系统性红斑狼疮并发巩膜炎4例临床分析
王 乐,杨 月△,贾 园,苗 恒,周云杉,张晓盈
(北京大学人民医院 1.风湿免疫科, 2.眼科, 北京 100044)
·病例报告·
系统性红斑狼疮并发巩膜炎4例临床分析
王 乐1,杨 月1△,贾 园1,苗 恒2,周云杉1,张晓盈1
(北京大学人民医院 1.风湿免疫科, 2.眼科, 北京 100044)
红斑狼疮, 系统性;巩膜炎;自身免疫疾病
系统性红斑狼疮(systemic lupus erythematosus,SLE)是一种全身性自身免疫病,因多种自身抗体及血管炎的存在,患者可出现多器官、系统的受累。除脑、肺、心、肾等重要脏器外,还可出现眼部病变。眼部受累表现形式多样,从眼表到眼底疾病均可出现,其中以视网膜受累最为常见,也可出现巩膜受累。广义的巩膜炎包括表层巩膜炎及巩膜炎,其作为临床上一种相对少见的眼部疾病,发病率仅占眼部疾病总数的0.5%左右[1]。因SLE合并巩膜受累发病率低,多为个案报道,临床重视不足。但因巩膜受累可作为SLE的首发表现,且其常可引起多种急、慢性眼部并发症,如治疗不当可导致视力下降或眼球破坏,因此,识别表层巩膜炎及巩膜炎背后的SLE并尽早开始规范诊治尤其重要。本研究复习了4例于北京大学人民医院住院期间诊断为SLE继发表层巩膜炎或巩膜炎的病例,对其临床特点进行分析,并进行文献复习,为临床工作提供一定参考。
1 病例资料
2005年9月至2016年7月北京大学人民医院风湿免疫科收治的4例诊断SLE继发表层巩膜炎或巩膜炎的住院患者,其中女性3例、男性1例,年龄15~70岁,平均年龄(49.0±23.8)岁,初次发作表层巩膜炎或巩膜炎时SLE平均病程(2.1±1.4)年。4例病例均符合美国风湿病学会1997年推荐的SLE分类标准,其中1例(病例3)同时伴发干燥综合征。患者一般资料、临床表现及实验室检查如表1所示。
SLE的临床表现方面,表层巩膜炎或巩膜炎发作同时,3例患者均有关节肿痛症状,脱发1例,颊部红斑3例(其中2例伴光过敏),口腔溃疡1例,肌炎1例。器官系统受累方面,4例患者中1例患狼疮性肾炎;3例有呼吸系统受累,分别表现为肺间质病变(病例1、3)及胸腔积液(病例4),其中1例(病例4)患者同时存在心包积液及左侧睾丸鞘膜积液。患者既往病程中的其他表现见表1。4例中2例患者既往曾有血液系统受累,1例(病例2)为白细胞、血小板减少,另1例(病例3)为白细胞减少。辅助检查方面,全部4例患者均存在高滴度的抗核抗体(antinuclear antibody,ANA);2例发作表层巩膜炎或巩膜炎时抗双链DNA(double-stranded DNA,dsDNA)抗体升高;3例抗核小体抗体(anti-nucleosome antibody,ANuA)阳性,另1例未检测此指标;2例患者血清免疫球蛋白IgG升高,3例补体减低。
