沉默糖原合成激酶3β表达对胰腺癌PANC1细胞生长及上皮间质转化的影响
宋博 马洪运 李森 邵卓 宋彬 郝俊 程鹏 金钢
200433 上海,第二军医大学附属长海医院胰腺肝胆外科(宋博、马洪运、李森、邵卓、宋彬、郝俊、程鹏、金钢);解放军第454医院普外科(宋博)
·论著·
沉默糖原合成激酶3β表达对胰腺癌PANC1细胞生长及上皮间质转化的影响
宋博马洪运李森邵卓宋彬郝俊程鹏金钢
200433上海,第二军医大学附属长海医院胰腺肝胆外科(宋博、马洪运、李森、邵卓、宋彬、郝俊、程鹏、金钢);解放军第454医院普外科(宋博)
【摘要】目的观察沉默糖原合成激酶3β(GSK3β)的表达对胰腺癌PANC1细胞增殖及上皮间质转化(EMT)的影响,探讨其作用机制。方法设计并合成靶向GSK3β的3个siRNA(siRNA-GSK3β)及阴性对照siRNA(siRNA-NC),分别转染PANC1细胞。通过RT-PCR法检测各组细胞GSK3β mRNA表达量,筛选基因沉默效果最佳的siRNA进行后续实验。采用MTT法检测转染细胞的增殖。采用RT-PCR法检测转染细胞Wnt/β-catenin通路成员Wnt、β-catenin、C-myc、CyclinD1mRNA;Hedgehog通路成员Shh、Smo mRNA;PI3K/Akt/mTOR通路成员PI3K、Akt、mTOR、4E-BP1、p70S6K mRNA以及EMT相关分子Slug、Snail、Twist、E-cadherin、N-cadherin、Vimentin mRNA的表达。结果转染siRNA-NC的PANC1细胞GSK3β mRNA表达量为1.00±0.15,3个转染siRNA-GSK3β的GSK3β mRNA表达量分别为0.25±0.08、0.62±0.09、0.70±0.11,转染siRNA-GSK3β细胞均显著低于转染siRNA-NC细胞,差异有统计学意义(P值均<0.0001 )。转染后siRNA-GSK3β组细胞的增殖显著低于转染siRNA-NC组细胞,差异有统计学意义(P<0.05)。转染后siRNA-GSK3β组细胞的Wnt、β-catenin、C-myc、CyclinD1、PI3K、Akt、mTOR、4E-BP1、p70S6K、Slug、Snail、N-cadherin、Vimentin mRNA表达量分别为0.28±0.04、0.47±0.05、0.37±0.05、0.62±0.08、0.22±0.03、0.47±0.06、0.65±0.08、0.39±0.04、0.56±0.07、0.33±0.05、0.46±0.07、0.55±0.06、0.38±0.04,均显著低于转染siRNA-NC组细胞,差异有统计学意义(P值均<0.05);Shh、Smo mRNA表达量分别为1.10±0.13、1.05±0.11,与转染siRNA-NC组细胞的差异无统计学意义;Twist mRNA表达量为0.62±0.08,低于转染siRNA-NC组细胞,E-cadherin mRNA表达量为2.12±0.25,高于转染siRNA-NC组细胞,但差异均无统计学意义。结论沉默PANC1细胞GSK3β基因表达后能够通过Wnt/β-catenin、PI3K/Akt通路抑制胰腺癌细胞的增殖,并抑制其上皮间质转化过程。
【关键词】胰腺肿瘤;糖原合成酶激酶3β;细胞增殖;上皮间质转化
