切口妊娠介入治疗的临床应用及预后分析
鲁景元,顾建平,徐文健,楼文胜,施万印,汪 涛,邵泽锋
(1. 南京医科大学附属南京医院介入科, 南京 210006; 2. 南京医科大学附属南京妇幼保健院介入科, 南京 210004)
·论著·
切口妊娠介入治疗的临床应用及预后分析
鲁景元1,2,顾建平1△,徐文健2,楼文胜1,施万印1,汪 涛1,邵泽锋1
(1. 南京医科大学附属南京医院介入科, 南京 210006; 2. 南京医科大学附属南京妇幼保健院介入科, 南京 210004)
目的:分析子宫动脉栓塞(uterine artery embolization,UAE)治疗切口妊娠(cesarean scar pregnancy, CSP)的临床价值及预后。方法: 选取2011年1月至2014年12月收治于南京医科大学附属南京妇幼保健院的确诊CSP患者492例,其中高危组283例、低危组209例。根据是否行UAE治疗,将高危组分为高危UAE组(UAE+腹腔镜组)167例,高危非UAE组(化疗+腹腔镜组)116例;将低危组分为低危UAE组(UAE+清宫组)113例,低危非UAE组(化疗+清宫组) 96例。分别比较术中出血、住院时间、血人绒毛膜促性腺激素(beta human chorionic gonadotropin,β-HCG)降至正常时间、月经复潮时间及住院费用的差异,并通过多因素回归分析预测CSP再发风险。结果: 高危UAE组在术中出血[(36.5±14.8) mLvs. (76.5±39.7) mL)]、住院时间[(5.9±0.9) dvs.(9.6±1.3) d]、血β-HCG降至正常时间[(17.9±8.7) dvs. (28.7±10.1) d)]以及月经复潮时间[(18.1±1.6) dvs.(24.3±1.8) d]的比较中优于高危非UAE组,而低危UAE组在术中出血[(93.2±43.3) mLvs. (284.8±110.5) mL]、住院时间[(10.2±1.4) dvs.( 30.7±9.6) d]、血β-HCG降至正常时间[(50.1±17.6) dvs. (67.5±22.9) d)]以及月经复潮时间[(56.3±6.7) dvs.(65.9±9.3) d)]的比较中优于低危非UAE组,均P<0.05;高危UAE组住院费用[(20 140±1 520)元vs.(13 510±1 013)元)]高于高危非UAE组,而低危UAE组住院费用[(10 095±962)元vs. (3 890±457)元)]高于低危非UAE组,P<0.01;多因素Logistic回归分析结果显示,治疗方法是CSP再发风险的独立预测因素(OR2.407, 95%CI1.176~5.092,P<0.05),采用包含UAE在内的综合治疗方法可降低CSP再发风险。结论: UAE治疗CSP疗效迅速可靠、并发症少、恢复快、再发风险低,在有条件的医院,特别是针对有再次生育要求的CSP患者,应将含UAE治疗手段的综合治疗方案列为首选。
妊娠, 异位;子宫动脉栓塞术;明胶海绵, 吸收性;甲氨喋呤
