表现为间质性肺炎的肺腺癌15例临床分析
李建东,郝淑玲,王 斐
(陆军总医院呼吸科,北京 100700;*通讯作者,E-mail:ljdzy@hotmail.com)
表现为间质性肺炎的肺腺癌15例临床分析
李建东*,郝淑玲,王 斐
(陆军总医院呼吸科,北京 100700;*通讯作者,E-mail:ljdzy@hotmail.com)
目的 提高对肺腺癌临床表现及影像学多样性的认识,减少误诊。 方法 回顾性分析2012-07~2015-05收治的15例表现为肺间质性肺炎的肺腺癌临床资料及诊治经过,总结其临床特点、影像学表现及与间质性肺炎的差异,提出诊断线索和方法。 结果 15例患者中,男8例,女7例,年龄在44-78岁,平均(56.8±8.2)岁。临床表现为不同程度咳嗽、咳痰、进行性呼吸困难,6例患者发热,体温在37.8-38.8 ℃。13例肺部可闻及爆裂音。14例患者部分肿瘤标志物增高。15例肺功能弥散功能下降,14例患者血气分析为Ⅰ型呼吸衰竭。胸部CT表现为磨玻璃影,实变、小结节影,网格影。15例患者经抗感染治疗无效。12例患者进行性呼吸困难给予甲强龙治疗,咳嗽,呼吸困难好转,肺部爆裂音减少,动脉血氧分压上升至70-80 mmHg,但胸部CT无明显吸收。经皮肺活检病理诊断为肺腺癌。5例患者拒绝治疗出院,随访3例死亡,生存期2-3个月,2例失访。8例患者给予化疗(GP,DP方案),患者病情好转,后随访8例患者死亡,生存期8-10月。2例EGFR基因突变患者给予化疗(GP方案)及吉非替尼治疗,患者病情明显好转,肺部病变明显吸收,随访3年,病情稳定。 结论 肺腺癌临床、影像学无特异性,表现形式呈多样性,尤其是部分肺腺癌临床与影像学类似间质性肺炎,易造成误诊。提高对这类型表现的肺腺癌的认识,在临床诊疗过程中发现肺癌的诊断线索,积极行经皮肺活检病理检查,明确诊断。
肺腺癌; 间质性肺炎; 胸部CT
近年来肺腺癌的发病率显著增高[1],肺腺癌临床表现无特征性,多以咳嗽起病,可有痰中带血,症状呈多样性,影像学表现复杂,大部分表现为团块影、结节影,部分肺癌影像学表现类似肺炎。近年来我科收治15例以咳嗽、咳痰、进行性呼吸困难为首发症状,双肺弥漫性间质性病变为表现的肺腺癌病例,给予糖皮质激素治疗,呼吸困难明显好转,临床表现为间质性肺炎,后经皮肺活检诊断为肺腺癌。现报道如下并结合文献进行复习,提高对肺腺癌临床表现多样性的认识,减少误诊率。
