome, reduce postpartum hemorrhage and improve coagulation function in patients with GBS in the third trimester.
[Key words] Late pregnancy Group B streptococcal infection Sensitive antibiotics Timing of treatment
B族链球菌(Group B streptococcus,GBS)是导致妊娠期妇女生殖道感染的主要致病菌,不仅会引起母婴垂直感染,导致新生儿早、迟发感染的出现,还会诱发产妇败血症及新生儿脑膜炎,具有较高的致死率,严重威胁了产妇及新生儿的生命安全[1-2]。有报道指出,GBS患者妊娠晚期出现早产及新生儿感染的概率远高于正常产妇[3-4]。目前常采用青霉素G或氨苄青霉素等抗生素治疗GBS妊娠晚期患者,可通过抑制GBS生存及繁殖来起到降低不良事件的发生率,但不同治疗时机可能会导致治疗疗效存在差异。本研究通过对比35~37周及临产产妇应用抗生素治疗的临床效果,旨在探究治疗时机对患者母婴结局的影响,现报道如下。
1 资料与方法
1.1 一般资料 选取2019年4月1日-2020年3月31日在本院收住的GBS感染者70例为研究对象,将其分为A、B组,每组35例。A组于妊娠35~37周给予青霉素G预防治疗,B组于临产或胎膜早破后给予青霉素G或氨苄青霉素治疗,并以2018年4月1日-2019年3月31日在本院行产检并确诊GBS感染者但未进行抗生素治疗的孕妇35例为C组。(1)纳入标准:①经阴道GBS培养确诊为GBS患者[5];②单胎妊娠。(2)排除标准:①其他感染性疾病患者;②多胎妊娠者;③入组前1个月内有抗菌药物应用史者;④肝肾功能异常者;⑤对本研究药物过敏者;⑥严重血液疾病患者;⑦严重妊娠合并症者。所有患者均知情同意并签署同意书,研究经本院伦理委员会审核通过。
1.2 方法 A、B组产妇均于术前接受抗生素药敏试验。A组于35~37周给予抗生素预防治疗:青霉素G(生产厂家:石药集团中诺药业有限公司,批准文号:国药准字H20033291),500万U/d,静脉滴注,分2~4次,共治疗5 d。B组于临产或胎膜早破后给予抗生素治疗:青霉素G500万U或氨苄青霉素(生产厂家:成都倍特药业股份有限公司,批准文号:国药准字H13021726)2 g,加入250 mL 0.9%氯化钠注射液,静脉滴注,然后给予250万U青霉素G或1 g氨苄青霉素治疗,4 h/次,直至分娩。C组未接受抗生素治疗。
1.3 观察指标及评价标准 (1)母婴不良妊娠结局:于产妇生产后,比较三组产妇及新生儿不良妊娠结局发生率。新生儿不良妊娠结局:胎儿生长受限、胎儿窘迫、宫内感染、新生儿侵袭性疾病;产妇不良妊娠结局:胎膜早破、产褥感染、早产。(2)比较三组患者自然分娩率、分娩时间及产后出血量。(3)凝血功能:比较三组治疗前及分娩后血清纤维蛋白原含量及PT值,采集患者5 mL静脉血,离心分离血清,采用酶联免疫吸附法检测血清纤维蛋白原含量;将已采集的静脉血加入含有1/10体积0.109 mol/L枸橼酸钠抗凝液的硅化玻璃管中,离心10 min,转速为3 000 r/min,用试管取上层液体0.1 mL,于37 ℃下孵育2 min,在试管中加入凝血活酶0.2 mL,混匀,用秒表记录凝血酶原时间(PT)。
1.4 统计学处理 使用SPSS20统计软件进行数据处理,计量资料采用(x±s)表示,比较采用t检验,计数资料采用率(%)表示,比较采用字2检验,以P<0.05为差异有统计学意义。
2 结果
