不同炎性因子对重症急性胰腺炎的预测价值研究
张红松,冯 芳,付丽彬,齐 艳,蔡红燕
·论著·
不同炎性因子对重症急性胰腺炎的预测价值研究
张红松*,冯 芳,付丽彬,齐 艳,蔡红燕
目的探讨不同炎性因子对重症急性胰腺炎(SAP)的预测价值。方法本研究采用前瞻性观察性研究方法。选取于2014年6月—2016年10月收住兰州大学第二医院外科重症监护病房(SICU)的并发器官功能障碍的急性胰腺炎(AP)患者40例。入科48 h根据患者是否持续存在器官功能障碍,将患者分为中重症急性胰腺炎(MSAP)组27例和SAP组13例。比较两组患者入科时的肿瘤坏死因子α(TNF-α)、白介素1(IL-1)、白介素6(IL-6)、白介素8(IL-8)及白介素10(IL-10)水平,采用Spearman秩相关分析、Logistic回归分析筛选出能够预测SAP的炎性因子,绘制受试者工作特征(ROC)曲线并寻找其最佳截断点,比较其对SAP的预测价值。结果两组患者入住SICU时,TNF-α、IL-6水平比较,差异均有统计学意义(P<0.05);IL-1、IL-8、IL-10水平比较,差异均无统计学意义(P>0.05)。Spearman秩相关分析显示,SAP与TNF-α、IL-6呈正相关(rs值分别为0.539、0.557,P<0.05);与IL-1、IL-8、IL-10无相关性(rs值分别为0.303、0.284、-0.257,P>0.05)。Logistic回归分析结果显示,TNF-α、IL-6是SAP发生的影响因素〔OR(95%CI)分别为1.143(1.011,1.293)、1.084(1.014,1.158),P<0.05〕。TNF-α、IL-6预测SAP的ROC曲线下面积(AUC)分别为0.832(0.700,0.964)、0.843(0.684,1.000),均较好地预测了SAP的发生(P<0.05)。TNF-α、IL-6的截断点分别为141.7 pg/L、143.3 pg/L时预测SAP的灵敏度和特异度较高。结论收住ICU的AP患者早期检测血浆中TNF-α与IL-6的水平,与其他炎性因子相比,可早期预测SAP的发生,为尽早采取措施保护器官功能提供了理论依据。
重症急性胰腺炎;炎性因子;肿瘤坏死因子α;白细胞介素6;预测
张红松,冯芳,付丽彬,等.不同炎性因子对重症急性胰腺炎的预测价值研究[J].中国全科医学,2017,20(25):3127-3131.[www.chinagp.net]
ZHANG H S,FENG F,FU L B,et al.Predictive value of inflammatory cytokines in severe acute pancreatitis[J].Chinese General Practice,2017,20(25):3127-3131.
急性胰腺炎(acute pancreatitis,AP)发病急,病情多变,易并发多器官功能障碍综合征(multiple organ dysfunction syndrome,MODS),死亡率高,是普外科与重症医学科的研究热点[1-2]。随着对AP基础与临床研究的深入,结合国际上AP的分级和分类系统[3],中华医学会外科学分会胰腺外科学组颁布了《急性胰腺炎诊治指南(2014)》[4]。该指南根据器官功能障碍持续的时间是否>48 h将AP分为中重症急性胰腺炎(moderately severe acute pancreatitis,MSAP)和重症急性胰腺炎(severe acute pancreatitis,SAP)。二者的病理生理及预后截然不同[5],寻找合适的指标尽快区分MSAP与SAP对临床医生极其重要。本研究通过比较MSAP和SAP患者收住ICU时各炎性因子的水平,探讨不同炎性因子对SAP的预测价值,希望寻找到能够预测SAP的炎性因子,为尽早干预治疗提供依据。
1 对象与方法
1.1 研究对象 选取于2014年6月—2016年10月收住兰州大学第二医院外科重症监护病房(SICU)的并发器官功能障碍的AP患者40例。入科48 h根据患者是否持续存在器官功能障碍,将患者分为MSAP组27例和SAP组13例。纳入标准:MSAP符合AP的诊断标准[6],Ranson评分≥3分,急性生理学与慢性健康状况评分系统Ⅱ(APACHEⅡ)评分≥8分,急性胰腺炎严重程度床边指数(BISAP)评分≥3分,修正CT严重指数(MCTSI)评分≥4分,伴有一过性(≤48 h)的器官功能障碍。SAP符合AP的诊断标准[6],伴有持续性(>48 h)的器官功能障碍(单器官/多器官),改良Marshall评分≥2分,余标准同MSAP[7]。排除标准:(1)年龄<18岁或>70岁;(2)慢性胰腺炎急性发作者;(3)AP合并慢性器官功能障碍或衰竭;(4)入住SICU 48 h内死亡者;(5)患者或家属不同意者。本研究方案符合医学伦理学标准,经兰州大学第二医院伦理委员会审批通过,并获得患者和家属的知情同意。