切口妊娠(cesarean scar pregnancy, CSP)是指有剖宫产史的孕妇,此次妊娠胚胎在子宫前壁下段瘢痕处着床,属于一种特殊且危险的异位妊娠[1-2]。据相关文献报道,在至少有一次剖宫产术史的育龄妇女中的发生率为1 ∶1 800至1 ∶2 216[3-5],且随着剖宫产率的增加有逐年上升趋势[6]。CSP可导致子宫破裂、胎盘植入以及难以控制的子宫出血等严重并发症,一经确诊必须尽早终止妊娠[7-8]。目前CSP的治疗方法主要有:全身及病灶局部化疗、清宫术、经腹或腹腔镜下子宫下段病灶切除术、子宫切除术以及子宫动脉栓塞术(uterine artery embolization,UAE)等,在临床上尚未形成统一方案,其中,UAE在CSP治疗中的作用正逐步被广大临床工作者所重视[9]。
1 资料与方法
1.1 研究对象
对2011年1月至2014年12月收治于南京医科大学附属南京妇幼保健院妇科病房的确诊CSP患者492例,根据停经时间及辅助检查指标将492例患者分为高危组283例、低危组209例。分组标准:若同时满足孕周<8周、孕囊与膀胱间子宫肌层厚度>2 mm、血人绒毛膜促性腺激素(beta human chorionic gonadotropin,β-HCG)<5 000 IU/L则归为低危组;孕周≥8周、孕囊与膀胱间子宫肌层厚度≤2 mm、血β-HCG≥5 000 IU/L,凡满足如上任何一项则纳入高危组。南京医科大学附属南京妇幼保健院所收治的CSP患者均采用综合治疗,高危组和低危组处理方案不同。根据是否行UAE,再将高危组分为高危UAE组(即UAE+腹腔镜组),共167例;高危非UAE组(即化疗+腹腔镜组),共116例。将低危组分为低危UAE组(即UAE+清宫组),共113例;低危非UAE组(即化疗+清宫组),共96例。
一般资料比较,分别比较高危UAE组与高危非UAE组、低危UAE组与低危非UAE组,各组在年龄、停经时间、距前次剖宫产时间、治疗前血β-HCG值以及孕囊与膀胱间子宫肌层厚度方面差异均无统计学意义(P>0.05), 见表1。
表1 高危UAE组与高危非UAE组、低危UAE组与低危UAE组一般资料比较(±s)
table1 Comparison of general data between high-risk UAE group and high-risk non UAE group and between low-risk UAE group and low-risk non UAE group (±s)
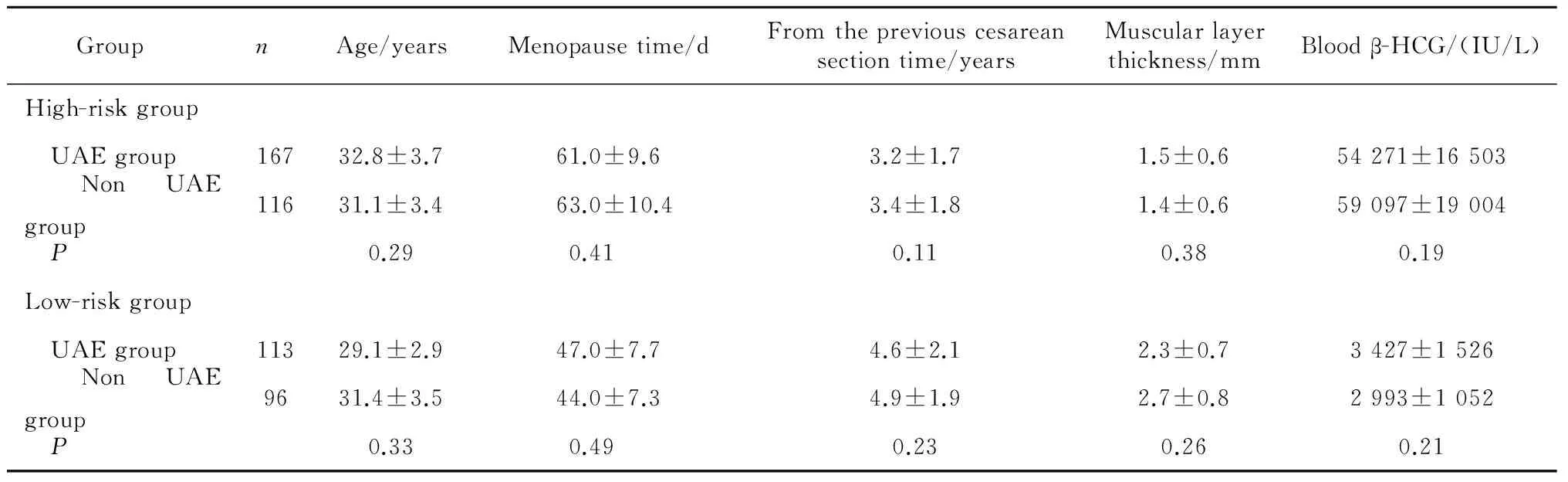
表1 高危UAE组与高危非UAE组、低危UAE组与低危UAE组一般资料比较(±s)
GroupnAge/yearsMenopausetime/dFromthepreviouscesareansectiontime/yearsMuscularlayerthickness/mmBloodβ-HCG/(IU/L)High-riskgroup UAEgroup16732.8±3.761.0±9.63.2±1.71.5±0.654271±16503 NonUAEgroup11631.1±3.463.0±10.43.4±1.81.4±0.659097±19004 P0.290.410.110.380.19Low-riskgroup UAEgroup11329.1±2.947.0±7.74.6±2.12.3±0.73427±1526 NonUAEgroup9631.4±3.544.0±7.34.9±1.92.7±0.82993±1052 P0.330.490.230.260.21
UAE,uterine artery embolization;β-HCG,beta human chorionic gonadotropin.