1 材料与方法
1.1 研究对象
选取2012-07~2015-05入住我院呼吸科经皮肺活检明确诊断为肺腺癌患者15例,其中男8例,女7例,年龄在47-77岁,平均(57.5±8.2)岁。吸烟5例。病程2周至3月,平均(1.69±0.984)月。15例患者既往健康13例,慢性阻塞性肺病2例,均无间质性肺疾病病史。
1.2 诊断标准
结合患者病史、临床症状、体征,实验室检查及胸部X线表现,经皮肺活检组织病理学诊断。
1.3 方法
回顾性总结15例患者的病史、症状体征、实验室检查、胸部X线表现、组织病理结果及诊疗过程,并随访。
2 结果
2.1 临床表现
15例患者中13例表现为不同程度咳嗽、咳痰,均无咳大量泡沫痰,2例患者干咳,15例患者均表现为进行性呼吸困难,10例患者活动受限,2例患者需无创呼吸机治疗。6例患者发热,体温在37.8-38.8 ℃。13例患者肺部可闻及爆裂音。
2.2 实验室及肺功能检查
15例患者中12例血常规正常,2例轻度轻度贫血,血红蛋白在90-110 g/L。10例患者肝肾功能正常,2例患者谷丙转氨酶增高,为50-105 U/L,3例患者白蛋白减低,为30-34 g/L。6例患者血沉增快,为30-55 mm/h。12例患者CEA增高,在5.9-80.7 ng/ml(参考值为0-4.6 ng/ml),6例患者CA125增高,65.9-116.6 U/ml(参考值为0-35 U/ml),1例患者CA15-3增高,为42.2 U/ml(参考值为0-25 U/ml),7例CA19-9增高,65.4-746.6 U/ml(参考值为0-39 U/ml),6例CA724增高,6.0-61.4 U/ml(参考值为0-5.3 U/ml),6例NSE增高,17.5-27.2 U/ml(参考值为0-15.2 U/ml),仅1例患者肿瘤标志物正常。
15例患者血气分析检查,14例为Ⅰ型呼吸衰竭,动脉血氧分压40-58 mmHg,1例动脉血氧分压87 mmHg。
肺功能检查15例患者中13例限制性通气功能障碍,2例混合型通气功能障碍,15例患者均一氧化碳弥散功能减低,一氧化碳弥散量占预计值百分比为32%-75%。
2.3 胸部CT