4例患者眼部受累情况、眼科并发症、治疗及预后如表2所示。患者均完成眼科专科查体(包括巩膜、结膜、角膜、虹膜睫状体及前房情况),测定视力及眼压,并进行常规裂隙灯和眼底镜检查。通过裂隙灯显微镜对巩膜病灶详细观察以确定诊断:10%(体积分数)新福林滴眼后进行观察,表层巩膜炎时巩膜表层血管充血可减轻、颜色变淡,巩膜组织并不受累;巩膜炎时巩膜水肿,且巩膜深部血管丛剧烈扩张并不消退。巩膜受累伴随“眼部并发症”的诊断:(1)视力下降:住院或随访期间复查视力下降≥2行或者视力≤0.25;(2)角膜炎:主要包括边缘硬化性及溃疡性角膜炎;(3)葡萄膜炎:前葡萄膜炎,眼前节出现1个以上浮游细胞;(4)眼压升高:眼压高于21 mmHg(1 mmHg=0.133 kPa);(5)视网膜和视神经炎:后极部视网膜水肿、渗出性脱离、视网膜絮状渗出、视乳头和/或黄斑部水肿及缺血性视神经病变。疑诊感染的患者完成眼部刮片细菌学及病毒免疫学检查。4例患者中,3例为表层巩膜炎,1例为巩膜炎;2例(病例2、4)为首次发作,另2例曾有反复发作。4例患者主要眼部表现包括眼痛、眼红、流泪,眼科查体主要发现包括球结膜充血水肿、表层巩膜或巩膜血管扩张,伴或不伴压痛。4例患者中,2例患者存在眼科并发症,包括1例葡萄膜炎(病例1)及1例视力下降(病例4)。眼科局部治疗方面,全部4例患者均接受糖皮质激素点眼治疗,其中1例患者接受非甾体抗炎药(nonsteroidalantiinflammatory drug,NSAID)点眼治疗,1例罹患巩膜炎的患者同时接受糖皮质激素球旁注射治疗;全身治疗方面,4例患者均接受糖皮质激素及免疫抑制治疗。表层巩膜炎及巩膜炎在治疗1周至2个月后消退。病例3患者治疗1周后眼部症状明显好转,治疗前后眼表情况对比见图1。以上患者长期在北京大学人民医院风湿免疫科门诊随诊,未再出现眼部不适主诉。
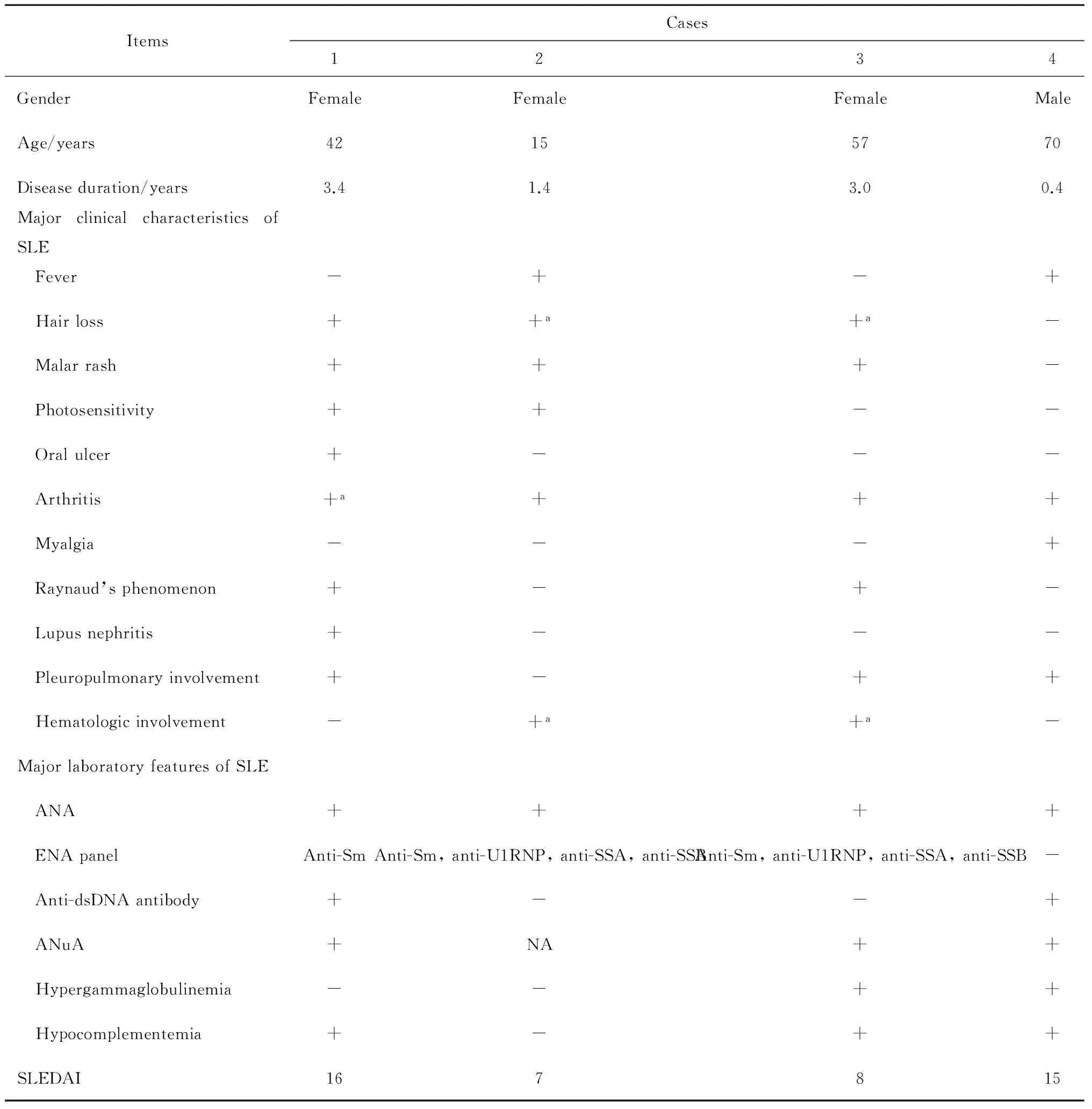
表1 4例患者的人口资料、临床表现及实验室检查
SLE, systemic lupus erythematosus; ANA, antinuclear antibody; ENA, extractable nuclear antigen; Sm, Smith; U1RNP, U1 ribonuclear protein; SSA, Sjögren’s syndrome A; SSB, Sjögren’s syndrome B; ANuA, anti-nucleosome antibody; SLEDAI, systemic lupus erythematosus disease activity index; NA, not applicable. a,past manifestations.