1.2 研究方法 入选患者均给予禁食水、胃肠减压、抑制胰腺外分泌、抑制胰酶活性、抗感染、补液等治疗。同时根据器官功能障碍的程度选择性给予血管活性药物、机械辅助通气、持续血液净化、纠正凝血功能紊乱等支持治疗。所有患者入科后即刻采集静脉血5 ml,离心3 000 r/min,离心半径为10 cm。10 min后分离血浆置于-70 ℃冰箱以备检测。采用ELISA法测定肿瘤坏死因子α(TNF-α)、白介素1(IL-1)、白介素6(IL-6)、白介素8(IL-8)、白介素10(IL-10)。同时采集血标本行肝肾功能、电解质检测及动脉血气分析,计算APACHEⅡ评分,并判断患者是否有器官功能障碍及其程度。入科48 h根据患者是否持续存在器官功能障碍,将患者分为MSAP组与SAP组,比较两组患者入科时各炎性因子的水平。

2 结果
2.1 两组患者基线资料的比较 两组患者在入住SICU时,在性别、年龄、APACHEⅡ评分方面比较,差异均无统计学意义(P>0.05,见表1)。
2.2 两组患者炎性因子水平的比较 两组患者入住SICU时,TNF-α、IL-6水平比较,差异均有统计学意义(P<0.05);IL-1、IL-8、IL-10水平比较,差异均无统计学意义(P>0.05,见表2)。
2.3 炎性因子与SAP的相关性分析Spearman秩相关分析显示,SAP与TNF-α、IL-6呈正相关(rs值分别为0.539、0.557,P<0.05);与IL-1、IL-8、IL-10无相关性(rs值分别为0.303、0.284、-0.257,P>0.05)。
2.4SAP发生影响因素的Logistic回归分析 以是否发生SAP为因变量,以两组间有差异的炎性因子为自变量,进行Logistic回归分析。结果显示,TNF-α、IL-6是SAP发生的影响因素(P<0.05,见表3)。
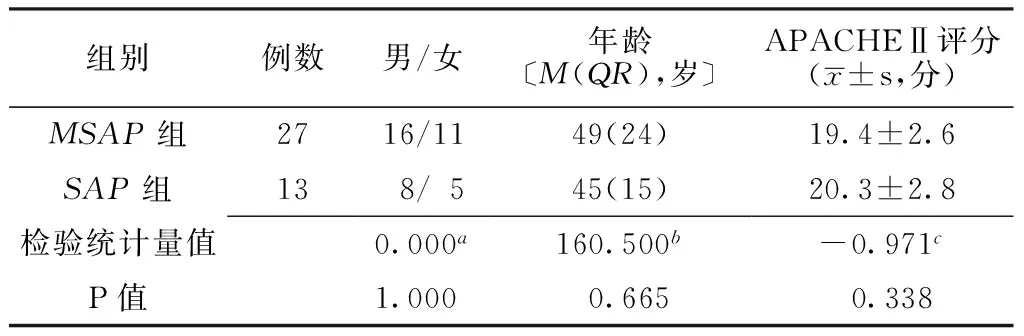
表1 两组患者基线资料的比较
注:MSAP=中重症急性胰腺炎,SAP=重症急性胰腺炎,APACHEⅡ=急性生理学与慢性健康状况评分系统Ⅱ;a为χ2值,b为U值,c为t值

Table2LevelsoffiveinflammatorycytokinesofMSAPgroupcomparedwiththoseofSAPgroup

组别例数TNF-αIL-1IL-6IL-8IL-10MSAP组27136.8±8.231.1±1.8124.3±14.399.6±14.860.3±4.8SAP组13147.4±8.132.2±1.6145.6±17.6107.5±10.157.9±4.5t值-3.840-1.884-4.084-1.7431.515P值0.0350.067<0.0010.0890.138
注:TNF-α=肿瘤坏死因子α,IL-1=白介素1,IL-6=白介素6,IL-8=白介素8,IL-10=白介素10
表3 SAP发生影响因素的Logistic回归分析
Table3 Logistic regression analysis of the inflammatory cytokines associated with SAP

炎性因子b值SEWaldχ2值P值OR(95%CI)TNF-α0.1340.0634.5410.0331.143(1.011,1.293)IL-60.0810.0345.6750.0171.084(1.014,1.158)
2.5 TNF-α、IL-6的ROC曲线 TNF-α、IL-6的ROC曲线下面积(AUC)分别为0.832(0.700,0.964)、0.843(0.684,1.000),均较好地预测了SAP的发生(P<0.05,见图1)。
2.6 TNF-α、IL-6预测SAP的最佳截断点分析 TNF-α、IL-6的最佳截断点分别为141.7 pg/L、143.3 pg/L,预测SAP的灵敏度和特异度较高(见表4)。

注:TNF-α=肿瘤坏死因子α,IL-6=白介素6,SAP=重症急性胰腺炎,ROC曲线=受试者工作特征曲线
