胱抑素C对体外循环术后急性肾损伤的早期预测价值的研究
董佳月+倪红英


[摘要] 目的 探讨Cys C在体外循环术后患者急性肾损伤早期诊断中的价值。 方法 选择我院重症监护室2013年7月~2016年10月行体外循环术后患者114例,根据术后有无产生急性肾损伤分为观察组及对照组,测定术后第1、2、3、4天Cys C数值,采用 ROC曲线评价Cys C对体外循环术后急性肾损伤的诊断价值。 结果 结果显示,观察组Cys C1、Cys C2、Cys C3、Cys C4(术后第1、2、3、4天Cys C数值)、Cys Cx(术后Cys C平均值)及Cys Cnl(Cys C标准负荷量)与对照组比较,有统计学差异(P1=0.006,P2=0.022,P3=0.001,P4=0.000,Px=0.000,Pnl=0.005),ROC曲线结果显示,Cys C1的ROC曲线下面积为0.674,Cys C2的ROC曲线下面积为0.672,Cys C3的ROC曲线下面积为0.706,Cys C4的ROC曲线下面积为0.752,Cys Cx的ROC曲线下面积为0.732,Cys Cnl的ROC曲线下面积为0.702,采用Cys C1为早期诊断指标,Cys C1的最佳截断值为1.3 mg/L;多次测量的患者可采用Cys Cnl作为早期诊断指标,Cys Cnl的最佳截断值为1.15 mg/L。 结论 Cys C可作为体外循环术后患者发生急性肾损伤的内源性标志物,Cys C1及Cys Cnl可作为体外循环术后急性肾损伤早期诊断的指標。
[关键词] 重症监护室;胱抑素C;体外循环;急性肾损伤;早期诊断
[中图分类号] R654.2 [文献标识码] A [文章编号] 1673-9701(2017)25-0004-04
Study on the early predictive value of cystatin C in acute kidney injury after cardiopulmonary bypass
DONG Jiayue NI Hongying
Department of Intensive Care Unit (ICU), Jinhua Central Hospital in Zhejiang Province, Jinhua 321000, China
[Abstract] Objective To evaluate the value of CysC in the early diagnosis of acute kidney injury after cardiopulmonary bypass. Methods A total of 114 patients who underwent cardiopulmonary bypass from July 2013 to October 2016 in the ICU in our hospital were selected. According to whether there was the occurrence of acute kidney injury after surgery, the patients were divided into observation group and control group. The value of Cys C was measured at 1, 2, 3 and 4 days after operation. The diagnostic value of Cys C in acute kidney injury after cardiopulmonary bypass was evaluated by ROC curve. Results The results showed that there were statistical differences in Cys C1, Cys C2, Cys C3, Cys C4 (Cys C values on day 1, 2, 3 and 4 days after the surgery), Cys Cx (mean value of Cys C after the surgery) and Cys Cnl (Cys C standard load) between the observation group and the control group (P1=0.006, P2=0.022, P3=0.001, P4=0.000, Px=0.000, Pnl=0.005). The ROC curve showed that the area under the ROC curve of Cys C1 was 0.674, the area under the ROC curve of Cys C2 was 0.672, that of Cys C3 was 0.706, that of Cys C4 was 0.752, that of Cys Cx was 0.732, and that of Cys Cnl was 0.702. Cys