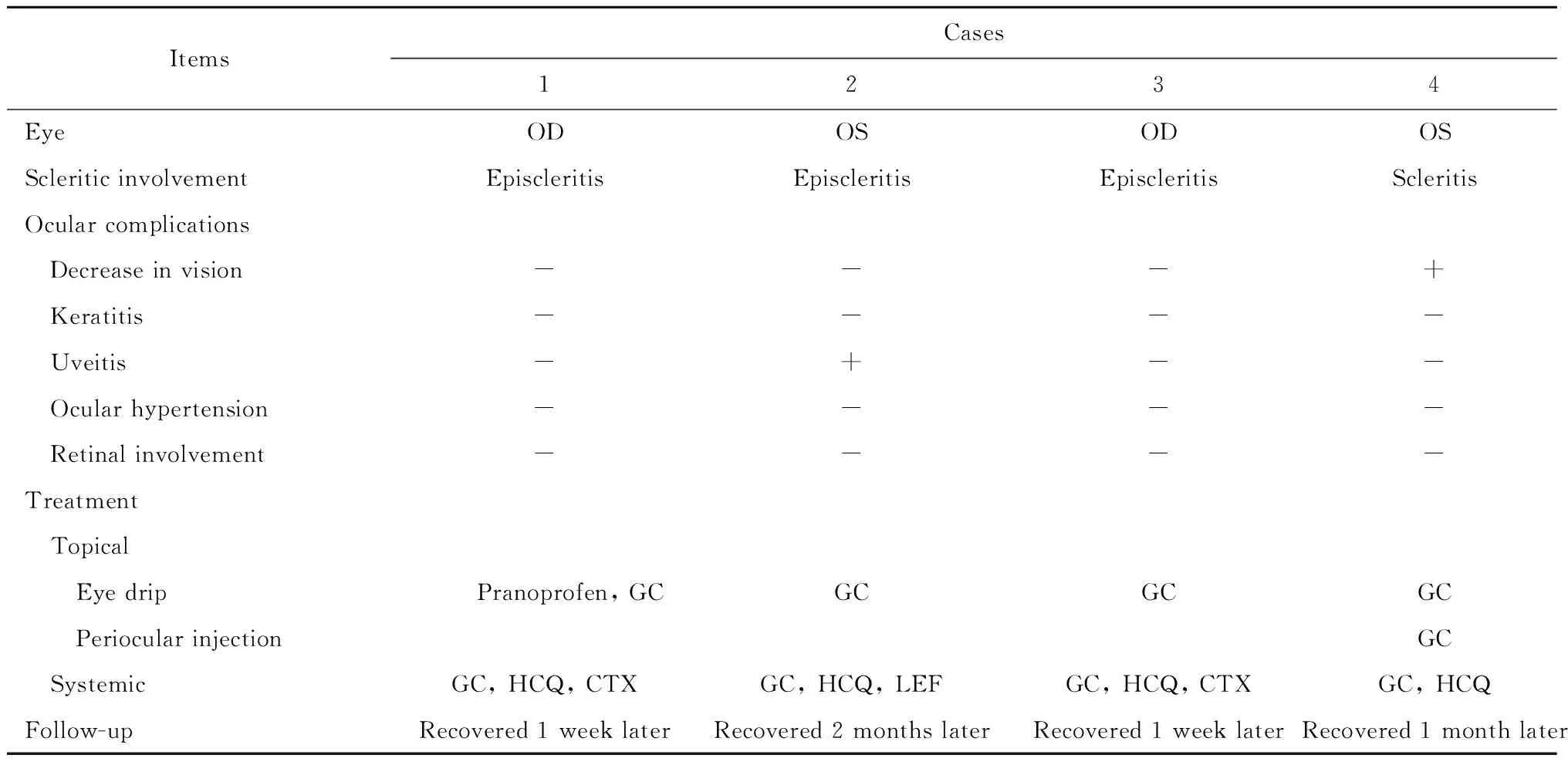
表2 4例患者的眼部受累情况及治疗随访情况
OD, right eye; OS, left eye; GC, glucocorticoid; HCQ, hydroxycloroquine; CTX,cyclophosphamide; LEF, leflunomide.
A,before the treatment, diffuse congestion of the superficial scleral and the conjunctiva was observed; B, after the treatment, the diffuse congestion lessened significantly.
图1 表层巩膜炎治疗前后眼表情况对比
Figure1 Comparison of ocular surface before and after the treatment of episcleritis
2 讨论
广义上的巩膜炎是一种相对少见的眼部疾病。Watson等[2]基于受累解剖部位的不同,又将广义巩膜炎分为表层巩膜炎和巩膜炎。两者均与自身免疫性疾病关系密切,有文献报道,30%~50%的病例可继发于自身免疫病,其中以类风湿关节炎最为常见,其次是肉芽肿性多血管炎,此外还可见于强直性脊柱炎、SLE、炎性肠病等[3-5]。我们回顾性分析2005年9月至2016年7月于北京大学人民医院风湿免疫科住院期间确诊表层巩膜炎或巩膜炎的患者共20例,其中除本文报道的SLE患者4例外,还有类风湿关节炎患者10例、系统性血管炎2例、复发性多软骨炎1例、类风湿关节炎合并复发性多血管炎1例、强直性脊柱炎1例及未分化结缔组织病1例。
尽管SLE合并表层巩膜炎及巩膜炎较为少见,且其危害多不及视网膜、葡萄膜或角膜病变,但从以下几个方面来看,对这一疾病的认知仍存在重要意义。首先,表层巩膜炎及巩膜炎可以作为SLE的首发表现存在,因此,眼科医师在接诊此类患者时,需注意询问SLE的相关表现,并完善血清学检查,以早期发现巩膜受累背后潜在的全身系统性疾病。其次,表层巩膜炎及巩膜炎易反复出现,且可作为SLE全身病情活动的一部分,因此,在巩膜病变再次出现时,需注意警惕SLE的复发及病情活动。此外,巩膜病变虽较视网膜、葡萄膜或角膜病变危害小,但其容易并发以上部位受累,出现眼部并发症,进而导致视力下降及眼球破坏。周玉梅等[6]对90例眼科门诊就诊的表层巩膜炎及巩膜炎患者进行分析,发现64.4%的患者出现视力下降、葡萄膜炎、角膜炎、眼压升高、白内障等多种眼部并发症,因此,早期诊治表层巩膜炎及巩膜炎对预防这些眼部并发症的发生亦存在重要意义。