图1 TNF-α、IL-6预测SAP的ROC曲线
Figure1 ROC curves of TNF-α and IL-6 in the prediction of SAP
表4 TNF-α、IL-6预测SAP的最佳截断点分析
Table4 Optimal cut-off value of TNF-α and IL-6 in the prediction of SAP

炎性因子截断点(pg/L)约登指数灵敏度(%)特异度(%)TNF-α141.70.54776.977.8IL-6143.30.73276.996.3
3 讨论
SAP是SICU常见的急危重症,占AP的15%~20%,因胰腺出血、坏死和自溶,出现胰酶消化自身组织,继而有强烈的局部与全身性爆发性炎性反应,胰腺血管受损栓塞,胰腺坏死,继发感染,多器官受损,除腹痛、腹膜刺激征等症状外,可出现循环障碍、高热、黄疸、少尿、腹胀、肠麻痹以及皮下瘀点、瘀斑[8-9],病死率高达10%~30%[10],合并MODS则病死率高达30%~50%[11]。近年来AP的基础研究有了新的认识,使临床处理与决策也发生了相应的变化。2014年中华医学会外科学分会胰腺外科学组也修订了2007版指南,推出了《急性胰腺炎诊治指南(2014)》[4]。该指南依据国际最新进展,将AP按照病情严重程度分为轻症急性胰腺炎(mild acute pancreatitis,MAP)、MSAP、SAP。MSAP与SAP的主要区别是器官功能障碍持续的时间是否>48 h,因此这两型在发病后入住ICU时不能区分。但如何早期预测AP的分型对临床把握病情、采取适宜的治疗措施及评估预后极为重要。故本研究以临床需求为出发点,探讨不同炎性因子对SAP的预测价值。
SAP发病机制是一个复杂的、多因素参与的病理生理过程,至今未完全阐明[12]。早期提出的“自身消化学说”[13]已不能全面阐明AP的发病机制及其复杂的病理生理过程。近年的研究提出了许多新学说。RINDERKNECHT[14]早期提出的SAP“白细胞过度激活”假说和后来提出的SAP是一种系统性全身炎性反应综合征(SIRS)[15]的概念均认为异常激活的胰酶在损伤胰腺的同时,也导致了炎性细胞中炎性因子的“瀑布级联反应”,加剧了促炎与抗炎细胞因子失衡,促发了全身过度炎性反应,并最终导致多脏器衰竭[16-18]。炎性因子是引起SAP发生SIRS的强效递质,但在细胞因子网络系统中,不同细胞因子促炎性反应的权重如何有待商榷。本研究结果显示:入住SICU时,SAP组的TNF-α与IL-6水平高于MSAP组,而IL-1、IL-8、IL-10水平两组无差异;Spearman秩相关分析结果显示,SAP与TNF-α、IL-6呈正相关,而与IL-1、IL-8、IL-10无相关性。因此本研究得出TNF-α、IL-6是促进SAP发生、发展的主要炎性递质的结论。
TNF-α由活化的单核细胞产生,是联系特异性免疫和炎性反应的重要因子,参与粒细胞的过度激活[19]。TNF-α诱导AP的可能机制为:(1)TNF-α可直接损伤胰管细胞,产生微血栓,导致腺泡缺血、出血、坏死、炎症、水肿;(2)TNF-α与胰酶协同参与炎性细胞的刺激与激活;(3)高水平的TNF-α使内皮黏连分子表达增强并聚集炎性细胞,促使粒细胞吞噬、脱颗粒、产生氧自由基和溶酶体酶、弹力蛋白酶等,导致细胞代谢紊乱及MODS;(4)TNF-α参与粒细胞过度激活,使炎性细胞和血管内皮细胞释放其他炎性递质,产生细胞因子网络效应,促成SIRS 加重胰腺损害[20]。IL-6主要由巨噬细胞、单核细胞释放,其诱导AP的机制为:(1)对血管内皮细胞及炎性细胞具有直接的激活和毒性作用;(2)诱导急性期蛋白的合成、放大全身炎性反应造成相关组织细胞的损害[21]。本研究Logistic回归分析结果显示,TNF-α、IL-6是SAP发生的影响因素。TNF-α、IL-6的AUC分别为0.832(0.700,0.964)、0.843(0.684,1.000);当二者截断点分别为141.7 pg/L、143.3 pg/L时,有较高的灵敏度与特异度。说明TNF-α与IL-6是早期预测SAP、评价AP严重程度的最有用的炎性因子,可以根据TNF-α与IL-6水平为患者制定合理的诊疗方案。
综上所述,收住ICU的AP患者早期检测血浆中TNF-α与IL-6的水平,与其他炎性因子相比,可早期预测SAP的发生,为尽早采取措施保护器官功能提供了理论依据。但是,本研究样本量较少,结论仍需多中心、大样本的研究证实。