C1 was used as the early diagnosis index. The optimal cutoff value of Cys C1 was 1.3 mg/L; Cys Cnl could be used as an early diagnostic index for the patients with multiple measurements. The optimal cutoff value for Cys Cnl was 1.15 mg/L. Conclusion Cys C can be used as an endogenous marker of acute kidney injury in patients after cardiopulmonary bypass. Cys C1 and Cys Cnl can be used as an early diagnosis index of acute kidney injury after cardiopulmonary bypass.endprint
[Key words] Intensive care unit (ICU); Cys C; Cardiopulmonary bypass; Acute kidney injury (AKI); Early diagnosis
胱抑素C(cystatin C,Cys C)是一种半胱氨酸蛋白酶抑制剂,循环中的Cys C仅经肾小球滤过而被清除,不依赖任何外来因素如性别、年龄、饮食的影响,是一种反映肾小球滤过率变化的理想标志物。在重症监护室(intensive care unit,ICU)中,引起急性肾损伤(acute kidney injury,AKI)最常见的疾病是脓毒症,体外循环手术为第二大诱因[1],心脏手术引起AKI的可能原因是肾脏的低灌注和缺血[2-3]。AKI对进行体外循环手术的患者而言,是一种严重的并发症[4]。由于AKI的定义有多个版本,经统计AKI的发病率为10%~40%不等[5-7]。近年来肾损伤领域的研究发现Cys C、中性粒细胞明胶酶相关脂质运载蛋白(neutrophil gelatinase associated lipocalin,NGAL)、尿白细胞介素-18及B型尿钠肽(brain natriuretic peptide,BNP)等生物标记物能够预测AKI的发生[8-11]。本研究通过监测体外循环术后患者Cys C的水平,评价Cys C对体外循环术后AKI早期预测及诊断的价值。
1 资料与方法
1.1 一般资料
研究对象来自于我院ICU 2013年7月~2016年10月行体外循环术后的患者,本院体外循环术后患者均需进入ICU监护治疗,保证了数据收集的完整性。进入ICU后收集患者年龄、原发疾病、性别、体重、急性生理与慢性健康评分Ⅱ(acute physiology and chronic health evaluation Ⅱ,APACHⅡ)、心功能(NYHA心功能分级)等基本信息。排除标准[12]:(1)年龄<15周岁;(2)合并多器官功能衰竭预期生存时间<24 h;(3)既往肾功能衰竭立即要求行透析治疗者。
1.2 实验方法
采集患者的基础肌酐值及术后1、2、3、4天的血清肌酐值、Cys C值、液体进出量。根据有无发生术后AKI分为肾损伤组及非肾损伤组。然后对采集到的数据进行统计分析。AKI的定义为血清肌酐值7 d內较基础肌酐值升高至1.5倍及以上,或连续6 h尿量<0.5 mL/(kg·min)[13]。血清肌酐值及Cys C值由金华市中心医院检验科测验。液体进出量由ICU护士统计。基础肌酐值为患者入院后第一次肌酐检查结果。
1.3统计学方法
采用SPSS22.0软件对数据进行处理。年龄、体重、APACHⅡ评分、血清肌酐值、Cys C值、液体进出量等计量资料采用均数±标准差表示,组间比较采用t检验,性别比例、心功能、原发疾病等构成比等计数资料采用%表示,组间比较采用χ2检验。P<0.05为差异有统计学意义。采用ROC曲线评估术后第1、2、3、4天Cys C的数值、术后Cys C的平均值及Cys C标准负荷量对AKI的早期诊断价值。
2 结果
2.1 基本信息
一般资料纳入流程:心脏外科术后147例患者,选取体外术后循环患者117例,剔除3例资料缺失过多患者,根据术后有无AKI分为肾损伤组20例,非肾损伤组94例。对两组患者的基本信息进行统计,结果显示,两组患者的年龄、性别比、体重、心功能、APACHⅡ评分、肌酐基础值、原发疾病等比较,均无统计学差异(P>0.05),见表1。
2.2 两组Cys C诊断价值结果
对两组患者的Cys C值进行统计并计算,结果显示,两组Cys C1、Cys C2、Cys C3、Cys C4(术后第1、2、3、4天Cys C数值)、Cys Cx(术后Cys C平均值)及Cys Cnl(Cys C标准负荷量)比较,有统计学差异(P<0.05),见表2。
2.3 两组术后Cys C值ROC曲线