北京大学人民医院收治的4例患者中,2例患者伴发眼部并发症、4例患者均伴随SLE的其他器官系统受累表现,系统性红斑狼疮病变活动指数(systemic lupus erythematosus disease activity index,SLEDAI)评分7~16分,提示病情活动。
表层巩膜炎及巩膜炎的病理生理机制较复杂,SLE患者出现巩膜受累的发病机制尚不明确。目前认为,血管炎在发病中发挥主要作用。在SLE继发坏死性巩膜炎的活检标本中,可观察到血管炎及肉芽肿性炎症,提示在疾病早期及后期的迟发型高敏反应中,存在免疫复合物的参与。此外,多种细胞包括Th17细胞、NK细胞等[7]亦被认为参与炎症的启动及维持。临床表现方面,表层巩膜炎及巩膜炎两者均以眼痛、眼红、流泪等非特异表现为主,可单眼发病或双眼同时发病,双眼发病率约为40%。表层巩膜炎多呈现自限性、易复发、良性病程的特点。相比之下,前巩膜炎症状多更为剧烈,而后巩膜炎在临床上则多缺乏明显的症状特征,但因其炎症区接近黄斑、视网膜和视神经,所以潜在危害性更大,如未规范诊治可迅速导致失明。本文中观察到的4例患者中3例为表层巩膜炎(其中1例并发葡萄膜炎),1例为巩膜炎,并发视力下降。
在SLE相关表层巩膜炎及巩膜炎的治疗方面,需同时兼顾眼部病变及SLE全身病情,并借鉴眼科非感染性巩膜炎的相关经验。表层巩膜炎及巩膜炎的治疗可分为局部及全身治疗。局部治疗包括外用糖皮质激素及NSAID类药物点眼,以及眶周或球后注射糖皮质激素。外用药物点眼常用于病情较轻的表层巩膜炎及前巩膜炎,优点是使用方便及副作用较小。局部注射曲安奈德适用于巩膜炎,尤其是坏死性巩膜炎的患者。不良反应是可导致结膜出血及眼压升高,并增加巩膜坏死和穿孔的风险,因此其应用需谨慎。继发于风湿免疫病(包括SLE)的巩膜受累患者较少单独使用局部治疗,因为虽有文献报道单独外用糖皮质激素治疗的成功率可达47%,但其定义的时间范围为2个月内[8]。继发于SLE的巩膜受累易反复发作,局部治疗失败率较高,绝大多数患者需要同时进行全身治疗。全身治疗包括口服非甾体抗炎药、激素及免疫抑制剂或生物制剂。口服NSAID是治疗表层巩膜炎及巩膜炎的一线用药,但SLE患者多同时口服糖皮质激素,故继发消化道溃疡的风险较大,需慎用此类药物,必要时可选择环氧化酶-2(cyclooxygenase,COX-2)抑制剂。口服糖皮质激素治疗是公认的NSAID治疗无效的非坏死性巩膜炎患者的一线治疗方案,起始剂量以1 mg/(kg·d)为宜。合并表层巩膜炎的SLE患者多同时伴有全身其他器官、系统受累,因此糖皮质激素亦为首选药物,其剂量根据眼部病变性质及全身病情个体化决定。