1.2 切口妊娠的诊断
CSP的确诊主要依据停经史、血β-HCG符合妊娠早期改变、影像学证据,其中超声为确诊CSP的重要辅助检查手段。以Godin等[10]于1997年提出的超生诊断标准为基础,并做了适当改进及完善,即:(1)宫腔及宫颈管内未探及妊娠囊;(2)妊娠囊或混合性包块位于子宫峡部前壁宫颈内口水平处或既往剖宫产瘢痕处;(3)妊娠囊或包块与膀胱之间,子宫下段前壁肌层变薄或连续性中断;(4)彩色多普勒血流成像在妊娠囊滋养层周边探及明显的环状血流信号,脉冲多普勒示高速(峰值流速>20 cm/s)低阻(搏动指数<1)血流图,与正常早期妊娠血流图相似;(5)附件区未探及包块,直肠子宫陷凹无游离液性暗区(CSP破裂除外)。
1.3 方法
1.3.1 高危组治疗方案
高危UAE组,行双侧UAE,术中影像见图1。采用改良Seldinger技术穿刺右侧股动脉,置入5 F(1 F=0.33 mm)导管鞘, 插入5 F子宫动脉导管, 行双侧子宫动脉超选择性插管, 术中经双侧子宫动脉灌注甲氨蝶呤(methotrexate,MTX)各50 mg,再用直径1 000~1 400 μm明胶海绵颗粒栓塞, 经造影证实子宫动脉闭塞,血供阻断。术后3 d行腹腔镜下子宫下段病灶切除+修补术。腹腔镜术后监测血β-HCG,两天1次,若下降至100 IU/L以下,准予出院,嘱院外随访。若术后1周仍未下降至100 IU/L以下,给予MTX 100 mg单次肌肉注射(肌注),直到下降至100 IU/L以下予以出院,期间可重复追加MTX 100 mg肌注,间隔时间为1周。本组有14人追加MTX肌注。
高危非UAE组,予米非司酮50 mg口服,每天2次, 连服3 d,加单次MTX 100 mg肌注,治疗期间检测肝功能,并监测血β-HCG下降至500 IU/L以下,行腹腔镜下子宫下段病灶切除+修补术。腹腔镜术后监测血β-HCG,两天1次,若下降至100 IU/L以下,准予出院,嘱院外随访。若术后1周仍未下降至100 IU/L以下,给予MTX 100 mg单次肌注,直到下降至100 IU/L以下予以出院,期间可重复追加MTX 100 mg肌注,间隔时间为1周。本组有17人追加MTX肌注。
A,before embolism,lower uterine segment vascular hyperplasia, and placental lobule vascular develop(arrow show placental cotyledon vessels);B, after embolism,distal uterine artery blocked.