ROC曲线结果显示,Cys C1的ROC曲线下面积为0.674,Cys C2的ROC曲线下面积为0.672,Cys C3的ROC曲线下面积为0.706,Cys C4的ROC曲线下面积为0.752,Cys Cx的ROC曲线下面积为0.732,Cys Cnl的ROC曲线下面积为0.702。根据ROC曲线面积结果及早期诊断价值,对于单次测量Cys C的患者可选取Cys C1作为早期预测的指标,计算约登指数(Youden index)后Cys C1的最佳截断值为1.3 mg/L。对于多次测量的Cys C数值可使用Cys Cnl作为早期预测的参数,计算约登指数后Cys Cnl的最佳截断值为1.15 mg/L。见封三图1。
3 讨论
体外循环术后AKI作为一种严重的并发症,能够早期预测、诊断治疗AKI,对患者意义重大。主动脉阻断时间、平均动脉压、液体的进出量均被认为是一个关于体外循环术后AKI发生的重要因素。其中,对于围手术期液体的管理仍有很大的争议[14]。有危重症患者的观察性研究表明液体的正平衡和组织的水肿会加快AKI的进程[15],同样有研究表明液体的过多摄入会使AKI恶化为严重的AKI并降低患者的生存率[16]。有系统评价结果显示保守目标导向的液体管理能减少AKI的发生率[17]。目前,体外循环术后AKI的诊断主要依靠传统的指标如肌酐、尿素氮及尿量的变化,然而这些指标的影响因素较多,且这些指标在肾功能明显受损时才会出现变化,早期预测价值有限,临床需要敏感性及特异性更高的早期预测指标。近年来有一批肾小球滤过率标志物被发现可用于AKI的诊断[18],其中Cys C是一种良好的内源性肾小球滤过率标志物[19]。有研究显示Cys C在慢性肾病的诊断中优于肌酐,且能更好地预测患者的预后[20],故本研究目的在于探讨Cys C对体外循环术后患者AKI的早期诊断价值。endprint
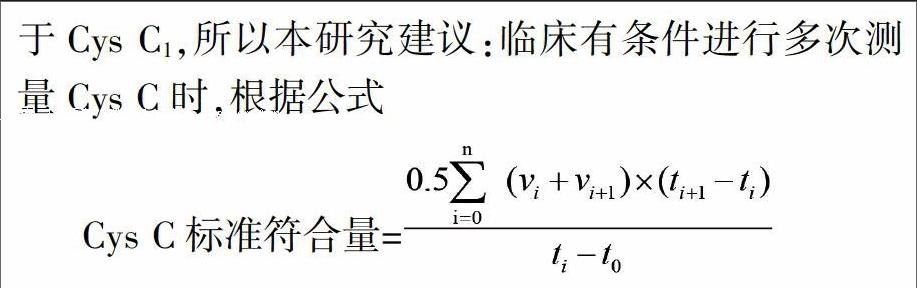
本研究结果显示体外循环患者Cys C对体外循环术后急性肾损伤早期诊断有重要作用。患者采集的Cys C数值中术后第4天值的ROC曲线下面积值最大,故诊断价值最大,但是术后第4天值获得数据时间较晚,對AKI的早期诊断价值不高。由ROC曲线可知,Cys C术后第1天值诊断价值高于术后第2天值,且Cys C术后第1天值获得数据时间较早,在肌酐尚未上升至最高值时已具有预测AKI发生的价值,所以本研究选取Cys C术后第1天值作为诊断指标。约登指数又称为正确指数,是评价筛查试验真实性的方法,计算方法是灵敏度与特异度之和减去1,表示筛检方法发现真正的患者与非患者的总能力,指数越大说明筛查实验的效果越好,真实性越大。我们选取约登指数最大的值为最佳截断值,计算出Cys C术后第1天值诊断AKI的最佳参考值为1.3 mg/L,该结果提示,体外循环术后患者术后第1天Cys C值若大于1.3 mg/L,需考虑并发AKI。由于本研究多次测量Cys C,单独采用Cys C术后第1天值作为诊断参考值时ROC曲线下面积仅为0.674,所以我们对多次采集的Cys C值采用了平均值计算及Cys C标准负荷量的计算,由于平均值计算时并未考虑采集数据时间的因素,故不建议作为最终参考值,我们根据Zhang Z等[13]的研究中关于乳酸标准负荷量的计算方法,提出Cys C标准负荷量的概念,对采集到的Cys C值进行时间因素的加权计算,Cys Cnl的ROC曲线下面积为0.702,大于Cys C1的曲线下面积,提示Cys Cnl的诊断价值要大于Cys C1,所以本研究建议:临床有条件进行多次测量Cys C时,根据公式
计算出CysCnl(v值为采集的Cys C值,t值为采集的时间),使用Cys Cnl为诊断参数,本研究计算约登指数后选取Cys Cnl的最佳截断值为1.15 mg/L,该结果提示体外循环术后患者Cys Cnl若>1.15 mg/L,需考虑并发AKI。
本研究通过监测体外循环术后患者Cys C的水平,研究 Cys C对体外循环术后患者AKI 的预测价值,结果显示,Cys C1及Cys Cnl可作为体外循环术后患者早期预测及诊断指标,若患者Cys C1>1.3 mg/L 或Cys Cnl>1.15 mg/L,需考虑体外循环术后患者并发AKI。Cys C的早期预测价值要高于肌酐值,在患者术后肌酐值尚未上升时即能预测AKI,且较肌酐值的干扰因素较少,所以根据本研究结果,建议临床工作时对于体外循环术后的患者,有条件时应在术后监测Cys C的水平,能有效地预测术后AKI的发生,并能够提前进行干预治疗,改善患者的预后。本研究纳入的患者均为体外循环术后的患者,Cys C对于其他疾病引起的AKI是否具有预测价值,尚待更多研究证明。对于近年来肾损伤领域发现的其他的生物学指标,如NGAL、尿白细胞介素-18及BNP等对体外循环术后患者AKI的预测价值本研究未能纳入,需要更多的临床研究验证。
[参考文献]
[1] Uchino S,Kellum JA,Bellomo R,et al. Acute renal failure in critically ill patients: a multinational,multicenter study[J]. JAMA, 2005,294:813-818.