作者贡献:张红松负责试验设计、撰写论文;冯芳、付丽彬负责试验实施、评估、资料收集;齐艳、蔡红燕负责质量控制。
本文无利益冲突。
[1]BEGER H G,RAU B M.Severe acute pancreatitis:clinical course and management[J].Word J Gastroenterol,2007,13(38):5043-5051.DOI:10.3748/wjg.v13.i38.5043.
[2]尚志荣,刘海中.糖尿病酮症酸中毒合并急性胰腺炎一例[J].实用心脑肺血管病杂志,2015,23(2):119-120.DOI:10.3969/j.issn.1008-5971.2015.02.043. SHANG Z R,LIU H Z.Diabetic ketoacidosis complicated with acute pancreatitis:a case report[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2015,23(2):119-120.DOI:10.3969/j.issn.1008-5971.2015.02.043.
[3]BANKS P A,BOLLEN T L,DERVENIS C,et al.Classification of acute pancreatitis——2012:revision of the Atlanta classification and definitions by international consensus[J].Gut,2013,62(1):102-111.DOI:10.1136/gutjnl-2012-302779.
[4]中华医学会外科学分会胰腺外科学组.急性胰腺炎诊治指南(2014)[J].中国实用外科杂志,2015,35(1):4-7. Pancreatic Surgery Group,Chinese Society of Surgery,Chinese Medical Association.Guidelines for diagnosis and treatment of acute pancreatitis(2014)[J].Chinese Journal of Practical Surgery,2015,35(1):4-7.
[5]VEGE SS,GARDNER T B,ChARI S T,et al.Low mortality and high morbidity in severe acute pancreatitis without organ failure:a case for revising the Atlanta classification to include "moderately severe acute pancreatitis"[J].Am J Gastroenterol,2009,104(3):710-715.
[6]SAGHAFI O.Comparative evaluation of the modified CT severity index and CT severity index in assessing severity of acute pancreatitis[J].Ajr American Journal of Roentgenology,2011,197(2):386-392.DOI:10.2214/AJR.09.4025.
[7]中华医学会消化病学分会胰腺疾病学组.中国急性胰腺炎诊治指南(2013年,上海)[J].中华消化杂志,2013,29(4):656-660.DOI:10.3760/cma.j.issn.0254-1432.2013.04.001. Pancreas Study Group,Chinese Society of Gastroenterology,Chinese Medical Association.Guidelines for diagnosis and treatment of acute pancreatitis in China (2013,Shanghai) [J].Chinese Journal of Digestion,2013,29(4):656-660.DOI:10.3760/cma.j.issn.0254-1432.2013.04.001.
