Optimalantiarrhythmic drug therapy for electricalstorm
Dan Sorajja,Thomas M.Munger,Win-Kuang Shen
Division of Cardiovascular Diseases,Mayo Clinic Arizona,Phoenix,AZ 85054,USA.
Optimalantiarrhythmic drug therapy for electricalstorm
Dan Sorajja✉,Thomas M.Munger,Win-Kuang Shen
Division of Cardiovascular Diseases,Mayo Clinic Arizona,Phoenix,AZ 85054,USA.
Electrical storm,defined as 3 or more separate episodes of ventricular tachycardia or ventricular fibrillation within 24 hours,carries significant morbidity and mortality.These unstable ventricular arrhythmias have been described with a variety of conditions including ischemic heartdisease,structuralheartdisease,and genetic conditions.While implantable cardioverterdefibrillatorimplantation and ablation may be indicated and required,antiarrhythmic medication remains an importantadjunctive therapy for these persons.
antiarrhythmic medication,electrical storm,ventricular tachycardia,ventricular fibrillation
Introduction
Electricalstorm(ES),which is recurrentventricular tachycardia(VT)or ventricular fibrillation(VF),is a life-threatening arrhythmic event with significant morbidity and mortality[1-4].Definitions vary for ES, with prior studies using 2 episodes of ventricular tachyarrhythmias within 24 hours[5,6].More typically, the definition for ES includes 3 or more separate episodes of ventricular tachyarrhythmias,whether untreated or treated with anti-tachycardia pacing or shocks(Fig.1)[7-9].Hemodynamic instability is not required to be associated with ES.Patients can have palpitations,lightheadedness,and/orsyncope.Inappropriate implantable cardioverterdefibrillator(ICD)shocks are notconsidered as ES.Some definitions of ES use a time delineation between episodes,such asbeing atleast 5 minutes apart or having 2 episodes within 1 hour[1,10]. Incessant VT,which is defined as a recurrence ofventricular tachyarrhythmia within 5 minutes of termination ofa previousepisode,can be considered an ES[5,11].
Epidemiology of electrical storm
Ischemia or worsening ofheartfailure predominates as the etiology in adults,while congenitalheartdisease and primary electrical disease are more common in children,who have a significantly lower frequency of ES overall compared to adults[1,2,7,8,12-15].Common and uncommon causes of ES are listed in Table 1. Factors related to worsening coronary artery disease and heartfailure,such asage,male gender,and leftventricularejection fraction,are risk factors for ES[2].
Additional factors that can precipitate ES include medication change(particularly use of class I antiarrhythmic medications,worsening congestive heart failure,lower ejection fraction,psychologicalstress, and alcohol;however the majority of triggers remain unknown[3,16-18].It has been reported that one predictor of ES is the co-presence ofsustained ST-segmentelevation and abnormalQwavesin≥2 ECGleadsin patients with structuralheartdisease[19].VF itself may be the culpritas itresults in intracellular calcium overloadrepeatedly initiating fibrillation and ES[20].These ventricular tachyarrhythmias and associated recurrent ICD shocks lead to adrenergic activation and heartfailure in a worsening spiralfashion[21].
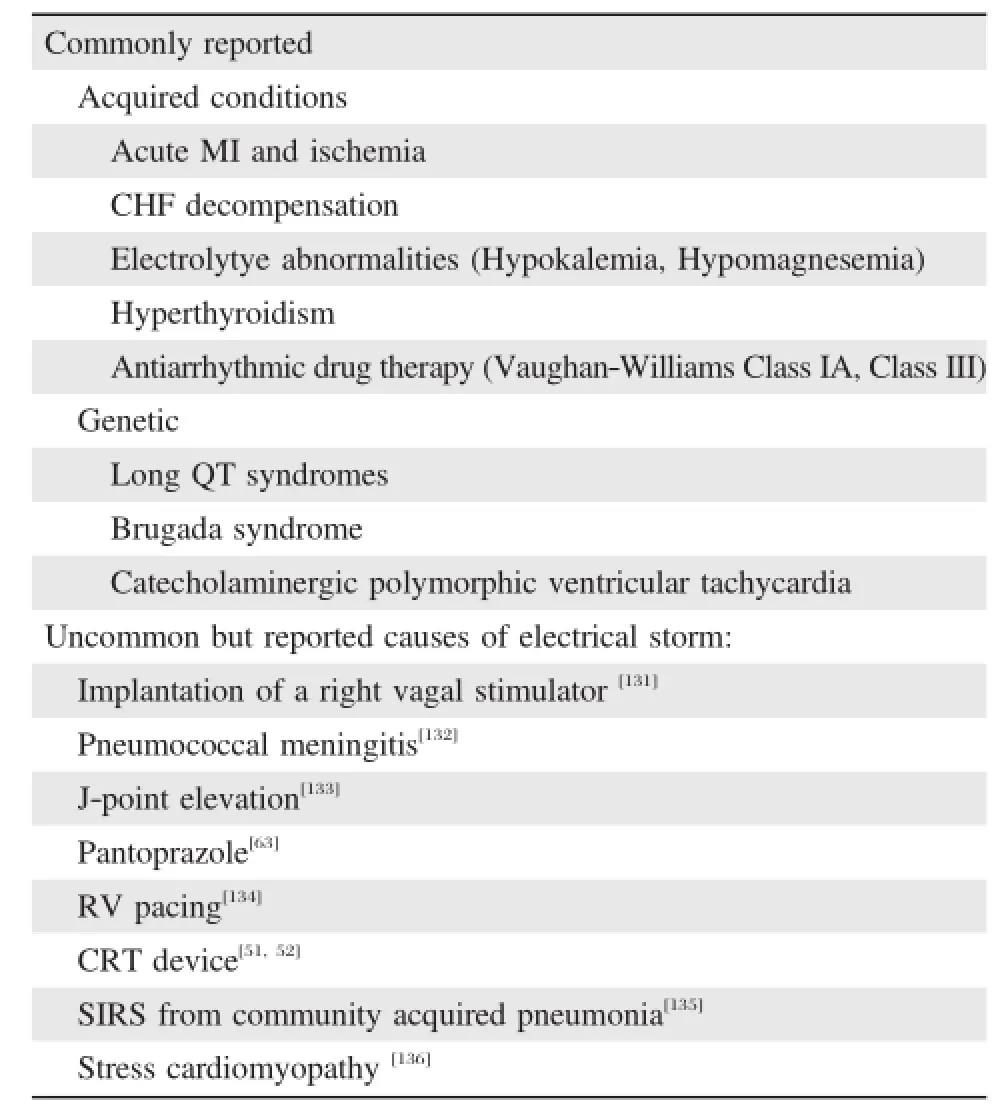
Table 1 Triggers of electrical storm
Circadian rhythm may play a role aswellasthere is a preponderance of ES during wintermonths(December, January,and February)and late afternoon similar to otherdata formyocardialinfarction and sudden cardiac death[15,17,22-25].
Substrates and mechanisms for ventricular tachyarrhythmias
Ventricular tachyarrhythmias can be grossly categorized based on electrocardiogram into 3 morphologies: monomorphic VT,polymorphic VT,and VF.Each of these is due to a pathophysiologic mechanism,in which a substrate is affected by a triggering event.
Monomorphic ventricular tachycardia
In monomorphic VT,the ventricularactivation morphology is the same on a beat-to-beatbasis,and most commonly is a reentrantelectricalwavefrontaround a fixed obstacle such as myocardialscar.Specific locationswithin the ventricleshave associated morphologies of ventricular tachyarrhythmias seen on electrocardiogram[26].Within or atthe border of these scar zones,slow conduction provides the necessary constructfor VT to sustain itself[27].Among episodes of ES,monomorphic VT comprises 77%ofthe cases[4].
Anotherform ofmonomorphic VT involvestriggered activity,usually in structurally normal hearts[28].These episodesof VT are usually self-limited,and uncommonly cause ES.Re-entry involving the His-Purkinje system in patients with cardiomyopathy or conduction system disease can resultin bundle-branch reentranttachycardia, usually with a leftbundle branch block morphology[29]. Another less common monomorphic VT is ventricular flutter,which isquite rapid with a cycle length ofapproximately 200 ms[30].