图1 高危子宫动脉栓塞组切口妊娠患者子宫动脉栓塞前、后影像资料
Figure1 Image of high-risk uterine artery embolization group of patients with cesarean scar pregnancy before and after uterine artery embolism
1.3.2 低危组治疗方案
低危UAE组,行双侧UAE,术中影像见图2。术中经双侧子宫动脉灌注MTX各50 mg,栓塞术后监测血β-HCG下降至500 IU/L以下,在B超监视下行清宫术。清宫术后监测血β-HCG,两天 1次,若下降至100 IU/L以下,准予出院,嘱院外随访。若术后1周仍未下降至100 IU/L以下,给予MTX 100 mg单次肌注,直到下降至100 IU/L以下予以出院,期间可重复追加MTX 100 mg肌注,间隔时间为一周。本组有16人追加MTX肌注。
低危非UAE组,予米非司酮50 mg口服,每天2次, 连服3 d,加单次MTX 100 mg肌注,治疗期间检测肝功能,并监测血β-HCG下降至500 IU/L以下,在B超监视下行清宫术。清宫术后监测血β-HCG,两天 1次,若下降至100IU/L以下,准予出院,嘱院外随访。若术后1周仍未下降至100 IU/L以下,给予MTX 100 mg单次肌注,直到下降至100 IU/L以下予以出院,期间可重复追加MTX 100 mg肌注,间隔时间为1周。本组有19人追加MTX肌注。
A, before embolism,lower uterine segment blood vessels associated with slight bleeding(arrow show lower uterine vessels bleeding);B, after embolism,uterine artery and its branches blocked.
图2 低危子宫动脉栓塞组切口妊娠患者子宫动脉栓塞前后影像资料
Figure2 Image of low-risk uterine artery embolization group of patients with cesarean scar pregnancy before and after uterine artery embolism
1.3.3 观测指标
比较高危UAE组与高危非UAE组、低危UAE组与低危非USE组术中出血、住院时间、血β-HCG将至正常时间、月经复潮时间以及住院费用的差异。
术中出血指标,高危UAE组中,统计UAE操作中股动脉穿刺出血量与腹腔镜术中出血量之和;高危非UAE组中,统计腹腔镜术中出血量;低危UAE组中,统计UAE操作中股动脉穿刺出血量与清宫术中出血量之和;低危非UAE组中,统计清宫术中出血量。住院时间指标,从患者入院至出院的天数,出院标准为治疗后血β-HCG降至100 IU/L以下。β-HCG降至正常时间指标,本研究定义为治疗前最后一次测血β-HCG到出院后门诊随访至5 IU/L以下的天数,检测方法采用放射免疫法。月经复潮时间指标,治疗前末次月经时间至治疗后月经重新来潮的天数。住院费用指标,患者从入院至完成治疗出院所产生的总费用。
预测CSP再发风险,分析本研究入组患者中,有生育意愿,治疗后月经复潮满6个月,未采取避孕措施在随访期内证实再次妊娠,且排除输卵管妊娠者的数据。高危UAE组中,再次正常妊娠者12例、再次CSP者9例、输卵管妊娠1例;高危非UAE组中,再次正常妊娠者9例、再次CSP者8例、输卵管妊娠2例;低危UAE组中,再次正常妊娠者17例、再次CSP者2例、无输卵管妊娠;低危非UAE组中,再次正常妊娠者15例、再次CSP者5例、输卵管妊娠1例。再次妊娠为正常宫内妊娠者累计53例,纳入再次正常妊娠组,再次妊娠仍为CSP者累计21例,纳入再次CSP组,比较再次正常妊娠组与再次CSP组,在剖宫产次数、再次妊娠间隔时间、孕囊与膀胱间子宫肌层厚度、治疗方法(UAE治疗与非UAE治疗)的差异性。筛选出其中有统计学差异的指标,再进一步行多因素分析,从而预测CSP再发的危险因素。
1.4 统计学分析
2 结果
2.1 高危组及低危组相关临床指标、住院费用比较