[8]KE L,NI H B,TONG Z H,et al.Intra-abdominal pressure and abdominal perfusion pressure:which is a better marker of severity in patients with severe acute pancreatitis[J].J Gastrointest Surg,2011,15( 8) :1426 -1432.DOI:10.1007/s11605-011-1553-3.
[9]中华外科学会胰腺外科学组.重症急性胰腺炎诊治指南[J].中华外科杂志,2007,45(11):727-729.DOI:10.3760/j.issn:0529-5815.2007.11.004. Group of Pancreas Surgery,Chinese Society of Surgery,Chinese Medical Association.The guideline of diagnosis and treatment of severe acute pancreatitis[J].Chinese Journal of Surgery,2007,45(11):727-729.DOI:10.3760/j.issn:0529-5815.2007.11.004.
[10]李道伟,何丹,董齐.胰腺坏死程度对急性胰腺炎预后的影响[J].中华临床医师杂志:电子版,2012,6(4):171-172. LI D W,HE D,DONG Q.The effect of pancreatic necrosis on the prognosis of acute pancreatitis[J].Chinese Journal of Clinicians:Electronic Edition,2012,6( 4) :171-172.
[11]SWAROOP V S,CHARI S T,CLAIN J E.Severe acute pancreatitis[J].JAMA,2004,291(23):2865-2868.
[12]张延龄.重新认识急性胰腺炎发病机制的意义[J].中国实用外科杂志,2003,23(1):29-30.DOI:10.3321/j.issn:1005-2208.2003.01.011. ZHANG Y L.Importance of reunderstanding the pathogenetic mechanism of acute pancreatitis[J].Chinese Journal of Practical Surgery,2003,23(1):29-30.DOI:10.3321/j.issn:1005-2208.2003.01.011.
[13]陈其奎.急性胰腺炎的病因和发病机制[J].现代消化及介入诊疗,2007,12(3):160-162.DOI:10.3969/j.issn.1672-2159.2007.03.006. CHEN Q K.Etiology and pathogenesis of acute pancreatitis[J].Modern Digestion & Intervention,2007,12(3):160-162.DOI:10.3969/j.issn.1672-2159.2007.03.006.
[14]RINDERKNECHT H.Fatal pancreatitis,a consequence of excessive leukocyte stimulation?[J].Int J Pancreatol,1988,3(2):105-112.
[15]GLOOR B,SCHMIDTMANN A B,WOMI M,et al.Pancreatic sepsis:prevention and therapy[J].Best Pract Res Clin Gastroenterol,2002,16(3):379-390.DOI:10.1053/bega.2002.0313.
[16]肖菲,江丽丹,郝金斗.血清降钙素原测定在儿童全身炎症反应综合征的临床应用价值[J].安徽医学,2015,36(9):1092-1094.DOI:10.3969/j.issn.1000-0399.2015.09.014. XIAO F,JIANG L D,HAO J D,et al.Clinical value of procalcitonin in treatment of systematic inflammatory response syndrome among children[J].Anhui Medical Journal,2015,36(9):1092-1094.DOI:10.3969/j.issn.1000-0399.2015.09.014.
[17]胡升安,项和平,高明,等.α-黑色素细胞刺激素胰蛋白酶原激活肽白介素-6检测评估急性胰腺炎病情严重程度的价值[J].安徽医学,2017,38(3):284-287.DOI:10.3969/j.issn.1000-0399.2015.09.014. HU S A,XIANG H P,GAO M,et al.Clinical value of procalcitonin in treatment of systematic inflammatory response syndrome among children[J].Anhui Medical Journal,2017,38(3):284-287.DOI:10.3969/j.issn.1000-0399.2015.09.014.
[18]PETROV M S,SHANBHAG S,CHAKRABORTY M,et al.Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis[J].Gastroenterology,2010,139(3):813-820.DOI:10.1053/j.gastro.2010.06.010.
[19]YAMASHITA A C,TOMISAWA N.Membrane materials for blood purification in critical care [J].Contrib Nephrol,2010,166(166):112-118.