Polymorphic ventricular tachycardia
On a beat-to-beatbasis,polymorphic VT has varying amplitude and/orduration ofthe QRS complex,and this typeofventricularactivation includestorsadesde pointes. Polymorphic VT can occurin patients with normaland prolonged QT intervals during sinus rhythm[31].Among ES cases,polymorphic VT comprises 7%ofcases[4].
Polymorphic VT occurring with a normalQT interval usually involvesischemic heartdisease ornon-ischemic cardiomyopathy.During acute myocardialinfarctions, 2 to 4%of patients develop polymorphic VT,butthis arrhythmia ismore common with coronary vasospasm[32]. In non-ischemic cases,hypertrophic cardiomyopathy and acute myocarditis can presentwith polymorphic VT[31].In addition,catecholaminergic polymorphic VT may present with polymorphic VT or bidirectional tachycardia with alternating QRS morphologies[33].
In patientswith prolonged QT on electrocardiogram, there is a risk for torsades de pointes(‘‘twisting of the points’’),a form ofpolymorphic VT.The QT prolongation may be genetic ormay be acquired.With congenital cases of polymorphic VT,the mechanism often involves an adrenergic trigger,such as exercise[34].The types of clinicaltriggersare variable and have been correlated with different genotypes of congenital Long QT Syndrome. For acquired cases,electrolyte abnormalities such as hypokalemia and hypomagnesemia increase the QT interval,but drug therapy for a large number of medical conditions,with or withoutelectrolyte abnormalities, more frequently is the cause.A fulllistof drugs that cause or are implicated in acquired QT prolongation can be found on the website,‘www.qtdrugs.org’.The triggering mechanism isdue to early-afterdepolarization type premature ventricular complexes occurring during thelengthened repolarization ofthe ventricle[35].Ashortlong RR intervalsequence(giving the name‘‘pausedependent’’),precipitating polymorphic VT is common when the initiation of the tachycardia is recorded[36].QTprolongation normally occurs with bradycardia[37].The QT intervalcould be prolonged furtherwith the concomitantuse of class IIIantiarrhythmic agents due to the drug-mediated reverse use-dependence propertieswhich resultin blockade ofthe rapid componentofthe delayed rectifierpotassium current(responsible for phase 2 and 3 depolarization)[38].
A specific subtype of ventricular tachyarrhythmias that should be mentioned is bidirectional VT,which displays a beat-to-beatalternans in the QRS morphology and/or axis,most notable in the frontal plane leads. While commonly associated as one of the arrhythmia manifestations of digitalis toxicity,bidirectional VT can also be seen in catecholaminergic VT[39].
Ventricular fibrillation
The appearance of VF includes rapid,irregular, undulating waveforms(usually faster than 200 ms)that are more disorganized than polymorphic VT.As VF persists,the fibrillation slows with waveforms also developing decreased amplitude preceding asystole[40,41]. VF storm comprises 11%of ES cases[4].
The mostcommon etiology of VF,particularly with ES,is ischemia.While VF during the initial 24 to 48 hours of myocardial infarction does not increase mortality risk[42],when ES occurswith VF,the mortality rates are exceedingly high,between 85%and 97%,even with defibrillation[43,44].VF is also the most commonly recorded during sudden cardiac arrest[45].Less frequent causes of VF include congenitalchannelopathies such as Brugada syndrome and catecholaminergic polymorphic VT[46].While rare,VF can occur from atrial fibrillation with rapid ventricularresponse degenerating into VF in cases of Wolff-Parkinson-White[47].
Prognosis of electrical storm
Management of electrical storm
Fora more comprehensive guideline fortreatmentof ventricular arrhythmias,the joint reportfrom American College of Cardiology,American Heart Association, and the European Society of Cardiology should be reviewed[30].An algorithm for acute management of ES is suggested in Figure 2.Advanced cardiac life support(ACLS)[55]should be initiated.As partof ACLS, defibrillation of hemodynamically unstable and symptomatic patients is required.Unless contraindicated, amiodarone IV bolus and infusion should be given in combination withβ-blocker bolus,which should be eitherpropranololormetoprololbolus.Sedation can also be an effective measure to rapidly suppressthe catecholamine excess thatfrequently drives ES.Identifying the etiology,particularly reversible causessuch asischemia, medication effect,heartfailure,orelectrolyte abnormalities should be evaluated,and electrophysiology consultation should be sought[30].If there are specific known diagnosesoretiologiesforan episode ofES,those should be targeted fortherapy on an individualbasis.Asummary of pharmacologic and non-pharmacologic therapy for acute management of ES is presented in Table 2.A management algorithm based on QRS morphology of theventriculartachyarrhythmiaissuggested in Figure 3.
For long-term treatment,ICDs are indicated for secondary prevention of SCD unless contraindications are present,butonly after the ventriculararrhythmia is suppressed and controlled in the acute setting[56,57]. ICDs do not prevent the actual recurrence of the tachyarrhythmia which occurs in more than 50%of this patientpopulation during 1-2 years of follow up. While ablation has been shown to reduce the burden of VT[16,58],antiarrhythmic medication remains the first line of therapy in the acute setting of ES and often isneeded to be an adjuncttherapy to reduce the burden of these ventricular tachyarrhythmias long-term.As is the case with acute therapy of ES,long term therapy should target triggers and etiologies to preventrecurrence. Table 3 includes suggested options for long-term antiarrhythmic medications and treatmentto preventrecurrence of ventricular tachyarrhythmias and to reduce ICD shocks(Table 3).
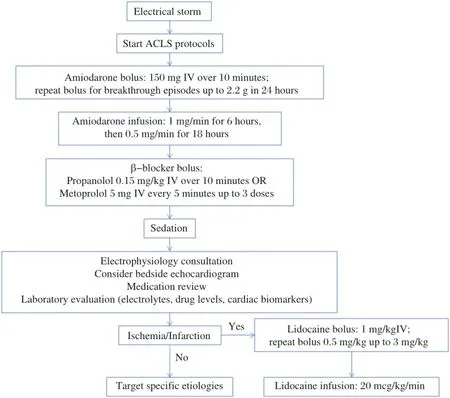
Fig.2 Acute management algorithm for electrical storm.ACLS:Advanced cardiac life support.
Anti-arrhythmic drugs β-blockers
Episodes of ES frequently are due to significant increases in sympathetic tone,and ES causes further heightening of sympathetic tone due to hemodynamic duress.Frequently ischemia and prior infarction can resultin elevated sympathetic tone due to denervation of sympathetic-parasympathetic fibers[57].β-blockade of bothβ1-andβ2-receptors remains an important treatment,which can reduce the risk of recurrent VT and VF by more than 50%[59],likely by increasing the threshold required for fibrillation[60].For patients with ES with a recent myocardial infarction,the use of β-blockade dramatically decreases the risk of sudden death compared to class I anti-arrhythmic medications[61].This effect correlates to prior data from acute myocardial infarction patients in theβ-blocker Heart Attack Trialin whichβ-blockerreduced mortality largely from prevention of ventricular tachyarrhythmias[62].For channelopathies,such as catecholaminergic polymorphic VT,β-blockade also is the mainstay oftreatment[7].
The benefits ofβ-blockade are largely a class effect, but there are differences with selective versus nonselectiveβ-blockers.Much of the data for reduction in VF during acute myocardial infarction was thought to be due to theβ1 receptors[63].Furtherdata has shown that in heart failure and post-infarction patients,the totalpopulation ofβ-receptors decreases,mainly due to down-regulation oftheβ1 receptor,whileβ2 receptors are preserved and thereby make up alargerproportion of the receptor density[63,64].In practice,propanololhas been shown to suppress ES thatis refractory to metoprololaswellas amiodarone[65].The effectin increasing the threshold required forfibrillation islargerwith more potentβ-blockers as well as with non-selectiveβblockers antagonizing bothβ1-andβ2-receptors[60].