高危UAE组与高危非UAE组、低危UAE组与低危非UAE组,在术中出血、住院时间、β-HCG降至正常时间以及月经复潮时间的指标比较中,差异均有统计学意义,且高危UAE组优于高危非UAE组,低危UAE组优于低危非UAE组(均P<0.05);在住院费用的比较中,高危UAE组高于高危非UAE组,低危UAE组高于低危非UAE组(均P<0.01),见表2。
表2 高危UAE组与高危非UAE组、低危UAE组与低危非UAE组术中出血、住院时间、人绒毛膜促性腺激素降至正常时间、月经复潮时间及住院费用的比较(±s)
table2 Comparison of intraoperative bleeding, length of stay, beta human chorionic gonadotropin dropped to normal time,menstruation recovery time and hospitalization expenses between high-risk UAE group and high-risk non UAE group and between low-risk UAE group and low-risk non UAE group (±s)

表2 高危UAE组与高危非UAE组、低危UAE组与低危非UAE组术中出血、住院时间、人绒毛膜促性腺激素降至正常时间、月经复潮时间及住院费用的比较(±s)
GroupnIntraoperativebleeding/mLLengthofstay/dBloodβ-HCGdroppedtonormaltime/dMenstruationrecoverytime/dHospitalizationexpenses/yuanHigh-riskgroup High-riskUAEgroup16736.5±14.85.9±0.917.9±8.718.1±1.620140±1520 High-risknonUAEgroup11676.5±39.79.6±1.328.7±10.124.3±1.813510±1013 P0.0260.0330.0310.0280.007Low-riskgroup Low-riskUAEgroup11393.2±43.310.2±1.450.1±17.656.3±6.710095±962 Low-risknonUAEgroup96284.8±110.530.7±9.667.5±22.965.9±9.33890±457 P0.0060.0290.0300.0340.004
UAE,uterine artery embolization;β-HCG,beta human chorionic gonadotropin.
2.2 CSP再发危险因素预测
单因素分析:再次正常妊娠组患者剖宫产次数、再次妊娠间隔时间、孕囊与膀胱间子宫肌层厚度、治疗方法(UAE治疗与非UAE治疗)与再次CSP组患者比较,差异有统计学意义(P<0.05),而两组间患者年龄、血β-HCG比较,差异无统计学意义(P>0.05),见表3。多因素分析:经单因素分析筛查出有预测意义的相关因素进行多因素分析,Logistic回归分析结果显示,剖宫产次数、治疗方法是CSP再发的独立预测因素(P<0.05),见表4,即减少剖宫产次数,并采用包含UAE在内的综合治疗方法可降低CSP再发风险。

表3 再次正常妊娠组与再次切口妊娠组患者临床指标的比较
UAE,uterine artery embolization;β-HCG,beta human chorionic gonadotropin;CSP,cesarean scar pregnancy.

表4 切口妊娠再发预测影响因素分析
3 讨论
3.1 CSP的病因
CSP的确切发病原因与机制目前仍不十分清晰,大多数研究认为与以下因素有关[11-12]: (1)孕卵运行过快、剖宫产引起子宫内膜间质蜕膜缺乏;(2)受精卵着床,发生底蜕膜缺损;(3)滋养细胞直接侵入子宫肌层,并不断生长,绒毛与子宫肌层粘连、植入甚至穿透子宫肌壁等。普遍认为本病病因是各种手术操作(如刮宫术、剖宫产术、子宫肌瘤剔除术、子宫成形术、宫腔镜甚至手取胎盘术等)所致的内膜损伤。Vial等[13]提出了CSP的2种生长方式, 一种是孕囊向宫腔方向生长, 个别可能活产,本研究中低危阻主要为此种生长方式;另一种是孕囊向膀胱、腹腔方向生长, 早期即可发生出血, 随孕周增大, 随时有发生子宫破裂大出血风险,本研究中高危组主要以此种方式生长。