胰腺癌是消化系统恶性程度极高、预后极差的恶性肿瘤,流行病学资料显示,胰腺癌患者的中位生存时间不足6个月、5年生存率更低于5%[1-2]。胰腺癌的早期诊断较为困难,确诊后又缺乏有效的靶向治疗手段,因此患者预后不佳[3]。近年来,糖原合成激酶3β(glycogen synthase kinase 3β, GSK3β)的生物学功能受到了越来越多的重视。GSK3β定位于胞质,属于丝氨酸/苏氨酸蛋白激酶,对细胞增殖、分化、侵袭等均具有调控作用[4-5]。本研究应用RNA干扰技术沉默胰腺癌细胞株PANC1的GSK3β表达,观察其对胰腺癌细胞增殖及上皮间质转化(epithelial-mesenchymal transition,EMT)的影响,探讨其作用机制。
材料与方法
一、材料
胰腺癌细胞株PANC1购自中科院细胞库,DMEM培养基、胎牛血清、胰蛋白酶均购自Gibco公司,转染试剂盒购自Invitrogen公司,MTT细胞活力试剂盒购自Promega公司,RNAiso提取液、反转录试剂盒以及PCR扩增试剂盒均购自Takara公司。
二、方法
1.细胞培养及siRNA转染:PANC1细胞复苏后用含有10%胎牛血清的DMEM在培养瓶中培养,待细胞生长至70%~80%融合后用0.125%的胰蛋白酶消化并传代。传代细胞接种于96孔培养板,每孔1×103个细胞。培养过夜后弃含血清的DMEM更换为无血清的DMEM继续培养24 h。委托吉玛公司设计及合成3个靶向GSK3β的siRNA,分别命名为siRNA-GSK3β-1、siRNA-GSK3β-2、siRNA-GSK3β-3。siRNA-GSK3β-1正义序列为5′-CAAGUC-GAUUUAGCUAGUC-3′,反义序列5′-UACCAAGUGUCCGUAGCGU-3′;siRNA-GSK3β-2正义序列5′-AUUUACACUUAAUCAUUC-3′,反义序列5′-UUAUUGCCGCUUAAGCUAGC-3′;siRNA-GSK3β-3正义序列5′-CGUAAAGCUAGCUAGCUG-3′,反义序列5′-AAUGGCAGCAAGUGCAU-3′。同时设计及合成阴性对照siRNA(siRNA-NC)。将转染试剂分别与3个siRNA-GSK3β及siRNA-NC按1∶2的比例混合,采用脂质体法将它们分别转染PANC1细胞,以不加siRNA的细胞作为阴性对照,每组设3个复孔,按试剂盒说明书操作。
2.细胞增殖检测:PANC1细胞转染siRNA-GSK3β或siRNA-NC前及转染后6、12、18、24 h分别在细胞培养孔内加入MTT 20 μl,孵育4 h,上酶标仪上读取各孔波长560 nm处的吸光值(A560值)。
3.转染细胞相关基因的mRNA表达检测:取PANC1细胞接种于12孔细胞板,每孔5×104个细胞,转染siRNA-GSK3β或siRNA-NC后24 h弃培养液,加入RNAiso提取液0.5 ml,用细胞刮刀充分裂解细胞,并依次加入三氯甲烷、异丙醇、95%乙醇抽提总RNA,加入DEPC水溶解。采用逆转录试剂盒及PCR试剂盒进行RT-PCR扩增。各基因的引物序列及退火温度见表1。引物由上海吉玛公司合成。逆转录反应条件:25℃ 10 min,42℃ 30 min,85℃ 5 min;PCR扩增条件:95℃ 10 s、退火温度15 s、72℃ 20 s,40个循环。由仪器自带软件获得Ct值,以siRNA-NC组细胞GSK3β mRNA表达量为1,计算siRNA-GSK3β组细胞GSK3β mRNA的相对表达量。