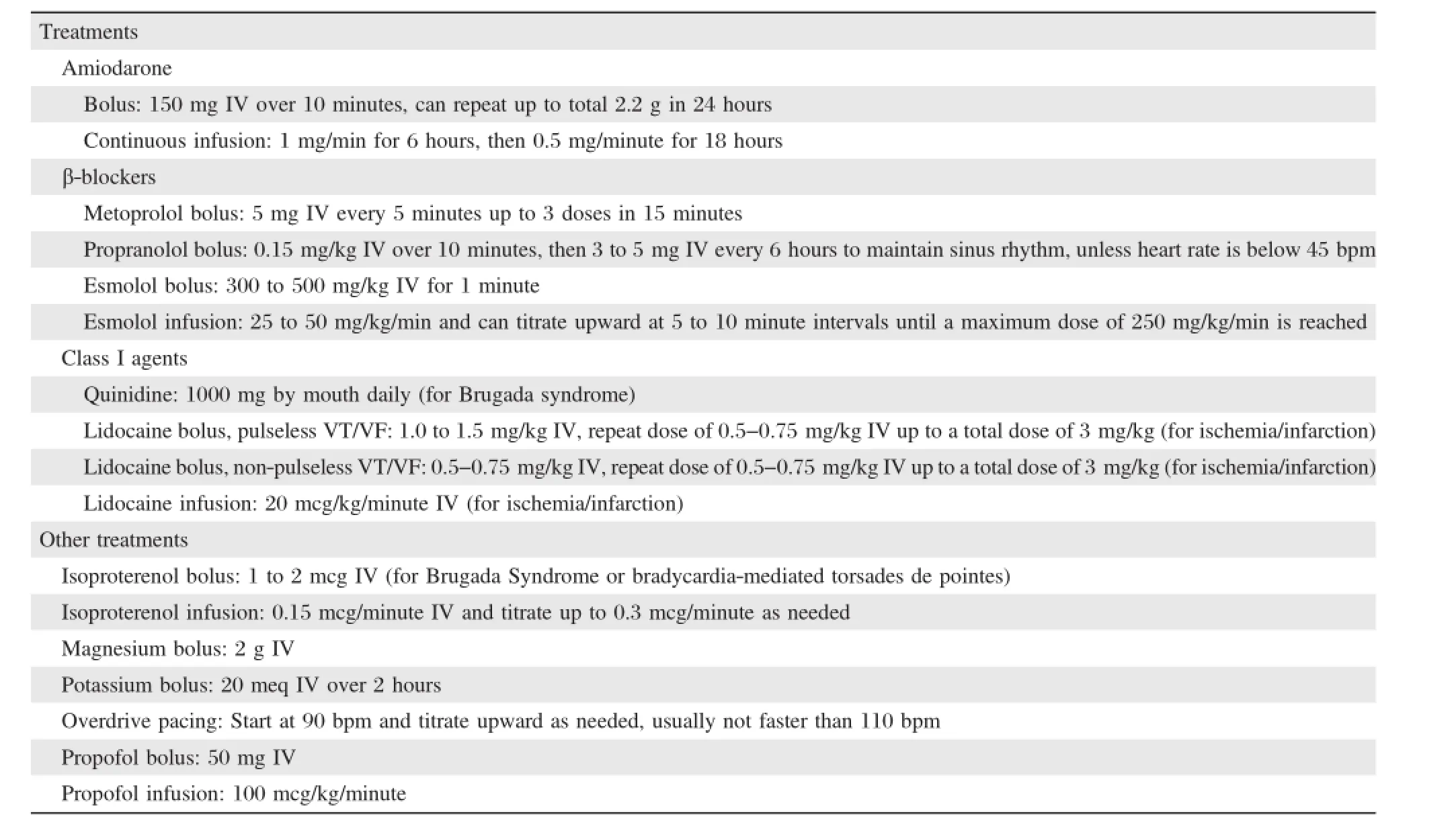
Table 2 Anti-arrhythmic medications and treatment for acute management of electrical storm
Amiodarone
Amiodarone has predominantly a Vaughan-Williams class IIIeffectofpotassium channelblockade resulting in lengthening ofthe cardiac action potential,leading to increased refractoriness of cardiac tissue.However, amiodarone also displays features of the other Vaughan William classes to a lesser degree,such as class I usedependentsodium channelblockade of inward sodium currents slowing the ventricularconduction,as wellas class IInon-competitive sympathetic blockade and class IV calcium channelblockade[66].The antiarrhythmic effects gradually build up due to slow distribution to tissue,and become maximal approximately 10 weeks after initiation[67].Recurrence of ventricular tachyarrhythmias during this loading phase does notpreclude long term effect and success of the medication to suppress these arrhythmias[66].
经肛门直肠癌局部切除术较经腹直肠癌根治术显著减小了手术创伤,有助于降低术中出血量,缩短手术时间,王锡山等[6-7]还认为局部切除能减少体液丢失,减小手术创伤对机体免疫功能的影响,同时减轻术后疼痛,缩短术后卧床时间,降低术后坠积性肺炎的发生,这对直肠癌患者术后早期恢复具有重要意义。另外,根治术中遵循TME原则,在游离系膜和肿瘤切除过程中可能损伤盆腔自主神经和盆底肌肉,造成术后性功能障碍[8]。而局部切除可有效保留盆底肌肉和盆腔自主神经,从而避免术后排便和性功能障碍的发生。本研究结果也证实上述观点。
The effectiveness of amiodarone has been seen in a number of studies on ventricular arrhythmias,and for this reason was chosen as the alternate therapy in the large secondary prevention trials,CIDS(Canadian Implantable Defibrillator Study),AVID(Antiarrythmics Versus Implantable Defibrillators),and CASH(Cardiac Arrest Study,Hamburg)[68-70].For acute controlof ES, amiodarone IV ata dose of 1 g per day is effective to suppress recurrent ventricular tachyarrhythmias[66].As a stand-alone medication,amiodarone effectively suppresses ventricular tachyarrhythmias in approximately 40%ofpatients within 24 hours of intravenous administration,even ifothermedicationsare unsuccessful[71,72]. In the OPTIC study(OptimalPharmacologicalTherapy in Cardioverter Defibrillator Patients),the use ofamiodarone combined withβ-blockers reduced the risk of ICD shock to 10.3%from 38.5%when onβ-blockers alone over the 1 year follow-up[73].Similar benefitwas seen in patients classified as receiving frequent ICD shocks(more than 10 ICD shocksperyear),with amiodarone plusβ-blockerhaving 1.4%incidence compared to 7.4%in patients onβ-blocker alone[73].In another cohortlooking in patients with prior ES,those patients on amiodarone had a recurrence ofES of12%compared to 53%in patients noton amiodarone over5-year follow-up[17].Using data from the Canadian Amiodarone Myocardial Infarction Arrhythmia Trial(CAMIAT) and European Myocardial Infarct Amiodarone Trial (EMIAT),amiodarone in addition toβ-blockers had a statistically signification reduction in antiarrhythmic death compared to those notonβ-blocker,suggesting a separate butadditive effectofthe medications[74].In patients with out-of-hospitalarrestresistantto shocks and stillin VT or VF,thosepatientswho received amiodarone showed improved survivalto hospitaladmission (44%versus 34%with placebo)[75],and this benefitpersisted when compared to lidocaine(28%versus 15%)to be admitted to a hospital[76].