如经口服糖皮质激素治疗1个月仍无反应,则可加用免疫抑制剂。目前广泛应用的免疫抑制剂包括抗代谢药如甲氨蝶呤、硫唑嘌呤及霉酚酸酯,烷化剂如环磷酰胺(cyclophosphamide,CTX)、苯丁酸氮芥,T细胞抑制剂如CsA及他克莫司[9-10],而对以上治疗仍效果不佳的患者,则可考虑选择生物制剂[包括肿瘤坏死因子(tumor necrosis factor,TNF)抑制剂[11-12]及CD20单抗[13]治疗]。有文献报道,在1例ANA阳性的非坏死性前巩膜炎患者中,使用英夫利昔单抗治疗后,巩膜炎病情一度好转,但随即出现复发,伴发热、血细胞减少、心包炎、抗dsDNA抗体阳性,确诊SLE,最终在更换为激素联合利妥昔单抗治疗后病情好转[14]。本文报道的4例患者均接受局部糖皮质激素点眼及全身糖皮质激素口服治疗;免疫抑制剂方面,其中2例接受CTX静脉注射,1例接受口服来氟米特,另1例没有加免疫抑制剂,只用了抗疟药羟氯喹。经以上治疗后患者眼科症状很快好转。
综上所述,SLE继发表层巩膜炎或巩膜炎报道的较少,继发于SLE的表层巩膜炎及巩膜炎可与SLE病情活动相关,甚至可能早于其他的系统性损害之前作为首发表现出现,因此早期诊断、积极治疗无论对于视力的保护或是SLE的全身治疗均意义重大。在本文报道的4例SLE继发表层巩膜炎的病例中,患者均在病程初期或激素、免疫抑制剂减量后病情复发时出现眼部疼痛、发红表现,同时伴有其他器官、系统的SLE活动表现,经全身激素及免疫抑制剂联合局部眼部激素及非甾体抗炎药治疗效果良好,因此,对于继发表层巩膜炎或巩膜炎的SLE患者,建议积极评估全身受累情况,尽早开始积极的干预(包括糖皮质激素以及免疫抑制剂的使用)。通过积极治疗,系统性红斑狼疮继发表层巩膜炎或巩膜炎的患者一般预后良好,随着SLE全身疾病的控制,巩膜炎也多随之缓解。
[1]李凤鸣.中华眼科学[M]. 北京:人民卫生出版社, 2006: 1394-1402.
[2]Watson PG,Hayreh SS. Scleritis and episcleritis[J].Br J Ophthalmol, 1976, 60(3): 163-191.
[3]Watson PG, Young RD. Scleral structure,organisation and disease. A review[J]. Exp Eye Res, 2004, 78(3): 609-623.
[4]Sainz de la Maza M,Foster CS,Jabbur NS,et al. Scleritis associa-ted with systemic vasculitic diseases[J]. Ophthalmology, 1995, 102(4): 687-692.