3.2 CSP的治疗
由于对CSP的认识较晚,且缺乏多中心大样本的随机前瞻性研究, 目前仍无统一规范的治疗指南。大多数研究认为[14-15],在保障患者生命安全的情况下,控制出血、清除病灶,并尽量保留患者生育功能是主要的治疗原则。各医疗机构根据自身特点及优势,开展以UAE、腹腔镜下子宫下段病灶切除+修补术、全身及病灶局部化疗、B超监测下清宫术、阴式病灶清除术等手段为主的综合治疗,其中UAE正逐步成为CSP综合治疗方案中的一项重要技术,其优势主要有:(1)UAE治疗后,阻塞了子宫的主要血供,能达到有效止血的目的;(2)瘢痕病灶局部缺血缺氧促进了胚胎及滋养细胞坏死、萎缩及脱落,降低后期宫腔镜手术或清宫术中、术后发生大出血的概率;(3)栓塞术后血β-HCG下降快,月经复潮所需时间短;(4)栓塞时较大直径明胶海绵颗粒仅能栓塞末梢血管以上管腔,不破坏毛细血管网,可保证毛细血管平面侧支循环的通畅,使子宫可通过毛细血管网获得适量血供,不致发生栓塞后子宫壁缺血坏死。明胶海绵颗粒大约在2~3周后开始吸收,3个月后可完全吸收,使90%以上被栓塞血管再通,最大程度地保留了生育功能[16]。本研究UAE术中选用直径1 000~1 400 μm可吸收栓塞剂明胶海绵颗粒预处理后再行腹腔镜手术或清宫术,取得较满意效果。
3.3 CSP治疗经验
由于单一治疗手段的成功率难以令人满意,故目前CSP患者多采用综合治疗。入院后完善各项检查,依据停经周数、孕囊与膀胱间子宫肌层厚度、血β-HCG数值将患者分别纳入高危组及低危组。高危组停经时间长、孕囊与膀胱间子宫肌层厚度菲薄、血β-HCG数值高,以孕囊向膀胱、腹腔方向生长为主,清宫术中易发生子宫下段穿孔,导致难以控制的大出血,有时不得不切除子宫,故对于高危UAE组患者治疗一律行腹腔镜下子宫下段病灶切除+修补术,术前辅以UAE+动脉灌注化疗;高危非UAE组患者行腹腔镜手术并辅以MTX全身化疗;而低危组患者停经时间较短、孕囊与膀胱间子宫肌层厚度相对较厚、血β-HCG数值不太高,孕囊向宫腔方向生长,清宫术中严重并发症发生率相对较低,故对于低危UAE组患者采取B超监测下清宫,术前结合UAE+动脉灌注化疗;低危非UAE组患者清宫同时辅以MTX全身化疗以提高疗效。帅文等[17]对低危组的定义及治疗方式的选择与本研究相似。
本研究各项数据表明,无论是高危组还是低危组,采取UAE+动脉灌注化疗的患者在术中出血、住院天数、血β-HCG降至正常时间以及月经复潮时间的指标比较中均优于采取全身化疗患者,可见UAE对CSP治疗是有效的。同时,本研究多因素Logistic回归分析结果显示,治疗方法是CSP再发风险的独立预测因素,采用包含UAE在内的综合治疗方法可降低CSP再发风险。腹腔镜治疗虽能较为彻底地清除病灶,但由于其术后有新的手术瘢痕产生,而UAE则可闭塞原切口处新生血管,有效降低CSP再发率[18-19],故对有再次生育要求的患者有重要价值,但UAE治疗所需数字减影血管造影设备昂贵,且需要有熟练掌握子宫动脉插管技术的专业人员,手术费用较高,在基层医疗机构推广有一定难度。
综上所述,CSP病情凶险,且发病率呈上升趋势,已逐渐被人们所重视,应早期明确诊断并尽早终止妊娠。超声在其诊断、分型方面价值很高,对临床治疗能起到关键性指导作用。UAE因其疗效迅速可靠、并发症少、恢复快等优点,作为CSP综合治疗的重要手段被引入后,可明显降低术中出血、缩短住院天数及血β-HCG降至正常的时间、加速月经复潮,更重要的是可降低CSP再发风险,因此,在有条件的医院,特别是针对有再次生育要求的CSP患者,应将含UAE治疗手段的综合治疗方案列为首选。
[1]Pavlova E,Gunev D,Diavolov V,et al. Cesarean scar ectopic pregnancy:diagnosis with 2D,three-dimensional (3D) ultrasound and 3D power doppler of a case and review of the literature[J].Akush Ginekol(Sofiia), 2013, 52(6): 43-52.