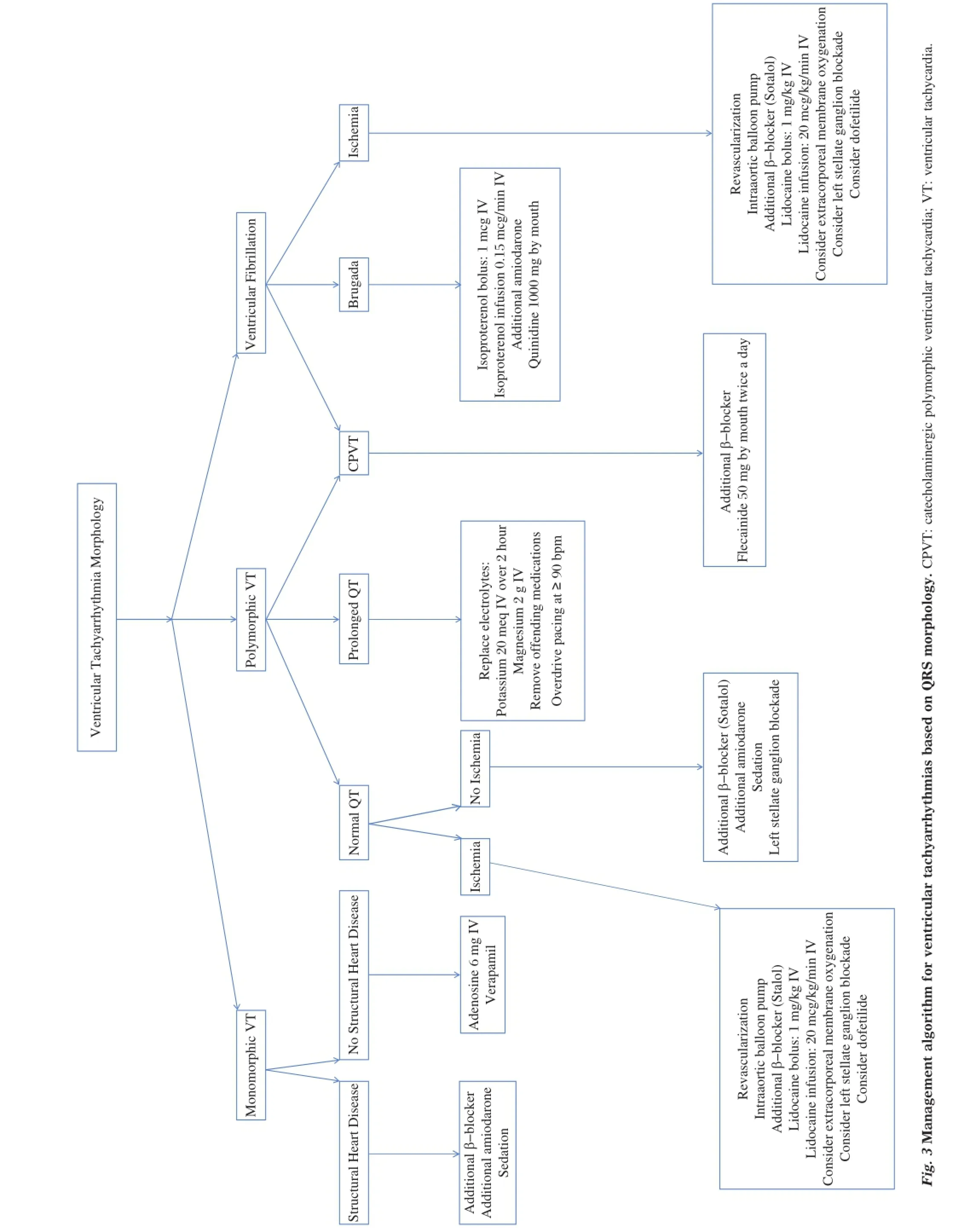
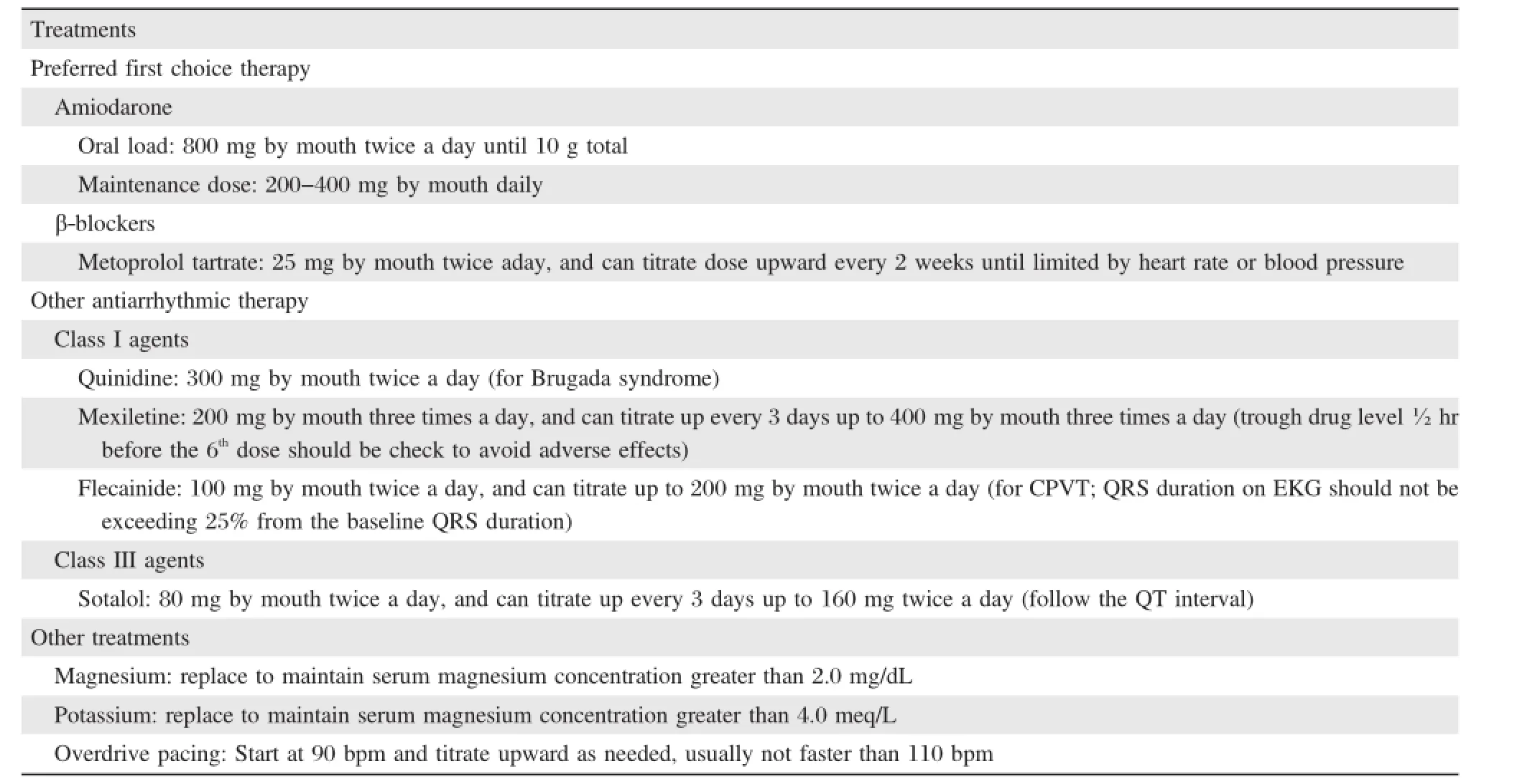
Table 3 Anti-arrhythmic medications and treatment for long-term treatment of electrical storm
Side effects from long term use of amiodarone are welldescribed.These include abnormalities seen in the thyroid,liver,lung,skin,and eye.In the CIDS trial, amiodarone-mediated side effects were reported in 82% of patients during 5.6 years of follow-up[77].Increased risk oftoxicity is associated with plasma concentrations>2.5 mg/L[78].Torsade de pointes with amiodarone is low,estimated to be less than 0.5%of cases,but QT prolongation does occur secondary to the potassiumchannelblocking effects[66].The defibrillation threshold can increase and defibrillation threshold testing is recommended forpatients on amiodarone[79,80].Intolerances to the amiodarone result in discontinuation of the medication in 23.5%ofpatients within 1 yearofinitiation oftherapy[73].Bradycardia usually manifests 2 to 4 weeks afterinitiation in 2.4%ofpatients,and would be addressed by ICD implantation in these patients with ES.[56,66].
Sotalol
Sotalolisa Vaughan-Williamsclass IIIantiarrhythmic, blocking the rapid componentof the delayed rectifier potassium current,IKr,resulting in prolongation of repolarization and therefore the QT interval but also exerts class IInon-selectiveβ-blocking effect[81].These separate effects are due to the d-and l-isomers which have class III and class II effects,respectively.