三、统计学处理
结果
一、转染细胞的沉默效果
转染siRNA-GSK3β-1、siRNA-GSK3β-2、siRNA-GSK3β-3、siRNA-NC的PANC1细胞GSK3β mRNA相对表达量分别为0.62±0.09、0.25±0.08、0.70±0.11、1.00±0.15。转染siRNA-GSK3β的3组细胞表达量均显著低于转染siRNA-NC细胞,差异有统计学意义(P值均<0.0001 ),其中以转染siRNA-GSK3β-2细胞的GSK3β沉默效率最高,以此转染细胞用于后续实验。
二、细胞增殖变化
转染前两组细胞的增殖差异无统计学意义。转染后siRNA-GSK3β组PANC1细胞的增殖显著低于siRNA-NC组,差异均有统计学意义(表2)。
三、转染细胞Wnt/β-catenin、Hedgehog通路成员mRNA表达的变化
转染24 h后siRNA-GSK3β组细胞Wnt/β-catenin通路成员Wnt、β-catenin、C-myc、CyclinD1 mRNA表达量均显著低于siRNA-NC组,差异有统计学意义;Hedgehog通路成员Shh、Smo mRNA表达量与siRNA-NC组的差异无统计学意义(表3)。
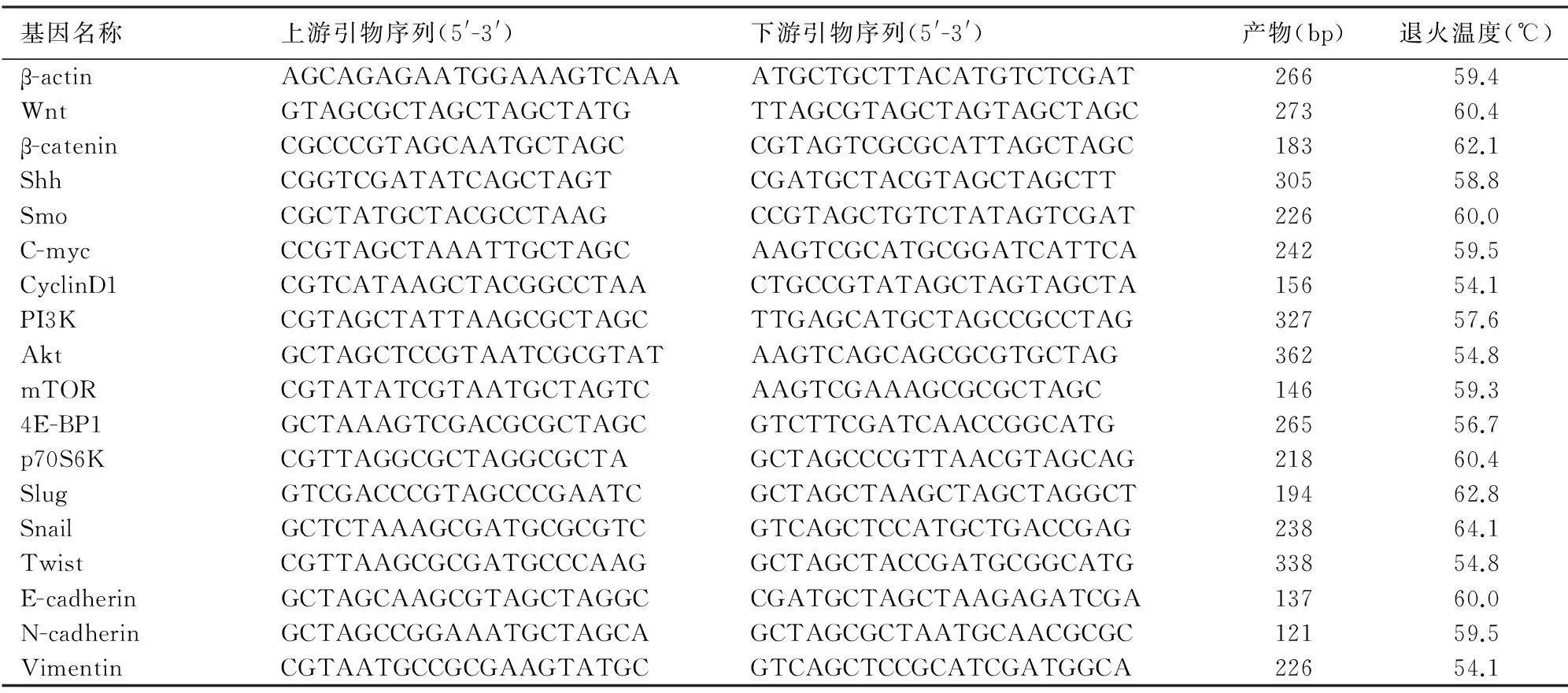
表1 转染细胞相关基因mRNA的引物序列

表2 siRNA-GSK3β组和siRNA-NC组细胞的增殖变化(A560值,

表3 转染细胞Wnt/β-catenin、Hedgehog通路成员mRNA表达量
四、转染细胞PI3K/Akt/mTOR通路成员 mRNA表达的变化
转染24 h后siRNA-GSK3β组细胞PI3K/Akt/mTOR通路成员PI3K、Akt、mTOR、4E-BP1、p70S6K mRNA表达量均显著低于siRNA-NC组,差异有统计学意义(表4)。
五、转染细胞EMT相关分子mRNA表达的变化
转染24 h后siRNA-GSK3β组细胞EMT相关分子Slug、Snail、N-cadherin、Vimentin mRNA表达量均显著低于siRNA-NC组,差异均有统计学意义。而Twist mRNA表达量低于siRNA-NC组,E-cadherin mRNA表达量高于siRNA-NC组,但差异均无统计学意义(表4)。
讨论
GSK3β是近年来倍受重视的一类蛋白激酶,它不但能使多种底物磷酸化,而且参与Wnt/β-catenin、PI3K/Akt及Hedgehog等信号通路的调控,对细胞的增殖、分化、侵袭等生物学行为均具有调控作用[6]。Shakoori等[7]报道,结肠癌组织GSK3β及其活性形式的表达水平显著高于其配对的周围正常组织,并且多种结肠癌细胞系GSK3β基因均高表达;应用GSK3β特异性抑制剂或RNA干扰技术抑制GSK3β的表达均能显著抑制多种结肠癌细胞的增殖,促进细胞凋亡,提示GSK3β表达异常与肿瘤的发生、发展有关。但GSK3β究竟发挥促肿瘤生长的作用还是抑肿瘤生长的作用尚无统一认识。Shao等[8]报道,GSK3β通过降解c-Jun以抑制乳腺癌细胞的生长和成瘤过程,但Grassilli等[9]和Liu等[10]的研究则认为GSK3β对结肠癌、肺癌细胞的生长、上皮充质转化具有促进作用。目前关于GSK3β是否参与胰腺癌的发生和发展以及如何调控胰腺癌细胞的生物学行为的研究较少。