[2]许燕军,张群锋.子宫动脉化疗栓塞术治疗子宫切口妊娠的临床效果分析[J].海南医学院学报, 2011, 17(5): 664-666.
[3]Sekiguchi A, Okuda N, Kawabata I, et al.Ultrasound detection of lacunae-like image of a cesareanscar pregnancy in the first trimester[J].J Nippon Med Sch, 2013, 80(1): 70-73.
[4]Seow KM, Wang PH, Huang LW, et al. Transvaginal sono-guided aspiration of gestational sac concurrent with a local methotrexate injection for the treatment of unruptured cesarean scar pregnancy[J].Arch Gynecol Obstet, 2013, 288(2): 361-366.
[5]An X, Ming X, Li K, et al. The analysis of efficacy and failure factors of uterine artery methotrexate infusion and embolization in treatment of cesarean scar pregnancy[J]. Sci World J, 2013, 2013 (9): 1351-1358.
[6]Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review[J]. Am J Obstet Gynecol, 2012, 207(1): 14-29.
[7]Shao MJ, Hu M, Hu MX. Conservative management of cesarean scar pregnancy by local injection of ethanol under hysteroscopic guidance[J].Int J Gynaecol Obstet, 2013, 121(3): 281-282.
[8]Yin X, Su S, Dong B, et al. Angiographic uterine artery chemoembolization followed by vacuum aspiration: an efficient and safe treatment for managing complicated cesarean scar pregnancy[J].Arch Gynecol Obstet, 2012, 285(5): 1313-1318.
[9]Yang XY,Yu H,Li KM, et al.Uterine artery embolisation combined with local methotrexate for treatment of caesarean scar pregnancy[J]. Br J Obstet Gynaecol, 2010, 117(8): 990-996.
[10]Godin PA,Bassil S,Donnez J.An ectopic pregnancy developing in a previous cesarean scar[J].Fertil Steril, 1997, 67(2): 398.
[11]Jain S,Simeja A,Malik R,et al. Cesarean scar pregnancy: a diagnostic dilemma and impending catastrophe [J].Arch Gynecol Obstet, 2014, 289(1): 221-222.
[12]Uysal F,Uysal A,Adam G. Cesarean scar pregnancy: diagnosis,management,and follow-up [J]. J Ultrasound Med, 2013, 32(7): 1295-1300.
[13]Vial Y, Petignat P, Hoblfeld P.Pregnancy in a cesarean scar[J].Ultrasound Obstet Gynecol, 2000, 16(6): 592-593.
[14]陈彦.子宫动脉灌注化疗栓塞联合宫腔镜电切术治疗子宫切口妊娠的临床价值[J].中国妇幼保健, 2012, 27(27): 4291-4293.
[15]Wang G,Liu X, Bi F,et al. Evaluation of the efficacy of laparoscopic resection for the management of exogenous cesarean scar pregnancy[J].Fertil Steril, 2014, 65(1): 68-72.
[16]Wozniak S, Pyra K, Kudka-Sternik M,et al.Uterine artery embolization using gelatin sponge particles performed due to massive vaginal bleeding caused by ectopic pregnancy within a cesarean scar: a case study[J].Ginekol Pol, 2013, 84(11): 966-969.
[17]帅文, 洪向丽, 鲍时华,等.剖宫产术后子宫切口瘢痕妊娠不同治疗方法的研究[J].生殖与避孕, 2010, 30(7): 463-467.
[18]Qian ZD,Huang LL,Zhu XM.Curettage or operative hysteroscopy in the treatment of cesarean scar pregnancy[J].Arch Gynecol Obstet, 2015, 292(5): 1055-1061.
[19]Gao LF,Huang Z,Gao J,et al.Uterine artery embolization followed by dilation and curettage within 24 hours compared with systemic methotrexate for cesarean scar pregna[J].Int J Gynaecol Obstet, 2014, 127(2): 147-151.