In patients who presentwith sustained VT,sotalol intravenously was able to terminate the arrhythmia within 15 minutesin 75%ofpatients[82].The intravenous form of sotalolis notavailable in the United States.In the OPTIC study,oralsotalolhad a lowerrisk of ICD shock(24.3%)vsβ-blockers(38.5%)during a followup of12 months,butthiswasnotstatistically significant (p=0.055)due to smallsample size[73].In the group of patients who received frequent ICD shocks,the incidence among patients on sotalol was 2.3%,while patients onβ-blocker alone carried an incidence of 7.4%[73].In another study ofpatients with ICD forsecondary prevention of SCD,sotalol(at 80 to 160 mg twice perday)reduced the frequency ofshocksperyear from 3.89 peryearto 1.43 peryear,regardless ofejection fraction[83].In a double-blind study thatincluded patients with sustained VT induced by programmed electricalstimulation atbaseline,34%ofpatientsplaced on sotalol(160 mg twice a day)were unable to have VT induced after sotalolloading[84].Over the subsequent yearoffollow-up on 26 patients,1 patienthad sustained VT and another patients was feltto have arrhythmic death from VF[84].These accumulated data supportthe currentrecommendation thatsotalolcan be helpfulin the treatment for sustained ventricular tachyarrythmias unresponsive toβ-blockers[30].Of note,in the Survivalwith Oral D-sotalol(SWORD)trial,a primary sudden death prevention study using the d-isomer alone,there was a significant increase in mortality likely from arrhythmias[85].Most likely,theβ-blocking effect of the l-isomerhas a protective effect.
Long term side effects remain a limitation of the medication,as 18-37%of patients stop sotalolwithin 1 year[73,84].In follow-up monitoring,sotalolhas been implicated in 17%ofthe reported casesofdrug-induced polymorphic VT[85,86].In patientswith renaldysfunction, depressed leftventricularejection fraction,orsignificant heartfailure,sotalolshould be avoided with preference given to amiodarone andβ-blockers[30,73].
Quinidine
Quinidine is a class 1A antiarrhythmic medication blocking the fast inward sodium current in a usedependentmanner,butalso blocks multiple potassium curents including the Ito,IKr,and IKs[87].Quinidine has been associated with increased proarrhythmic effects and increased mortality[88,89].In approximately 1.5% patients per year,torsades des pointes occurs resulting in‘‘quinidine syncope’’[90].
However,quinidine has proven effective in Brugada syndrome patients with inducible sustained ventricular tachyarrhythmia during electrophysiological study.In these patients,quinidine was able to render ventricular tachyarrhythmias noninducible in 96%of patients[91]. With the 4 Brugada patients in this study who tolerated quinidine,the medication prevented initiation of VF over a follow-up of 80 months[91].For patients in ES due to Brugada syndrome,quinidine also shows the ability to terminate these episodes[92].Another patient cohort that may potentially benefitfrom quinidine is short QT syndrome.In these patients who tolerate quinidine,VF was rendered non-inducible atelectrophysiological study[93].On a similar spectrum,early repolarization or J-wave syndrome may benefit from use of quinidine[94,95].
The use of quinidine in VT suppression has decreased significantly because of the frequent side effects.The mostcommon intolerance to quinidine is diarrhea,occurring in patients usually within several days of starting therapy.Other known common side effects include the drugsˊanticholinergic effects, resulting in urinary hesitancy.More worrisome adverse effects include thrombocytopenia,lupus-like syndrome,and cinchonism[96].
Lidocaine and mexiletine
Lidocaine and mexiletine are class IB antiarrhythmic medications,which display the class-effect of use-dependence forboth fastand slow sodium channel blockade.Structurally,the two medications are close analogues with the main difference between them being availability ofan oralformulation formexiletine[90].Use ofmexiletine has shown an ability to suppress the burden ofventricular ectopy[97,98],butwith a trend toward increased mortality[30].The main use of lidocaine for ventricular tachyarrhythmias is with ischemia,during which the medication is able to reduce the incidence of VF by approximately one third[99].
In several guidelines,the use of lidocaine has been the preferred antiarrhythmic medication with VF after out-of-hospitalcardiac arrest[100-102].However,the effect of lidocaine in shock-resistantout-of-hospitalcardiac arrestwas inferiorand less likely to survive to hospital admission when compared to those patients who received amiodarone[76].Thisfinding issimilarto smaller studies which showed worse resuscitation rates with lidocaine[103,104].
These data supportthe currentrecommendations of using lidocaine for the suppression of ventricular arrhythmias in the setting of acute myocardialinfarction or ischemia[30,57].Mexiletine can also be used as adjunctive long-term therapy with amiodarone after ES.Lidocaine and mexiletine may benefitpatients with type 3 long QT syndrome to preventrecurrenttorsades de pointes due to their slow sodium channel blockade effect,thereby shortening the QT interval[30,105,106].
Side effects of lidocaine and mexiletine are dosedependentand resolve with discontinuation ordecrease in drug dosing.Centralnervous system toxicity generally manifests as drowsiness and tremor,butgeneralized seizuresmay also occur.Adverse cardiac effects include bradycardia and asystole[107-109].
Flecainide
This class IC antiarrhythmic medication blocks cardiac sodium channels in use-dependent fashion,but also blocksthe rapid componentofthe delayed rectifier potassium current,IKr,as well as ryanodine receptors (RyR2),which release calcium from cardiac sarcoplasmic reticulum[110].
In the landmark Cardiac Arrhythmia Suppression Trial(CAST),patients with priormyocardialinfarction with ventricular ectopy were placed on flecainide resulting in excess mortality predominantly due to an arrhythmia[111].Some of this has been attributed to low utilization ofβ-blockersconcomitantly(26%usage among flecainide users)[111].In patients withoutstructuralheartdisease orcoronary artery disease,flecainide can be a reasonable addition to concomitantβ-blocker or calcium channel blocker therapy for ventricularectopy[112].In patients with catecholaminergic polymorphic VT,flecainide can be combined withβ-blockade resulting in a decrease in risk of ES after ICD shocks[110,113].
The mostcommon non-cardiac adverse effectfrom flecainide is blurred vision and dizziness.The proarrhythmia effectswere described above,butothercardiac effects include decreased leftventricular inotropy and possible worsening ofheartfailure[114,115].
Other therapy-non-pharmacologic Sedation
With ES frequently due to adrenergic stimulation, sedation is able to reduce this sympathetic tone[116]. Propofol,a short-acting generalanesthetic agentmediating itseffectwith gamma-aminobutyric acid receptors (GABA),hasbeen shown to inhibitsympathetic activity, and suppress refractory ES[117,118].
Extracorporealmembrane oxygenation(ECMO)
While predominantly indicated forcardiogenic shock, venoarterial extracorporeal membrane oxygenation has been used to treat ES related for myocardialischemia[119], myocarditis[120],and Brugada syndrome[121].ECMO maintains tissue perfusion,unloads the left ventricle, preserves coronary circulation,and likely results in decrease of catecholamine release by the individual[122].
Overdrive pacing
In patients who continue to have ES despite other medications and treatments,overdrive pacing can successfully prevent the arrhythmias[16,123,124].The suppression can be a temporizing measure while awaiting revascularization for ischemia or electrophysiology study and attempted catheter ablation,as the ES may return once the pacing ceases[16,123].In cases ofdigitalis toxicity,QT prolongation,and pause-dependent ES, temporary rightventricularpacing can also be effective[30]. Rightventricularpacing alone may notbe able to suppress ES,and reportofbiventricularpacing and wellas triple-sitebiventricularpacing hasshown to be successful in treating ES[124,125].
Left stellate ganglionic blockade
In patients with recent myocardial infarction or ongoing ischemia,leftstellate ganglionic blockade when combined with amiodarone improved survivalcompared to class 1 antiarrhythmic therapy by ACLS guidelines in one smallcohort of ES[61].Unilateralsympathetic denervation in some cases may be insufficientand require bilateral surgical sympathetic denervation[126].In cases where surgicalapproach is notavailable,percutaneous blockade ofthe stellate ganglion with bupivacaine has residual block lasting severalweeks and prevent ES recurrence[127].
Other therapy for selected conditionspharmacologic
Isoproterenol
While adrenergic stimulation triggers orworsens ES in many patients,select populations may benefit from it.Brugada syndrome patients have increased risk of ES from VF;isoproterenolin these patients suppresses ES likely due to augmentation of L-type calcium current[46,128].
Potassium
With hypokalemia identified as a trigger of ES[5,50], the effectis likely due to QT prolongation.Potassium supplementation should be instituted for ventricular arrhythmias whetherfrom diuretic use orother causes, with a goallevelbeing greaterthan 4.5 to 5 mmol/L[30].