本研究将siRNA-GSK3β转染胰腺癌细胞PANC1,结果显示转染细胞的GSK3β mRNA表达量显著下调,细胞的增殖明显被抑制。
GSK3β的下游信号通路涉及Wnt/β-catenin、PI3K/Akt、Hedgehog等[4, 11-12]。 Wnt/β-catenin和Hedgehog信号通路调节的下游靶基因均为C-myc、CyclinD1等促增殖基因。Wnt分子被活化后,β-catenin的降解过程受阻并在胞质中大量蓄积,转位进入细胞核后能启动C-myc、CyclinD1的转录过程[13-14]。Hedgehog通路中Shh被活化后Ptch对Smo的结合和抑制作用丧失,Smo释放并通过多种转录因子促进C-myc、CyclinD1的表达[15]。PI3K/Akt通路的上游激活信号由EGFR介导,而下游的效应分子为mTOR。mTOR能够通过4E-BP1和p70S6K抑制细胞凋亡、促进细胞增殖[16]。本研究结果显示,PANC1细胞转染siRNA-GSK3β后,细胞Wnt、β-catenin、C-myc、CyclinD1、PI3K、Akt、mTOR、4E-BP1、p70S6K mRNA表达量均显著低于转染siRNA-NC的PANC1细胞,差异均有统计学意义,而两组细胞Shh、Smo mRNA表达量的差异无统计学意义,提示PANC1细胞的Wnt/β-catenin、PI3K/Akt信号通路调控GSK3β基因的表达,而Hedgehog通路不参与GSK3β基因的调控。
EMT是指上皮细胞失去细胞极性并向具有较高侵袭、迁移能力的间质细胞转化。上皮细胞是人类进化过程中的终端细胞,通过细胞两面的极性形成紧密黏附,进而阻滞细胞的迁移过程;间质细胞具有较强的迁移和侵袭能力,细胞间结构松散且连接较少,能够促进细胞发生原位浸润以及远处转移[17-18]。Slug、Snail、Twist是调节EMT过程重要的转录因子,能够抑制上皮细胞标志分子E-cadherin的表达、增加间质细胞标志分子N-cadherin、Vimentin的表达[19]。近年来关于胰腺癌生物学特征的研究证实,EMT是造成胰腺癌病情进展的重要环节。本研究结果显示,PANC1细胞转染siRNA-GSK3β后,细胞Slug、Snail、Twist、N-cadherin、Vimentin mRNA表达量低于转染siRNA-NC的细胞,E-cadherin mRNA表达量高于转染siRNA-NC的细胞,提示抑制GSK3β基因表达能够阻碍胰腺癌细胞的EMT过程,为胰腺癌靶向GSK3β的基因治疗提供实验依据。

表4 转染细胞PI3K/Akt/mTOR通路成员及EMT相关分子mRNA表达量
参考文献
[1]Mettu NB, Abbruzzese JL. Clinical insights into the biology and treatment of pancreatic cancer[J]. J Oncol Pract, 2016, 12(1): 17-23.DOI:10.1200/JOP.2015.009092.