[2] Kulier A,Levin J,Moser R,et al. Impact of preoperative anemia on outcome in patients undergoing coronary artery bypass graft surgery[J]. Circulation,2007,116:471-479.
[3] Shaw A. Models of preventable disease:contrast-induced nephropathy and cardiac surgery-associated acute kidney injury[J]. Contrib Nephrol,2011,174:156-162.
[4] Mao H,Katz N,Ariyanon W,et al. Cardiac surgery-associated acute kidney injury[J]. Cardiorenal Med,2013,3:178-199.
[5] Englberger L,Suri RM,Connolly HM,et al. Increased risk of acute kidney injury in patients undergoing tricuspid valve surgery[J]. Eur J Cardiothorac Surg,2013,43:993-999.
[6] Englberger L,Suri RM,Li Z,et al. Clinical accuracy of RIFLE and Acute Kidney Injury Network(AKIN)criteria for acute kidney injury in patients undergoing cardiac surgery[J]. Crit Care,2011,15: R16.
[7] Parolari A,Pesce LL,Pacini D,et al. Risk factors for perioperative acute kidney injury after adult cardiac surgery: Role of perioperative management[J]. Ann Thorac Surg,2012,93:584-591.endprint
[8] Parikh CR,Mishra J,Thiessen-Philbrook H,et al. Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery[J]. Kidney Int,2006,70:199-203.
[9] Zhang Z,Lu B,Sheng X,et al. Cystatin C in prediction of acute kidney injury:A systemic review and meta-analysis[J]. Am J Kidney Dis,2011,58:356-365.
[10] Patel UD,Garg AX,Krumholz HM,et al. Preoperative serum brain natriuretic peptide and risk of acute kidney injury after cardiac surgery[J]. Circulation,2012,125:1347-1355.
[11] Vanmassenhove J,Vanholder R,Nagler E,et al. Urinary and serum biomarkers for the diagnosis of acute kidney injury:An in-depth review of the literature[J]. Nephrol Dial Transplant,2013, 28:254-273.
[12] Bellomo R,Ronco C,Kellum JA,et al. Acute renal failure- definition,outcome measures,animal models,fluid therapy and information technology needs:the Second International Consensus Conference of the Acute Dialysis Quality Initiative(ADQI)Group[J]. Crit Care,2004,8:R204-R212.
[13] Zhang Z,Ni H. Normalized lactate load is associated with development of acute kidney injury in patients who underwent cardiopulmonary bypass surgery[J]. PLoS One,2015,10: e0120466.
[14] Prowle JR,Kirwan CJ,Bellomo R. Fluid management for the prevention and attenuation of acute kidney injury[J]. Nat Rev Nephrol,2014,10:37-47.
[15] Payen D,de Pont AC,Sakr Y,et al. A positive fluid balance is associated with a worse outcome in patients with acute renal failure[J]. Crit Care,2008,12:R74.
[16] Grams ME,Estrella MM,Coresh J,et al. Fluid balance, diuretic use,and mortality in acute kidney injury[J]. Clin J Am Soc Nephrol,2011,6:966-973.
[17] Prowle JR,Chua HR,Bagshaw SM,et al. Clinical review: Volume of fluid resuscitation and the incidence of acute kidney injury-a systematic review[J]. Crit Care,2012, 16:230.
[18] Cruz DN,Goh CY,Haase-Fielitz A,et al. Early biomarkers of renal injury[J]. Congest Heart Fail,2010,16(Suppl 1):S25-S31.
[19] Ichihara K,Saito K,Itoh Y. Sources of variation and reference intervals for serum cystatin C in a healthy Japanese adult population[J]. Clin Chem Lab Med,2007,45:1232-1236.
[20] Peralta CA,Katz R,Sarnak MJ,et al. Cystatin C identifies chronic kidney disease patients at higher risk for complications[J]. J Am Soc Nephrol,2011,22:147-155.endprint