Magnesium
Hypomagnesemia has been implicated in polymorphic ventricular ES and other episodes of polymorphic VT[129,130].Magnesium likely exerts its antiarrhythmic effect by antagonizing the L-type calcium channel,which is responsible for generating early afterdepolarization type during the plateau phase ofventricularaction potentials[129].Magnesium supplementation is beneficial in hypomagnesemia due to diuretics and in cases of VT secondary to digoxin toxicity[57].
Conclusions
ES consists of frequent episodes of ventricular tachyarrhythmias,which carry significant morbidity and mortality.The most common cause is ischemia, butevaluation of these patients at presentation should include assessment of other potential substrates and triggers such as worsening heart failure,medications,and genetic conditions.Initial treatment should include ACLS and stabilizing measures.Many patients with ES willrequire more definitive therapy, such as revascularization or ablation with an electrophysiology study,butapplication of optimalmedical therapy remains an importantadjunctive therapy.Use ofβ-blocker and amiodarone are cornerstones of therapy,but tailoring the treatment and antiarrhythmic therapy for the underlying condition and trigger is necessary.
[1]Exner DV,Pinski SL,Wyse DG,et al.Electrical storm presages nonsudden death:the antiarrhythmics versus implantable defibrillators(AVID)trial.Circulation 2001; 103(16):2066-2071.
[2]Gatzoulis KA,Andrikopoulos GK,Apostolopoulos T, et al.Electrical storm is an independent predictor of adverse long-term outcome in the era ofimplantable defibrillator therapy.Europace 2005;7(2):184-192.
[3]Guerra F,Shkoza M,Scappini L,et al.Role of electrical storm as a mortality and morbidity risk factorand its clinical predictors:a meta-analysis.Europace 2014;16(3):347-353.
[4]Nayyar S,Ganesan AN,Brooks AG,etal.Venturing into ventricular arrhythmia storm:a systematic review and meta-analysis.Eur Heart J 2013;34(8):560-571.
[5]Brigadeau F,Kouakam C,Klug D,etal.Clinical predictors and prognostic significance of electrical storm in patients with implantable cardioverter defibrillators.Eur Heart J 2006;27(6):700-707.
[6]Verma A,Kilicaslan F,Marrouche NF,et al.Prevalence, predictors,and mortality significance of the causative arrhythmia in patients with electrical storm.J Cardiovasc Electrophysiol 2004;15(11):1265-1270.
[7]Clausen H,Pflaumer A,KamberiS,etal.Electricalstorm in children.Pacing Clin Electrophysiol2013;36(3):391-401.
[8]Gao D,Sapp JL.Electrical storm:definitions,clinical importance,and treatment.Curr Opin Cardiol2013;28(1): 72-79.
[9]Kowey PR,Marinchak RA,Rials SJ,etal.Electrophysiologic testing in patients who respond acutely to intravenous amiodarone for incessant ventricular tachyarrhythmias. Am Heart J 1993;125(6):1628-1632.
[10]Fries R,Heisel A,Huwer H,et al.Incidence and clinical significance of short-term recurrent ventricular tachyarrhythmias in patients with implantable cardioverter-defibrillator.Int J Cardiol 1997;59(3):281-284.
[11]Scheinman MM,Levine JH,Cannom DS,et al.Doseranging study of intravenous amiodarone in patients with life-threatening ventricular tachyarrhythmias.The Intravenous Amiodarone Multicenter Investigators Group. Circulation 1995;92(11):3264-3272.
[12]Berul CI,Van Hare GF,Kertesz NJ,et al.Results of a multicenter retrospective implantable cardioverter-defibrillator registry of pediatric and congenital heart disease patients.J Am Coll Cardiol 2008;51(17):1685-1691.
[13]Dubin AM,Berul CI,Bevilacqua LM,et al.The use of implantable cardioverter-defibrillators in pediatric patients awaiting heart transplantation.J Card Fail 2003;9(5): 375-379.
[14]Stefanelli CB,Bradley DJ,Leroy S,et al.Implantable cardioverter defibrillator therapy for life-threatening arrhythmias in young patients.J Interv Card Electrophysiol 2002;6(3):235-244.
[15]Wood MA,Simpson PM,Stambler BS,et al.Long-term temporal patterns of ventricular tach yarrhy thmias. Circulation 1995;91(9):2371-2377.
[16]Bansch D,Oyang F,Antz M,et al.Successful catheter ablation of electrical storm after myocardial infarction. Circulation 2003;108(24):3011-3016.
[17]Greene M,Newman D,Geist M,et al.Is electrical storm in ICD patients the sign of a dying heart?Outcome of patients with clusters of ventricular tachyarrhythmias. Europace 2000;2(3):263-269.
[18]Huang DT,Traub D.Recurrent ventricular arrhythmia storms in the age of implantable cardioverter defibrillator therapy:a comprehensive review.Prog Cardiovasc Dis 2008;51(3):229-236.
[19]Furushima H,Chinushi M,Iijima K,et al.Is the coexistence of sustained ST-segment elevation and abnormal Q waves a risk factor for electrical storm in implanted cardioverter defibrillator patients with structural heart diseases?Europace 2012;14(5):675-681.
[20]Zaugg CE,Wu ST,Barbosa V,etal.Ventricular fibrillation-induced intracellular Ca2+overload causes failed electrical defibrillation and post-shock reinitiation of fibrillation.J Mol Cell Cardiol 1998;30(11):2183-2192.
[21]Runsio M,Bergfeldt L,Brodin LA,et al.Left ventricular function after repeated episodes of ventricular fibrillation and defibrillation assessed by transoesophageal echocardiography.Eur Heart J 1997;18(1):124-131.
[22]Anderson TW,Le Riche WH.Cold weather and myocardial infarction.Lancet 1970;1(7641):291-296.
[23]Cohen MC,Rohtla KM,Lavery CE,etal.Meta-analysis of the morning excess ofacute myocardialinfarction and sudden cardiac death.Am J Cardiol1997;79(11):1512-1516.
[24]Marchant B,Ran jadayalan K,Steven son R,et al. Circadian and seasonal factors in the pathogenesis of acute myocardialinfarction:the influence ofenvironmental temperature.Br Heart J 1993;69(5):385-387.
[25]Muller JE,Ludmer PL,Willich SN,etal.Circadian variation in the frequency of sudden cardiac death.Circulation 1987;75(1):131-138.
[26]Miller JM,MarchlinskiFE,Buxton AE,etal.Relationship between the 12-lead electrocardiogram during ventricular tachycardia and endocardial site of origin in patients with coronary artery disease.Circulation 1988;77(4):759-766.
[27]Soejima K,Stevenson WG,Maisel WH,etal.Electrically unexcitable scar mapping based on pacing threshold for identification of the reentry circuit isthmus:feasibility for guiding ventricular tachycardia ablation.Circulation 2002;106(13):1678-1683.
[28]Kim RJ,IwaiS,Markowitz SM,etal.Clinicaland electrophysiological spectrum of idiopathic ventricular outflow tract arrhythmias.J Am Coll Cardiol 2007;49(20):2035-2043.
[29]Blanck Z,Dhala A,Deshpande S,etal.Bundle branch reentrant ventricular tachycardia:cumulative experience in 48 patients.J Cardiovasc Electrophysiol1993;4(3):253-262.
[30]European Heart Rhythm A,Heart Rhythm S,Zipes DP, et al.ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death:a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines(Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death).J Am Coll Cardiol2006;48(5):e247-346.
[31]Viskin S,Belhassen B.Polymorphic ventricular tachyarrhythmias in the absence of organic heart disease:classification,differential diagnosis,and implications for therapy.Prog Cardiovasc Dis 1998;41(1):17-34.
[32]Wolfe CL,Nibley C,Bhandari A,et al.Polymorphous ventricular tachycardia associated with acute myocardial infarction.Circulation 1991;84(4):1543-1551.
[33]Richter S,Gebauer R,Hindricks G,et al.A classic electrocardiographic manifestation of catecholaminergic polymorphic ventricular tachycardia.J Cardio vasc Electrophysiol 2012;23(5):560.
[34]Takenaka K,Ai T,Shimizu W,et al.Exercise stress test amplifies genotype-phenotype correlation in the LQT1 and LQT2 forms of the long-QT syndrome.Circulation 2003;107(6):838-844.