[2]Verma A, Shukla S, Verma N. Diagnosis, preoperative evaluation, and assessment of resectability of pancreatic and periampullary cancer[J]. Indian J Surg, 2015, 77(5): 362-370.DOI:10.1007/S12262-015-1370-0.
[3]Takakura K, Koido S. Direct therapeutic intervention for advanced pancreatic cancer[J]. World J Clin Oncol, 2015, 6(6): 216-219.DOI:10.5306/wjco.v6.ib.216.
[4]Trnski D, Sabol M, Gojevic A, et al. GSK3beta and Gli3 play a role in activation of Hedgehog-Gli pathway in human colon cancer-Targeting GSK3beta downregulates the signaling pathway and reduces cell proliferation[J]. Biochim Biophys Acta, 2015, 1852(12): 2574-2584.DOI:10.1016/j.bbadis.2015.09.005.
[5]Zhang L, Tu Y, He W, et al. A novel mechanism of hepatocellular carcinoma cell apoptosis induced by lupeol via Brain-Derived Neurotrophic Factor Inhibition and Glycogen Synthase Kinase 3 beta reactivation[J]. Eur J Pharmacol, 2015, 762:55-62.DOI:10.1016/j.ejphar.2015.05.030.
[6]Morfini G, Szebenyi G, Brown H, et al. A novel CDK5-dependent pathway for regulating GSK3 activity and kinesin-driven motility in neurons[J]. EMBO J, 2004, 23(11): 2235-2245.DOI:10.1038/sj.emboj.7600237.
[7]Shakoori A, Ougolkov A, Yu ZW, et al. Deregulated GSK3beta activity in colorectal cancer: its association with tumor cell survival and proliferation[J]. Biochem Biophys Res Commun, 2005, 334(4): 1365-1373.DOI:10.1016/j.bbrc.2005.07.041.
[8]Shao J, Teng Y, Padia R, et al. COP1 and GSK3beta cooperate to promote c-Jun degradation and inhibit breast cancer cell tumorigenesis[J]. Neoplasia, 2013, 15(9): 1075-1085.
[9]Grassilli E, Narloch R, Federzoni E, et al. Inhibition of GSK3B bypass drug resistance of p53-null colon carcinomas by enabling necroptosis in response to chemotherapy[J]. Clin Cancer Res, 2013, 19(14): 3820-3831.DOI:10.1158/1078-0432.CCR-12-3289.
[10]Liu ZC, Chen XH, Song HX, et al. Snail regulated by PKC/GSK-3beta pathway is crucial for EGF-induced epithelial-mesenchymal transition (EMT) of cancer cells[J]. Cell Tissue Res, 2014, 358(2): 491-502.DOI:10.1007/S00441-014-1953-2.
[11]Hsieh HY, Shen CH, Lin RI, et al. Cyproheptadine exhibits antitumor activity in urothelial carcinoma cells by targeting GSK3beta to suppress mTOR and beta-catenin signaling pathways[J]. Cancer Lett, 2016, 370(1): 56-65.DOI:10.1016/j.canlet.2015.09.018.
[12]Koga T, Suico MA, Shimasaki S, et al. Endoplasmic reticulum (ER) stress induces sirtuin 1 (SIRT1) expression via the PI3K-Akt-GSK3beta signaling pathway and promotes hepatocellular injury[J]. J Biol Chem, 2015, 290(51): 30366-30374.DOI:10.1074/jbc.M115.664169.
[13]Rennoll S, Yochum G. Regulation of MYC gene expression by aberrant Wnt/beta-catenin signaling in colorectal cancer[J]. World J Biol Chem, 2015, 6(4): 290-300.DOI:10.4331/wjbc.vb.i4.290.
[14]Gopalakrishnan N, Saravanakumar M, Madankumar P, et al. Colocalization of beta-catenin with Notch intracellular domain in colon cancer: a possible role of Notch1 signaling in activation of CyclinD1-mediated cell proliferation[J]. Mol Cell Biochem, 2014, 396(1-2): 281-293.DOI:10.1007/S11010-014-21163-7.
[15]Mille F, Tamayo-Orrego L, Levesque M, et al. The Shh receptor Boc promotes progression of early medulloblastoma to advanced tumors[J]. Dev Cell, 2014, 31(1): 34-47.DOI:10.1016/j.devcel.2014.08.010.
[16]Soares HP, Ming M, Mellon M, et al. Dual PI3K/mTOR inhibitors induce rapid overactivation of the MEK/ERK pathway in human pancreatic cancer cells through suppression of mTORC2[J]. Mol Cancer Ther, 2015, 14(4): 1014-1023.DOI:10.1158/1535-7163.MCT-14-0669.