15例患者胸部CT表现为双肺弥漫性斑片、实变影,磨玻璃影,小结节影,网格影。胸部CT表现为双肺多发性,非对称磨玻璃影12例,双肺斑片、实变影伴支气管充气征6例,双肺小结节影4例,网格影4例,几种征象常共存(见图1,2)。图1为52岁女性患者,入院时胸部CT:双肺散在分布直径小于1.0 cm结节,双上肺明显,双肺上叶及右肺中下叶见斑片、实变影,支气管充气征(见图 1A-C)。患者化疗、吉非替尼治疗1年后胸部CT:双肺多发淡薄小结节影,右肺及左肺上叶见弥漫性斑点及条片影,局部呈磨玻璃密度改变(见图 1D-F)。图2为59岁女性,入院时胸部CT:双肺多发性磨玻璃影,右肺为著。
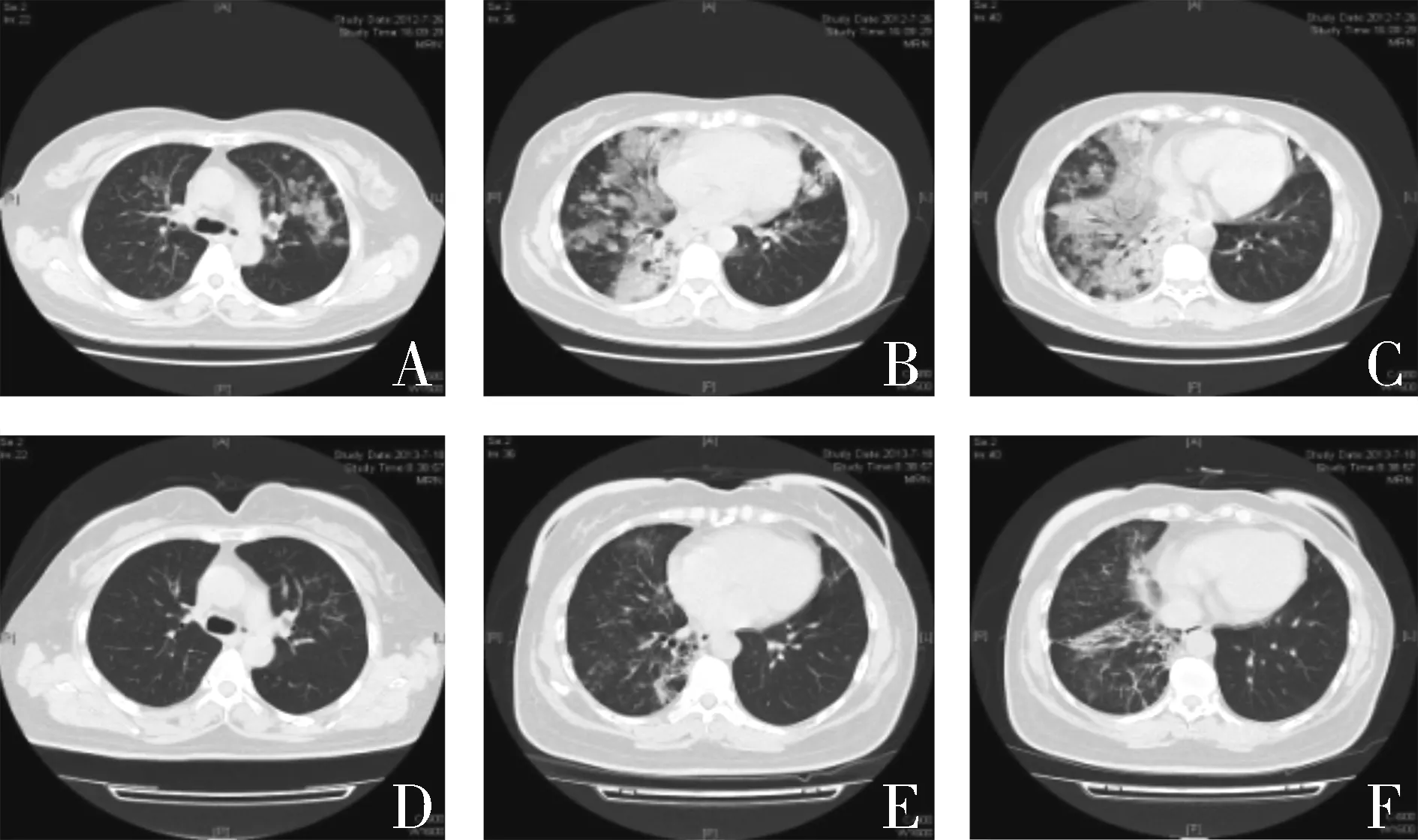
A-C.入院时胸部CT,双肺散在分布直径小于1.0 cm结节,双上肺明显;双肺上叶及右肺中下叶见斑片、实变影,右肺为著,内见支气管充气征;D-F.患者化疗、吉非替尼治疗1年后胸部CT,双肺多发淡薄小结节影;右肺及左肺上叶见弥漫性斑点及条片影,局部呈磨玻璃密度改变图1 52岁女性患者胸部CT结果Figure 1 Chest computed tomography finding of a 52-year-old female patient
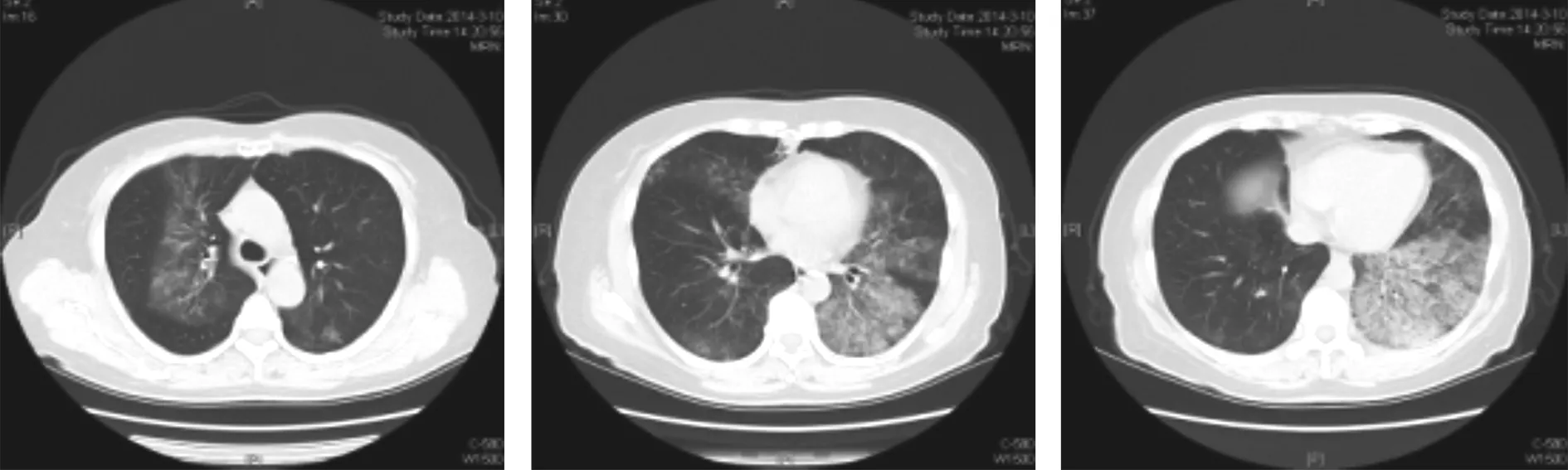
双肺多发性磨玻璃影,右肺为著图2 59岁女性患者入院时胸部CT结果Figure 2 Chest computed tomography finding of a 59 year-old female patient
2.4 病理
15例患者均经皮肺活检组织病理检查为肺腺癌(见图3,4),其中7例呈贴壁生长,4例呈乳头状生长,4例呈部分贴壁,乳头样生长。11例患者行EGFR基因检测,2例exon21突变。
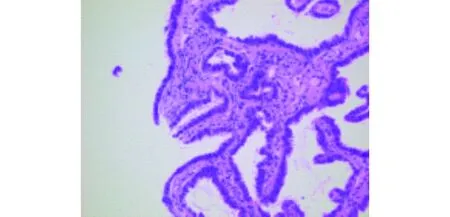
肺腺癌,贴壁型生长图3 图1患者经皮肺活检病理结果Figure 3 Histopathological finding of figure 1 patient obtained from percutaneous lung biopsy
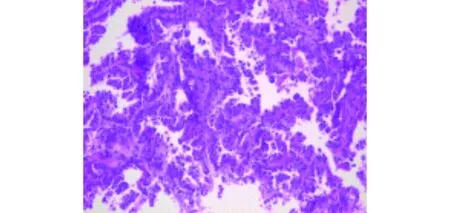
肺腺癌,贴壁型生长图4 图2患者经皮肺活检病理结果Figure 4 Histopathological finding of figure 2 patient obtained from percutaneous lung biopsy