[35]El-Sherif N.Mechanism of ventricular arrhythmias in the long QT syndrome:on hermeneutics.J Cardiovasc Electrophysiol 2001;12(8):973-976.
[36]Jackman WM,Friday KJ,Anderson JL,et al.The long QT syndromes:a critical review,new clinical observations and a unifying hypothesis.Prog Cardiovasc Dis 1988;31(2):115-172.
[37]Hondeghem LM,Snyders DJ.Class III antiarrhythmic agents have a lot of potential but a long way to go. Reduced effectiveness and dangers of reverse use dependence.Circulation 1990;81(2):686-690.
[38]Yang T,Roden DM.Extracellularpotassium modulation of drug block of IKr.Implications for torsade de pointes and reverse use-dependence.Circulation 1996;93(3):407-411.
[39]Priori SG,Napolitano C,Memmi M,et al.Clinical and molecular characterization of patients with catecholaminergic polymorphic ventricular tachycardia.Circulation 2002;106(1):69-74.
[40]Umapathy K,Foomany FH,Dorian P,et al.Real-time electrogram analysis for monitoring coronary blood flow during human ventricular fibrillation:implications for CPR.Heart Rhythm 2011;8(5):740-749.
[41]Valderrabano M.Deciphering the electrogram in ventricular fibrillation to extract physiological information. Heart Rhythm 2011;8(5):750-751.
[42]Liberthso n RR,Nag el EL,Hirsch man JC,et al. Prehospital ventricular defibrillation.Prognosis and follow-up course.N Engl J Med 1974;291(7):317-321.
[43]Herlitz J,Bang A,Holmberg M,et al.Rhythm changes during resuscitation from ventricular fibrillation in relation to delay until defibrillation,number of shocks delivered and survival.Resuscitation 1997;34(1):17-22.
[44]Windecker S.Percutaneous left ventricular assist devices for treatment of patients with cardiogenic shock.Curr Opin Crit Care 2007;13(5):521-527.
[45]Bayes de Luna A,Coumel P,Leclercq JF.Ambulatory sudden cardiac death:mechanisms of production of fatal arrhythmia on the basis of data from 157 cases.Am Heart J 1989;117(1):151-159.
[46]Ohgo T,Okamura H,Noda T,et al.Acute and chronic management in patients with Brugada syndrome associated with electrical storm of ventricular fibrillation. Heart Rhythm 2007;4(6):695-700.
[47]Timmermans C,Smeets JL,Rodriguez LM,etal.Aborted sudden death in the Wolff-Parkinson-White syndrome. Am J Cardiol 1995;76(7):492-494.
[48]Hariman RJ,Hu DY,GallasteguiJL,etal.Long-term follow-up in patients with incessant ventricular tachycardia. Am J Cardiol 1990;66(10):831-836.
[49]Bansch D,Bocker D,Brunn J,etal.Clusters of ventricular tachycardias signify impaired survival in patients with idiopathic dilated cardiomyopathy and implantable cardioverter defibrillators.J Am Coll Cardiol2000;36(2):566-573.
[50]Credner SC,Klingenheben T,Mauss O,et al.Electrical storm in patients with transvenous implantable cardioverter-defibrillators:incidence,management and prognostic implications.J Am Coll Cardiol 1998;32(7):1909-1915.
[51]Nayak HM,Verdino RJ,Russo AM,et al.Ventricular tachycardia storm after initiation of biventricular pacing: incidence,clinical characteristics,management,and outcome.J Cardiovasc Electrophysiol 2008;19(7):708-715.
[52]Shukla G,Chaudhry GM,Orlov M,etal.Potentialproarrhythmic effect of biventricular pacing:fact or myth? Heart Rhythm 2005;2(9):951-956.
[53]Gasparini M,Lunati M,Landolina M,et al.Electrical storm in patients with biventricular implantable cardioverter defibrillator:incidence,predictors,and prognostic implications.Am Heart J 2008;156(5):847-854.
[54]Sesselberg HW,Moss AJ,McNitt S,et al.Ventricular arrhythmia storms in postinfarction patients with implantable defibrillators for primary prevention indications:a MADIT-II substudy.Heart Rhythm 2007;4(11):1395-1402.
[55]Aehlert B.ACLS Study Guide.4th ed.St.Louis:Elsevier 2012,402.
[56]Epstein AE,DiMarco JP,Ellenbogen KA,et al.2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities:a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society.J Am Coll Cardiol 2013;61(3):e6-75.
[57]Zipes DP.Influence of myocardial ischemia and infarction on autonomic innervation of heart.Circulation 1990;82(4):1095-1105.
[58]Marrouche NF,Verma A,Wazni O,etal.Mode of initiation and ablation of ventricular fibrillation storms in patients with ischemic cardiomyopathy.J Am Coll Cardiol 2004;43(9):1715-1720.
[59]Moss AJ,Zareba W,Hall WJ,etal.Prophylactic implantation ofa defibrillator in patients with myocardialinfarction and reduced ejection fractio n.N En gl J Med 2002;346(12):877-883.
[60]Anderson JL,RodierHE,Green LS.Comparative effects of beta-adrenergic blocking drugs on experimentalventricular fibrillation threshold.Am J Cardiol1983;51(7):1196-1202.
[61]Nademanee K,Taylor R,Bailey WE,etal.Treating electrical storm:sympathetic blockade versus advanced cardiac life support-guided therapy.Circulation 2000;102(7): 742-747.
[62]A randomized trial of propranolol in patients with acute myocardial infarction.I.Mortality results.JAMA 1982; 247(12):1707-1714.
[63]Billman GE,Castillo LC,Hensley J,etal.Beta2-adrenergic receptor antagonists protectagainstventricular fibrillation: in vivo and in vitro evidence for enhanced sensitivity to beta2-adrenergic stimulation in animals susceptible to sudden death.Circulation 1997;96(6):1914-1922.
[64]Bristow MR,Ginsburg R,Umans V,et al.Beta 1-and beta 2-adrenergic-receptor subpopulations in nonfailing and failing human ventricular myocardium:coupling ofboth receptor subtypes to muscle contraction and selective beta 1-receptor down-regulation in heart failure.Circ Res 1986;59(3):297-309.
[65]Tsagalou EP,Kanakakis J,Rokas S,etal.Suppression by propranololand amiodarone of an electricalstorm refractory to metoprolol and amiodarone.Int J Cardiol 2005; 99(2):341-342.
[66]Connolly SJ.Evidence-based analysis of amiodarone efficacy and safety.Circulation 1999;100(19):2025-2034.
[67]Mitchell LB,Wyse DG,Gillis AM,et al.Electropharmacology of amiodarone therapy initiation.Time courses of onset of electrophysiologic and antiarrhythmic effects.Circulation 1989;80(1):34-42.
[68]A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias.The Antiarrhythmics versus Implantable Defibrillators(AVID)Investigators. N Engl J Med 1997;337(22):1576-1583.
[69]Connolly SJ,Gent M,Roberts RS,et al.Canadian implantable defibrillator study(CIDS):a randomized trial of the implantable cardioverter defibrillator againstamiodarone.Circulation 2000;101(11):1297-1302.
[70]Kuck KH,Cappato R,Siebels J,etal.Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the Cardiac Arrest Study Hamburg(CASH).Circulation 2000;102(7):748-754.
[71]Chapman JR,Boyd MJ.Intravenous amiodarone in ventricular fibrillation.Br Med J(Clin Res Ed)1981;282(6268): 951-952.
[72]Levine JH,Massumi A,Scheinman MM,etal.Intravenous amiodarone forrecurrentsustained hypotensive ventricular tachyarrhythmias.Intravenous Amiodarone Multicenter Trial Group.J Am Coll Cardiol1996;27(1):67-75.
[73]Connolly SJ,Dorian P,Roberts RS,et al.Comparison of beta-blockers,amiodarone plus beta-blockers,or sotalol for prevention of shocks from implantable cardioverter defibrillators:the OPTIC Study:a randomized trial. JAMA 2006;295(2):165-171.