[5]Hamideh F,Prete PE. Ophthalmologic manifestations of rheumatic diseases[J]. Semin Arthritis Rheum, 2001, 30(4): 217-241.
[6]周玉梅,王智群,张阳,等. 表层巩膜炎及巩膜炎90例临床分析[J]. 中华眼科杂志, 2014, 50(4): 261-266.
[7]Yeh S,Li Z,Sen HN,et al.Scleritis and multiple systemic auto-immune manifestations inchronic natural killer cell lymphocytosis associated with elevated TCR alpha/beta+CD3+CD4-CD8-double-negative T cells[J].Br J Ophthalmol, 2010, 94(6): 748-752.
[8]McMullen M, Kovarik G, Hodge WG. Use of topical steroid therapy in the management of nonnecrotizing anterior scleritis[J]. Can J Ophthalmol, 1999, 34(4): 217-221.
[9]Rachitskaya A,Mandelcorn ED,Albini TA. An update on the cause and treatment of scleritis[J].Curr Opin Ophthalmol, 2010, 21(6): 463-467.
[10]Kempen JH,Daniel E,Gangaputra S,et al. Methods for identifying long-term adverse effects of treatment in patients with eye diseases: the Systemic Immunosuppressive Therapy for Eye Diseases (SITE) Cohort Study[J].Ophthalmic Epidemiol, 2008, 15(1): 47-55.
[11]Doctor P,Sultan A,Syed S,et al. Infliximab for the treatment of refractory scleritis[J]. Br J Ophthalmol, 2010, 94(5): 579-583.