2.5 治疗经过
15例患者住院后均给予广谱抗菌药物抗感染治疗,12例患者因呼吸困难明显,给予甲强龙治疗(甲强龙80 mg/d,后逐渐减量,总剂量在1 320-1 600 mg),2例无创呼吸机治疗,经甲强龙治疗后,患者体温正常,咳嗽、咳痰、呼吸困难好转,双肺爆裂音减少,复查血气分析血氧分压上升70-80 mmHg,但复查胸部CT病灶无明显吸收。15例患者经皮肺活检诊断为肺腺癌。2.6 转归
15例患者经病理诊断明确后,5例患者拒绝治疗出院,随访3例死亡,生存期2-3个月,2例失访。8例患者给予化疗(GP方案,盐酸吉西他滨1 250 mg/m2,d1,d8,静脉滴注;顺铂75 mg/m2,d1,静脉滴注;DP方案,多西他塞75 mg/m2,d1,静脉滴注;卡铂300 mg/m2,d1,静脉滴注),患者病情好转,后随访8例患者均死亡,生存期8-10月。2例EGFR基因突变患者给予化疗(GP方案)及吉非替尼(250 mg/d,口服)治疗,患者病情明显好转,肺部病变明显吸收,随访3年,病情稳定。
3 讨论
肺癌是世界上发病率和死亡率最高的恶性肿瘤之一,近年来肺腺癌已成为最常见的组织类型,目前肺腺癌占肺癌的46.5%[2]。肺腺癌起源于支气管黏膜腺,部分起源于Clara细胞,Ⅱ型肺泡上皮细胞,多见于周围型肺癌。肺腺癌无特异性症状、体征及胸部X线特征,其临床表现及影像学呈多样性,极易误诊。
本组15例患者以咳嗽、进行性呼吸困难起病,多数肺部可闻及爆裂音,胸部CT表现为磨玻璃、实变、小结节影及网格影,抗感染治疗无效,糖皮质激素治疗呼吸困难可缓解,临床过程类似间质性肺炎,后经皮肺活检诊断肺腺癌。
本组患者具有以下特点:①年龄在47-77岁,平均(57.5±8.2)岁,男 ∶女为1.14 ∶1。②均表现咳嗽、进行性呼吸困难,近半数患者发热,为轻中度发热,多数患者(86.7%,13/15)肺部均可闻及爆裂音。患者均无大量泡沫痰。③胸部CT表现为双肺磨玻璃影、实变影、多发性小结节影、网格影,几个征象多共存。④大部分患者(93.3%,14/15)出现Ⅰ型呼吸衰竭。⑤肺一氧化碳弥散功能减低。⑥多数患者(93.3%,14/15)一种或多种肿瘤标志物增高。⑦病理均为肺腺癌,为贴壁或乳头型生长,或两者兼有之。