[17]Wang F, Li H, Yan XG, et al. Alisertib induces cell cycle arrest and autophagy and suppresses epithelial-to-mesenchymal transition involving PI3K/Akt/mTOR and sirtuin 1-mediated signaling pathways in human pancreatic cancer cells[J]. Drug Des Devel Ther, 2015, 9:575-601.DOI:10.2147/DDDT.S75221.
[18]Hasegawa S, Nagano H, Konno M, et al. A crucial epithelial to mesenchymal transition regulator, Sox4/Ezh2 axis is closely related to the clinical outcome in pancreatic cancer patients[J]. Int J Oncol, 2016, 48(1): 145-152.DOI:10.3892/ijo.2015.3258.
[19]Quint K, Tonigold M, Di Fazio P, et al. Pancreatic cancer cells surviving gemcitabine treatment express markers of stem cell differentiation and epithelial-mesenchymal transition[J]. Int J Oncol, 2012, 41(6): 2093-2102.DOI:10.3892/ijo.2012.1648.
(本文编辑:屠振兴)
Effects of glycogen synthase kinase3β silencing on cell growth and epithelial-mesenchymal transition in pancreatic cancer PANC1 cells
SongBo,MaHongyun,LiSeng,ShaoZhuo,SongBin,HaoJun,ChenPeng,JinGang.DepartmentofGeneralSurgery,ChanghaiHospital,SecondMilitaryMedicalUniversity,Shanghai200433,China
【Abstract】ObjectiveTo study the effect of inhibiting glycogen synthase kinase3β (GSK3β) on cell proliferation and epithelial mesenchymal transition (EMT) in pancreatic cancer PANC1 cells. MethodsThe siRNA trageting GSK3β(siRNA-GSK3β) and negative control siRNA (siRNA-NC) were synthesized to transfect pancreatic cancer PANC1 cells. MTT assay was used to detect cell proliferation. mRNA expression of Wnt, β-catenin, C-myc, CyclinD1 in Wnt/β-catenin signaling, Shh and Smo in Hedgehog pathway, PI3K, Akt, mTOR, 4E-BP1, p70S6K in PI3K/Akt/mTOR signal pathway and Slug, Snail, Twist, E-cadherin, N-cadherin, Vimentin involved in EMT were detected by RT-PCR. ResultsGSK3β mRNA expression was 1in cells transfected with siRNA-NC, which was 0.25±0.08, 0.62±0.09, 0.70±0.11 in cells with 3 different siRNA-GSK3βs, respectively. GSK3β mRNA was significantly decreased by transfection of siRNA-GSK3β(P<0.0001). The cell proliferation of siRNA-GSK3β group was significantly lower than that of siRNA-NC group(P<0.05). Wnt, β-catenin, C-myc, CyclinD1, PI3K, Akt, mTOR, 4E-BP1, p70S6K, Slug, Snail, N-cadherin, Vimentin mRNA in cells transfected with siRNA-GSK3β was 0.28±0.04, 0.47±0.05, 0.37±0.05, 0.62±0.08, 0.22±0.03, 0.47±0.06, 0.65±0.08, 0.39±0.04, 0.56±0.07, 0.33±0.05, 0.46±0.07, 0.55±0.06, 0.38±0.04, which were greatly lower than those in cells transfected with siRNA-NC, and the difference was statistically significant (all P<0.05). Shh and Smo mRNA was 1.10±0.13 and 1.05±0.11, which was comparable with those in cells with siRNA-NC. Twist mRNA was 0.62±0.08, which was lower than that in cells with siRNA-NC, while E-cadherin mRNA was 2.12±0.25, which was higher than that in cells with siRNA-NC, but the differences were not statistically significant. ConclusionsGSK3β silencing in PANC1 cells can suppress cell proliferation and EMT of pancreatic cancer cells by regulating Wnt/β-catenin and PI3K/Akt pathway.
【Key words】Pancreatic neoplasms;Glycogen synthase kinase 3β;Cell proliferation;Epithelial mesenchymal transition
(收稿日期:2016-01-06)
Corresponding author:Jin Gang, Email:jin_gang@outlook.com
通信作者:金钢,Email:jin_gang@outlook.com
DOI:10.3760/cma.j.issn.1674-1935.2016.02.002