(2015-10-30收稿)
(本文编辑:刘淑萍)
Clinical application and prognostic analysis of interventional treatment for cesarean scar pregnancy
LU Jing-yuan1,2, GU Jian-ping1△, XU Wen-jian2, LOU Wen-sheng1, SHI Wan-yin1, WANG Tao1, SHAO Ze-feng1
(1. Department of Interventional Radiology,Affiliated Nanjing Hospital,Nanjing Medical University,Nanjing 210006,China;2. Department of Interventional Radiology, Nanjing Maternity and Child Health Hospital,Nanjing Medical University, Nanjing 210004,China)
Objective: To analyze the clinical value and prognosis of cesarean scar pregnancy (CSP) treated by uterine artery embolization (UAE). Methods: In the study, 492 cases of patients in Nanjing Maternal and Child Health Care Hospital Affiliated to Nanjing Medical University diagnosed as CSP between January 2011 and December 2014 were chosen, of which 283 were of high-risk group and 209 of low-risk group. According to whether to take UAE, the high-risk group was subdivided into high-risk UAE group(UAE+laparoscopic group), 167 cases, and high-risk non UAE group (chemotherapy+laparoscopic group), 116 cases, while the low-risk group was subdivided into low-risk UAE group (UAE+curettage group), 113 cases, and low-risk non UAE group(chemotherapy+curettage group), 96 cases. The differences of the intraoperative bleeding, length of stay, blood beta human chorionic go-nadotropin (β-HCG) dropped to normal time, menstruation recovery time and the hospitalization expenses were compared. And multivariate regression analysis was used to predict the recurrence risk of CSP. Results: The high-risk UAE group was better than the high-risk non UAE group in comparison of intraoperative bleeding [(36.5±14.8) mLvs.(76.5±39.7) mL], length of stay [(5.9±0.9) dvs.(9.6±1.3) d], blood β-HCG dropped to normal time [(17.9±8.7) dvs.(28.7±10.1) d] and menstruation recovery time [(18.1±1.6) dvs.(24.3±1.8) d],while the low-risk UAE group was better than the low-risk non UAE group in comparison of intraoperative bleeding [(93.2±43.3) mLvs.(284.8±110.5) mL], length of stay [(10.2±1.4) dvs. (30.7±9.6) d], blood β-HCG dropped to normal time [(50.1±17.6)dvs.(67.5±22.9)d] and menstruation recovery time[(56.3±6.7)dvs.(65.9±9.3) d], allP<0.05. The high-risk UAE group was higher than the high-risk non UAE group in comparison of hospitalization expenses [(20 140±1 520 )Yuanvs.(13 510±1 013) Yuan], and the low-risk group UAE was also higher than the low-risk non UAE group in comparison of hospitalization expenses [(10 095±962 )Yuanvs.(3 890±457) Yuan], allP<0.01. Multivariate Logistic regression analysis showed that the treatment method was independent predictor of CSP recurrence risk (OR2.407, 95%CI1.176-5.092,P<0.05), and using the comprehensive treatment including UAE could reduce the risk of recurrent CSP. Conclusion: As the efficacy of interventional therapy for CSP was rapid and reliable, fewer complications, faster recovery and lower recurrence, hospitalization with good conditions, and particularly for those patients with CSP who want to fertility again, the comprehensive treatment including UAE treatment should be the first choice.
Pregnancy, ectopic; Uterine artery embolization; Gelatin sponge, absorbable; Methotre-xate
国家自然科学基金(81541061)、江苏省科技发展基金临床医学专项(BL2014013)、南京市卫生科技发展基金重点项目(ZKX10004)、南京市科技发展项目(201402049)资助Supported by the National Natural Science Foundation of China (81541061), Jiangsu Province Science and Technology Development Fund Clinical Medicine Special(BL2014013), the Key Project of Nanjing Health Science and Technology Development Fund(ZKX10004), and Nanjing Science and Technology Development Project(201402049)
时间:2016-10-31 16:28:49
http://www.cnki.net/kcms/detail/11.4691.R.20161031.1628.024.html
R714.22
A
1671-167X(2016)06-1012-07
10.3969/j.issn.1671-167X.2016.06.016
△ Corresponding author’s e-mail, cjr.gujianping@vip.163.com