本组患者虽然临床过程及影像学表现酷似间质性肺炎,但可发现肺癌的诊断线索。①多数患者可有多种肿瘤标志物增高。②糖皮质激素治疗虽可减轻患者呼吸困难症状,但肺部病灶无明显吸收。③胸部CT多表现为磨玻璃影、实变影、小结节影、网格影等几种征象共存,双侧不对称与间质性肺炎略有不同,结节影较间质性肺炎多见[3-7]。④经皮肺活检是明确诊断简便、安全的手段。
慢性间质性肺疾病合并肺癌的发生率较高[8],本组患者表现与慢性间质肺病合并肺癌不同。其原因为:①慢性间质性肺炎既往有相关的病史,如结缔组织疾病史,缓慢的进行性呼吸困难,胸部CT表现为网格、蜂窝阴影,双肺胸膜下病变为主,与本组患者表现不符。②慢性间质性肺炎多缓慢进展,在弥漫性间质疾病基础出现团块、结节影[9],与本组患者起病即为磨玻璃、实变、结节影等不同。③慢性间质性肺炎合并肺癌,肿瘤病理类型为腺癌、鳞癌、小细胞,呈多样性,而本组患者均为腺癌,可能与肺腺癌的生长特性有关,而呈现为间质性肺炎表现。
本组患者表现与急性间质性肺炎有差别。急性间质性肺炎病因不明,平均发病年龄在50-55岁,表现为发热、头痛、肌痛等流感样症状,咳嗽,进行性加重的呼吸困难,迅速发展为Ⅰ型呼吸衰竭,大多数患者需要呼吸支持,糖皮质激素治疗效果差,死亡率达到70%[3,6,7]。本组患者病情进展相对缓慢,糖皮质激素治疗可缓解呼吸困难,但病灶无明显吸收,可能与肿瘤细胞刺激局部炎性水肿有关。患者近期死亡率不高,与急性间质性肺炎不同。
由此,我们推测,可能存在着一种类型的肺腺癌,具有与一般肺腺癌不同的生物学特性,其生长方式浸润肺间质,临床上表现为呼吸困难,肺部爆裂音,Ⅰ型呼吸衰竭,胸部CT表现为磨玻璃、实变、结节影、网格影,可能为肺腺癌的一种表型,表现了肺腺癌的异质性。但这需要进一步研究。
综上所述,肺腺癌临床表现、影像学无特异性,表现形式呈多样性,尤其是部分肺腺癌临床表现与影像学检查类似间质性肺炎,易造成临床医生误诊。提高对这类型表现的肺腺癌的认识,熟悉其临床、影像学表现形式及与间质性肺炎差异,在临床诊疗过程中发现肺癌的诊断线索,积极行经皮肺活检病理检查,明确诊断。
[1] Jemal A,Bray F,Center MM,etal.Global cancer statistics[J].CA Cancer J Clin,2011,61(2):69-90.