2.1 两组基线资料比较 A组年龄21~38岁,平均(29.15±4.29)岁;生产次数0~2次,平均(0.97±0.42)次;孕周35~37周,平均(36.02±0.49)周。B组年龄20~39岁,平均(29.64±4.16)岁;生产次数0~2次,平均(1.02±0.47)次。C组年龄20~36岁,平均(29.11±4.04)岁;生产次数0~2次,平均(1.07±0.41)次。三组在年龄、生产次数方面对比差异均无统计学意义(P>0.05),具有可比性。
2.2 三组母婴不良妊娠结局发生情况比较 A组产妇及新生儿不良妊娠结局发生率均低于C组(P<0.05),B、C组产妇及新生儿不良妊娠结局发生率对比差异无统计学意义(P>0.05)。见表1、2。
2.3 三组凝血功能指标比较 三组治疗前血清纤维蛋白原含量及PT值對比,差异均无统计学意义(P>0.05);分娩后,A组血清纤维蛋白原含量低于B组、C组,PT值小于B组、C组(P<0.05);分娩后,B组PT值小于C组(P<0.05)。见表3。
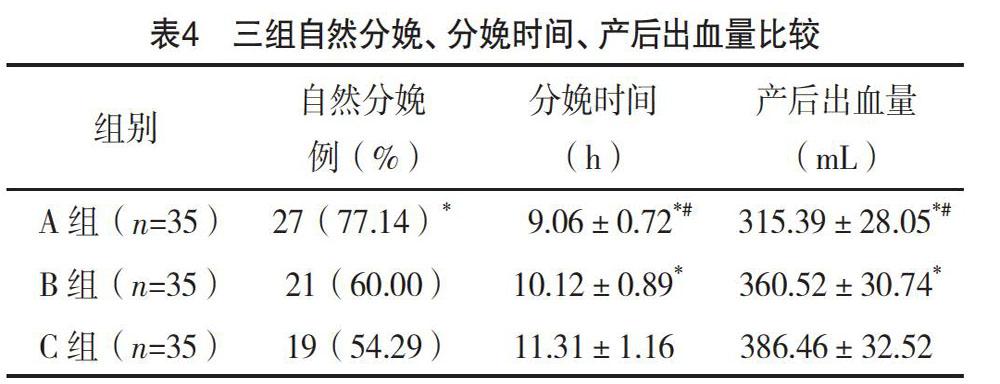
2.4 三组自然分娩率、分娩时间、产后出血量比较A组的自然分娩率高于C组(P<0.05);A组分娩时间短于B组、C组,产后出血量少于B组、C组(P<0.05);B组分娩时间短于C组,产后出血量少于C组(P<0.05),见表4。
3 讨论
GBS为无乳链球菌,为兼性厌氧的革兰阳性链球菌,正常寄居于阴道和直肠,属于条件致病菌[6-7]。因孕期免疫力降低,孕妇受GBS感染的危险性大大增加[8],另外,GBS可在孕妇生殖道逆行至宫腔,进而可能导致产妇及新生儿不良妊娠结局的发生[9]。有研究指出,在GBS患者妊娠第35~37周给予抗生素治疗,可起到降低母婴不良妊娠结局的发生率[10-12]。对GBS患者妊娠35~37期给予抗生素治疗,可减轻或消除GBS引起的炎症反应,降低尿路感染、宫内膜感染、胎膜感染等感染相关疾病的发生率,进而可降低不良妊娠结局发生率。本研究中,A组产妇及新生儿不良妊娠结局发生率低于C组(P<0.05),表明对妊娠晚期GBS患者第35~37周给予抗生素治疗,可降低母婴不良结局发生率,与上述研究一致。
GBS是导致严重围生期感染最主要的致病菌之一,随着妊娠时间的推移,可导致绒毛膜羊膜炎和胎膜早破的发生,不利于正常妊娠的进行[13]。有报道指出,及时发现并尽早治疗GBS感染,对减少母婴发病及提高自然分娩率具有重要意義[14-15]。对GBS患者尽早给予抗生素治疗,可改善阴道内环境,并促进生殖器官功能的恢复,可促进正常妊娠的进行,进而可提高自然分娩率。本研究发现,A组的自然分娩率高于C组,分娩时间短于B组、C组,(P<0.05),说明对妊娠晚期GBS患者第35~37周给予抗生素治疗,可提高自然分娩率,缩短分娩时间。Mengist等[16]研究选择不同时机对妊娠晚期GBS患者给予抗生素治疗,进一步证实了在患者35~37周时给予预防治疗,可提高自然分娩率,与本研究结构相同。
GBS感染会引起全身炎性反应,造成组织损伤的出现,导致孕妇血浆中凝血因子及激肽释放原水平异常,进而导致其出现凝血功能障碍[17-19]。对GBS患者尽早给予抗生素治疗,可在一定程度上降低阴道及直肠内GBS带菌量,进而减轻炎症反应,改善凝血功能。本研究中,A组血清纤维蛋白酶原含量低于B组、C组,PT值、产后出血量小于B组、C组(P<0.05),说明在妊娠晚期GBS患者35~37周给予抗生素治疗,可改善其凝血功能,与Amy等[20]研究结果相同。
综上所述,在妊娠晚期GBS患者35~37周基于抗生素预防,可降低产妇及新生儿不良妊娠结局发生率,减少产后出血量,改善凝血功能,另外,抗生素预防治疗虽能控制GBS感染,但往往会加剧产道内其他耐药菌感染,不利于产妇妊娠,因此需根据产妇情况决定治疗时机。
参考文献
[1]吉地阿依,马健,童闻,等.孕晚期孕妇B族链球菌带菌情况和危险因素及应用抗生素预防性治疗对母婴结局的影响[J].实用临床医药杂志,2017,21(19):194-196.