[20]徐军,张梅,刘学民,等.TNF-α基因表达在大鼠急性重症胰腺炎肺损伤中的作用[J].西安交通大学学报(医学版),2004,25(4):387-392.DOI:10.3969/j.issn.1671-8259.2004.04.024. XU J,ZHANG M,LIU X M,et al.Intrapulmonary expression of TNF-α gene in rats with acute severe pancreatitis[J].Journal of Xi′an Jiaotong University(Medical Sciences),2004,25(4):387-392.DOI:10.3969/j.issn.1671-8259.2004.04.024.
[21]OKAJIMA K,HARADA N,SAKURAI G,et al.Rapid assay for plasma soluble E-selectin predicts the development of acute respiratory distress syndrome in patients with systemic inflammatory response syndrome[J].Transl Res,2006,148(6):295-300.
(本文编辑:闫行敏)
PredictiveValueofInflammatoryCytokinesinSevereAcutePancreatitis
ZHANGHong-song*,FENGFang,FULi-bin,QIYan,CAIHong-yan
SICU,LanzhouUniversitySecondHospital,Lanzhou730030,China
*Correspondingauthor:ZHANGHong-song,Chiefphysician,Associateprofessor;E-mail:jijiuyish@163.com
ObjectiveTo investigate the predictive value of inflammatory cytokines in severe acute pancreatitis(SAP).MethodsA prospective observational study was conducted in Lanzhou University Second Hospital.The participants were 40 cases of acute pancreatitis(AP) with organ dysfunction admitted in the Surgical Intensive Care Unit(SICU) of the hospital from June 2014 to October 2016.Of them,27 cases with organ dysfunction within 48 h after SICU admission were assigned to the moderate to severe acute pancreatitis (MSAP) group,and other 13 cases with organ dysfunction more than 48 h after SICU admission were assigned to the severe acute pancreatitis(SAP) group.We compared the concentrations of tumor necrosis factor-alpha (TNF-α),interleukin 1 (IL-1),interleukin 6 (IL-6),interleukin 8 (IL-8) and interleukin 10 (IL-10) measured on SICU admission between the groups.We selected the inflammatory cytokines associated with SAP from the above inflammatory cytokines by using analyses with Spearman′s rank correlation and Logistic regression models and compared the predictive value of them in SAP based on analyzing their ROC curves and cut-off values for the prediction of SAP.ResultsThe levels of TNF-α and IL-6 measured on SICU admission differed significantly between the groups(P<0.05),while those of IL-1,IL-8 and IL-10 did not(P>0.05).Analysis with Spearman′s rank correlation found that,levels of TNF-α had a positive correlation with SAP(rs=0.539,P<0.05);levels of IL-6 were positively correlated with SAP(rs=0.557,P<0.05);but no correlation was found between SAP and levels of IL-1,IL-8 and IL-10(rs=0.303,P>0.05;rs=0.284,P>0.05;rs=-0.257,P>0.05,respectively).The analysis with Logistic regression models demonstrated that,levels of TNF-α and IL-6 were found to have predictive value for SAP 〔OR=1.143,95%CI(1.011,1.293),P<0.05;OR=1.084,95%CI(1.014,1.158),P<0.05,respectively〕.Both TNF-α and IL-6 had good performance in the prediction of SAP proved by the area under the ROC curve (AUC) 〔0.832(0.700,0.964),P<0.05;0.843(0.684,1.000),P<0.05,respectively〕.For predicting SAP,the optimal cut-off value of TNF-α and IL-6 was 141.7 pg/L,143.3 pg/L,respectively with maximized sensitivity and specificity.ConclusionThe levels of plasma TNF-α and IL-6 measured early in ICU patients with AP have values in the prediction of SAP,while those of other inflammatory cytokines do not,which provides a theoretical basis for taking measures to protect the patients′ organ function as soon as possible.
Severe acute pancreatitis;Inflammatory cytokines;Tumor necrosis factor-α;Interleukin-6;Forecasting
甘肃省兰州市城关区科技计划项目(2015-3-7)
R 576.1
A
10.3969/j.issn.1007-9572.2017.25.013
2017-02-10;
2017-05-25)
730030 甘肃省兰州市,兰州大学第二医院重症医学一科
*通信作者:张红松,主任医师,副教授;E-mail:jijiuyish@163.com