[2] Barsky SH,Cameron R,Osann KE,etal.Rising incidence of bronchioloalveolar lung carcinoma and its unique clinicopathologic feature[J].Cancer,1994,73(4):244-285.
[3] Vourlekis JS.Acute interstitial pneumonia[J].Clin Chest Med,2004,25:739-747.
[4] Avnon LS,Pikovsky O,Sion-Vardy N,etal.Acute interstitial pneumonia-hamman-rach syndrome:clinical characteristics and diagnostic and therapeutic consideration[J].Anesth Analg,2009,108:233-237.
[5] Ichikado K,Suga M,Muller NL,etal.Acute interstitial pneumonia:Comparison of hight-resolution computed tomography finging between survivors and nonsurvivors[J].Am J Respir Crit Care Med,2002,165:1551-1556.
[6] Suh GY,Kang EH,Chung MP,etal.Early intervention can improve clinical outcome of acute interstitial pneumonia[J].Chest,2006,129:753-761.
[7] Bonaccorsi A,CancellieriA,Chilosi M,etal.Acute interstitial pneumonia:report of Asries[J].Eur Reapir J,2003,21:187-191.
[8] Bouros D,Hatzakis K,Labrakis H,etal.Association of malignancy with disease causing interstitial pulmonary changes[J].Chest,2002,121(4):1278-1289.
[9] Fujita J,Yamadori I,Namihira H,etal.Increased intensity of lung infiltrates at the side of lung cancer in patients with lung cancer associated with pulmonary fibrosis[J].Lung Cancer,1999,26(3):169-174.
Clinical analysis of 15 cases of lung adenocarcinoma presenting as interstitial pneumonia
LI Jiandong*,HAO Shuling,WANG Fei
(DepartmentofRespiration,PLAArmyGeneralHospital,Beijing100700,China;*Correspondingauthor,E-mail:ljdzy@hotmail.com)
ObjectiveTo improve the understanding of the clinical manifestation and radiologic imaging diversity of lung adenocarcinoma and reduce misdiagnosis.MethodsClinical and imaging data of 15 cases of lung adenocarcinoma presenting as interstitial pneumonia were retrospectively analyzed.The data were collected form Army General Hospital from July 2012 to May 2015.ResultsAll the 15 cases(8 males and 7 females,aged 47-77 years old,mean 57.5±8.2 years old) had the symptoms of cough,expectoration and dyspnea in varying degrees.Six cases of them had fever(37.8-38.8 ℃).Coarse crackles was heard in one or two lung fields of 13 patients.Blood tumor markers were elevated in 13 patients.Monoxide diffusion function was reduced in 15 patients.Blood gas analysis presented typeⅠ respiratory failure in 14 patients.Chest computed tomography showed ground glass opacities,consolidation with air bronchograms,small nodules shadows and reticulation shadow in two lung fields.The patients all were treated with broad-spectrum antibiotics and the symptoms were not improved.Among 15 patients,12 patients with progressive dyspnea received corticosteroid therapy,and then the dyspnea of the patients was improved and the crackles of lung was reduced.Arterial oxygen partial pressure of the patients raised to 70-80 mmHg,but the pulmonary lesion of chest CT scan was not absorbed.The patients all were diagnosed as lung adenocarcinoma by percutaneous lung biopsy.Five patients refused chemotherapy and discharged.Three patients died after 2-3 months from the onset and two patients were lost for follow up.Eight patients received chemotherapy and survived for 8-10 months.Two patients with EGFR gene mutation were treated with chemotherapy combined with epidermal growth factor receptor inhibitor-gefitinib and still survived after three-year follow-up.ConclusionClinical manifestation and imaging of lung adenocarcinoma are diverse and non-specific,and even some of them present as interstitial pneumonia.Clinicians must improve the understanding of the lung adenocarcinoma and obtain actively pathologic diagnosis by precutaneous lung biopsy.
lung adenocarcinoma; interstitial pneumonia; chest CT scan
李建东,男,1962-10生,硕士,副主任医师
2017-02-23
R734.2
A
1007-6611(2017)06-0571-04
10.13753/j.issn.1007-6611.2017.06.013