[12]Restrepo JP,Molina MP. Successful treatment of severe nodular scleritis with adalimumab[J]. Clin Rheumatol, 2010, 29(5): 559-561.
[13]Chauhan S,Kamal A,Thompson RN,et al. Rituximab for trea-tment of scleritis associated with rheumatoid arthritis[J]. Br J Ophthalmol, 2009, 93(7): 984-985.
[14]Adler S,Kolev M,Varisco PA,et al. Induction of severe systemic lupus erythematosus by TNF blockade and response toanti-IL-6 strategy[J].Allergy clinimmunol, 2013, 131(4): 1235-1236.
(2016-08-15收稿)
(本文编辑:刘淑萍)
SUMMARY Episcleritis and scleritis are relatively rare ocular diseases, which are commonly associated with rheumatic diseases including systemic lupus erythematosus (SLE). To investigate clinical and laboratory features of SLE-associated episcleritis and scleritis, we now report 4 cases of inpatients who were diagnosed with episcleritis or scleritis secondary to SLE from September 2005 to July 2016 in the Department of Rheumatology and Immunology in Peking University People’s Hospital. Demographic, clinical and laboratory characteristics were summarized together with the treatment regimen and the prognosis; the literature was reviewed. There were 3 female and 1 male patients. The average age was (49.0±23.8) years and the mean duration of SLE at the onset of episcleritis or scleritis was (2.1±1.4) years. In addition to the eye involvement, the patients had mucocutaneous manifestations, serositis, lupus nephritis and interstitial pneumonia simultaneously; in the past, 1 patient experienced arthritis, 2 presented Raynaud’s phenomenon, and 2 had hematologic involvement. All the patients had antinuclear antibody (ANA) of high titer. The anti double-stranded DNA (ds-DNA) antibody titers were increased in 2 patients. Three patients had positive anti-nucleosome antibody (ANuA) while the other 1 patient did not test it. The complement levels were decreased in 3 patients. The systemic lupus erythematosus disease activity index (SLEDAI) scores were more than 4 points in all the patients (ranging from 7-16), suggesting active disease. Ocular symptoms included pain, redness of the eye and tears. Ophthalmic examinations revealed 3 cases of episcleritis and 1 case of scleritis. Among the 4 patients, 2 patients expe-rienced ocular complications including decrease in vision and uveitis. All the patients were treated with systemic corticosteroids combined with hydroxycloroquine; 3 patients were treated with immunosuppres-sants (cyclophosphamide in 2 patients and leflunomide in 1 patient). All of the 4 patients received topical steroid and 1 patient received periocular injection of triamcinolone acetonide; 1 patient received topical nonsteroidal anti-inflammatory drug (NSAID).No recurrence of episcleritis or scleritis was observed during the follow-ups. As a conclusion, scleritis and episcleritis, although uncommon, may occur in patients with autoimmune rheumatic diseases including SLE. The occurrence of episcleritis and scleritis may suggest active disease of SLE. Ocular complications need to be aware of in the patients. Prompt diagnosis and treatment was associated with good visual outcomes in the follow-ups.
Clinical characteristics of 4 cases of scleritis associated with systemic lupus erythematosus
WANG Le1, YANG Yue1△, JIA Yuan1, MIAO Heng2, ZHOU Yun-shan1, ZHANG Xiao-ying1
(1. Department of Rheumatology and Immunology, 2. Department of Ophtalmology,Peking University People’s Hospital, Beijing 100044, China)
Lupus erythematosus, systemic; Scleritis; Autoimmune diseases
国家自然科学基金(31300721)、高等学校博士学科点专项科研基金新教师类(20130001120066)资助Supported by the National Natural Science Foundation of China (31300721) and the Research Fund for the Doctoral Program of Higher Education of China (20130001120066)
R593.24
A
1671-167X(2016)06-1081-05
10.3969/j.issn.1671-167X.2016.06.028
时间:2016-10-31 16:04:18
http://www.cnki.net/kcms/detail/11.4691.R.20161031.1604.010.html
△ Corresponding author’s e-mail, yyang216@icloud.com