[2]陆少颜,徐烨,陈泳言,等.分娩时抗生素预防性治疗后新生儿B族链球菌感染情况分析[J].中国妇幼保健,2017,32(6):1205-1206.
[3] Zheng F,Spreckelsen N V,Zhang X,et al.Should preventive antibiotics be used in patients with acute stroke. A systematic review and meta-analysis of randomized controlled trials[J].PLoS One,2017,12(10):18667-18668.
[4] Yuanyuan W,Zijp T R,Akbar B M,et al.Effects of prophylactic antibiotics on patients with stable COPD: a systematic review and meta-analysis of randomized controlled trials[J].Journal of Antimicrobial Chemotherapy,2018,12(4):1-13.
[5] Skoetz N,Bohlius J,Engert A,et al.Prophylactic antibiotics or G(M)-CSF for the prevention of infections and improvement of survival in cancer patients receiving myelotoxic chemotherapy[J].Cochrane Database of Systematic Reviews,2015,12(12):7107-7109.
[6]郑建琼,陈海迎,倪菲菲,等.产时抗生素预防对B族溶血性链球菌定植产妇新生儿结局影响研究[J].中国实用妇科与产科杂志,2018,34(6):103-107.
[7] Liu X,Zuo X,Sun X,et al.Effects of prophylactic antibiotics before peritoneal dialysis catheter implantation on the clinical outcomes of peritoneal dialysis patients[J].Renal Failure,2019,41(1):16-23.
[8]刘娜,尤建萍,王博,等.妊娠晚期孕妇阴道B族链球菌感染青霉素钠治疗对血浆凝血功能及新生儿结局的影响分析[J].现代检验医学杂志,2019,34(4):146-150.
[9] Keyerleber M A,Lluís F.Effect of prophylactic cefalexin treatment on the development of bacterial infection in acute radiation-induced dermatitis in dogs: a blinded randomized controlled prospective clinical trial[J].Veterinary Dermatology,2017,29(1):37-38.
[10]罗力冰,周镇邦,劳锦辉,等.孕晚期B族链球菌筛查及分娩期预防性抗生素治疗效果的临床分析[J].中华围产医学杂志,2018,21(8):537-540.
[11] Jong-Sun K , Wan-Sik L , Cho-Yun C , et al.Clinical Impact of Prophylactic Antibiotic Treatment for Self-Expandable Metallic Stent Insertion in Patients with Malignant Colorectal Obstruction[J].Gastroenterology Research and Practice,2015,2015:416142.
[12]李亚超.妊娠晚期B族链球菌带菌者应用敏感抗生素预防性治疗的疗效及治疗时机分析[J].中国处方药,2019,17(5):45-46.
[13] Zhou F W,Zhou W Y,Zhu Q.Effect of systematic diet guidance on compliance and Maternal-Infant outcomes in patients with gestational diabetes mellitus[J].World Chinese Journal of Digestology,2017,25(14):1311-1315.
[14]林秀美.妊娠晚期B族链球菌带菌者敏感抗生素预防性治疗时机的选择及比较[J].中国医学创新,2019,16(5):133-136.
[15] Xu J,Wang J,Xuan S,et al.The Effects of Childbirth Age on Maternal and Infant Outcomes in Pregnant Women[J].Iranian Journal of Public Health,2018,47(6):788-793.
[16] Mengist A,Kannan H,Abdissa A.Prevalence and antimicrobial susceptibility pattern of anorectal and vaginal group B Streptococci isolates among pregnant women in Jimma, Ethiopia[J].BMC Research Notes,2016,9(1):1-5.
[17]刘昱,安莉莉,尹保民.头孢噻肟不同给药时机治疗妊娠晚期孕妇B族溶血性链球菌感染的临床研究[J].实用药物与临床,2018,21(6):647-650.
[18]陆少颜,徐烨,陈泳言,等.分娩时抗生素预防性治疗后新生儿B族链球菌感染情况分析[J].中国妇幼保健,2017,32(6):1205-1206.
[19] Zanardi D M,Moura E C,Santos L P,et al.The effect of maternal near miss on adverse infant nutritional outcomes[J].Clinics,2016,71(10):593-599.
[20] Amy Tanner Tubay,Kate A Mansalis,Matthew J Simpson, et al.The Effects of Group Prenatal Care on Infant Birthweight and Maternal Well-Being:A Randomized Controlled Trial[J].Military Medicine,2018,184(5):440-446.
(收稿日期:2020-06-03) (本文編辑:周亚杰)