[74]Boutitie F,Boissel JP,Connolly SJ,et al.Amiodarone interaction with beta-blockers:analysis of the merged EMIAT(European Myocardial Infarct Amiodarone Trial)and CAMIAT(Canadian Amiodarone Myocardial Infarction Trial)databases.The EMIAT and CAMIAT Investigators.Circulation 1999;99(17):2268-2275.
[75]Kudenchuk PJ,Cobb LA,Copass MK,et al.Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricularfibrillation.N EnglJ Med 1999;341(12):871-878.
[76]Dorian P,Cass D,Schwartz B,etal.Amiodarone as compared with lidocaine for shock-resistantventricular fibrillation.N Engl J Med 2002;346(12):884-890.
[77]Bokhari F,Newman D,Greene M,etal.Long-term comparison of the implantable cardioverter defibrillator versus amiodarone:eleven-year follow-up of a subsetof patients in the Canadian Implantable Defibrillator Study(CIDS). Circulation 2004;110(2):112-116.
[78]Connolly SJ,Gupta RN,Hoffert D,et al.Concentration response relationships of amiodarone and desethylamiodarone.Am Heart J 1988;115(6):1208-1213.
[79]Jung W,Manz M,Pizzulli L,et al.Effects of chronic amiodarone therapy on defibrillation threshold.Am J Cardiol 1992;70(11):1023-1027.
[80]Vischer AS,Sticherling C,Kuhne MS,etal.Role ofdefibrillation threshold testing in the contemporary defibrillator patientpopulation.J Cardiovasc Electrophysiol 2013; 24(4):437-441.
[81]Sanguinetti MC,Jurkiewicz NK.Two components of cardiac delayed rectifier K+current.Differentialsensitivity to block by class III antiarrhythmic agents.J Gen Physiol 1990;96(1):195-215.
[82]Ho DS,Zecchin RP,Richards DA,et al.Double-blind trial of lignocaine versus sotalol for acute termination of spontaneous sustained ventricular tachycardia.Lancet 1994;344(8914):18-23.
[83]Pacifico A,Hohnloser SH,Williams JH,et al.Prevention of implantable-defibrillator shocks by treatment with sotalol.d,l-Sotalol Implantable Cardioverter-Defibrillator Study Group.N Engl J Med 1999;340(24):1855-1862.
[84]Boriani G,Lubinski A,Capucci A,et al.A multicentre, double-blind randomized crossover comparative study on the efficacy and safety of dofetilide vs sotalol in patients with inducible sustained ventricular tachycardia and ischaemic heart disease.European heart journal 2001;22(23):2180-2191.
[85]Waldo AL,Camm AJ,deRuyter H,etal.Effectofd-sotalol on mortality in patients with left ventricular dysfunction after recent and remote myocardial infarction.The SWORD Investigators.Survival With Oral d-Sotalol. Lancet 1996;348(9019):7-12.
[86]Yap YG,Camm AJ.Drug induced QT prolongation and torsades de pointes.Heart 2003;89(11):1363-1372.
[87]Paul AA,WitchelHJ,Hancox JC.Inhibition of the current of heterologously expressed HERG potassium channels by flecainide and comparison with quinidine,propafenone and lignocaine.Br J Pharmacol 2002;136(5):717-729.
[88]Lafuente-Lafuente C,Longas-Tejero MA,Bergmann JF, et al.Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation.Cochrane Database Syst Rev 2012;5:CD005049.
[89]Morganroth J,Goin JE.Quinidine-related mortality in the short-to-medium-term treatment of ventricular arrhythmias.A meta-analysis.Circulation 1991;84(5):1977-1983.
[90]Roden DM,Woosley RL,Primm RK.Incidence and clinical features of the quinidine-associated long QT syndrome:implications for patient care.Am Heart J 1986; 111(6):1088-1093.
[91]Belhassen B,Viskin S,Fish R,etal.Effects ofelectrophysiologic-guided therapy with Class IAantiarrhythmic drugs on the long-term outcome of patients with idiopathic ventricular fibrillation with or without the Brugada syndrome.J Cardiovasc Electrophysiol 1999;10(10):1301-1312.
[92]Mok NS,Chan NY,Chiu AC.Successfuluse ofquinidine in treatment of electrical storm in Brugada syndrome. Pacing Clin Electrophysiol 2004;27(6 Pt 1):821-823.
[93]Giustetto C,Schimpf R,Mazzanti A,et al.Long-term follow-up of patients with short QT syndrome.J Am Coll Cardiol 2011;58(6):587-595.
[94]Antzelevitch C,Yan GX.J wave syndromes.Heart Rhythm 2010;7(4):549-558.
[95]Sacher F,Derval N,Horlitz M,et al.J wave elevation to monitor quinidine efficacy in early repolarization syndrome.J Electrocardiol 2014;47(2):223-225.
[96]Cohen IS,Jick H,Cohen SI.Adverse reactions to quinidine in hospitalized patients:findings based on data from the Boston Collaborative Drug Surveillance Program. Prog Cardiovasc Dis 1977;20(2):151-163.
[97]Chamberlain DA,Jewitt DE,Julian DG,etal.Oral mexiletine in high-risk patients after myocardial infarction. Lancet 1980;2(8208-8209):1324-1327.
[98]Kerin NZ,Aragon E,Marinescu G,et al.Mexiletine. Long-term efficacy and side effects in patients with chronic drug-resistant potentially lethal ventricular arrhythmias.Arch Intern Med 1990;150(2):381-384.
[99]MacMahon S,Collins R,Peto R,etal.Effects of prophylactic lidocaine in suspected acute myocardial infarction. An overview of results from the randomized,controlled trials.JAMA 1988;260(13):1910-1916.
[100]Eisenberg MS,Mengert TJ.Cardiac resuscitation.N Engl J Med 2001;344(17):1304-1313.
[101]Guidelines for cardiopulmonary resuscitation and emergency cardiac care.Emergency Cardiac Care Committee and Subcommittees,American Heart Association.Part I. Introduction.JAMA 1992;268(16):2171-2183.
[102]Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.Part 6:advanced cardiovascular life support:section 5:pharmacology I:agents for arrhythmias.The American Heart Association in collaboration with the International Liaison Committee on Resuscitation.Circulation 2000;102(8 Suppl):I112-128.
[103]van Walraven C,Stiell IG,Wells GA,et al.Do advanced cardiac life supportdrugs increase resuscitation rates from in-hospital cardiac arrest?The OTAC Study Group.Ann Emerg Med 1998;32(5):544-553.
[104]Weaver WD,Fahrenbruch CE,Johnson DD,et al.Effect of epinephrine and lidocaine therapy on outcome after cardiac arrest due to ventricular fibrillation.Circulation 1990;82(6):2027-2034.
[105]Blaufo x AD,Tristan i-Firo uzi M,Seslar S,et al. Congenital long QT 3 in the pediatric population.Am J Cardiol 2012;109(10):1459-1465.
[106]Fazekas T,Krassoi I,Lengyel C,et al.Suppression of erythromycin-induced early afterdepolarizations and torsade de pointes ventricular tachycardia by mexiletine. Pacing Clin Electrophysiol 1998;21(1 Pt 2):147-150.
[107]DeToledo JC.Lidocaine and seizures.Ther Drug Monit 2000;22(3):320-322.
[108]Johansson BW,Stavenow L,Hanson A.Long-term clinical experience with mexiletine.Am Heart J 1984;107(5 Pt 2):1099-1102.
[109]Rademaker AW,Kellen J,Tam YK,et al.Character of adverse effects of prophylactic lidocaine in the coronary care unit.Clin Pharmacol Ther 1986;40(1):71-80.
[110]Leenhardt A,Denjoy I,Guicheney P.Catecholaminergic polymorphic ventricular tachycardia.Circ Arrhythm Electrophysiol 2012;5(5):1044-1052.
[111]Preliminary report:effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction.The Cardiac Arrhythmia Suppression Trial(CAST)Investigators.N Engl J Med 1989;321(6):406-412.
[112]Prystowsky EN,Padanilam BJ,Joshi S,et al.Ventricular arrhythmias in the absence of structural heart disease. J Am Coll Cardiol 2012;59(20):1733-1744.
[113]Watanabe H,Chopra N,Laver D,etal.Flecainide prevents catecholaminergic polymorphic ventricular tachycardia in mice and humans.Nat Med 2009;15(4):380-383.
[114]Gentzkow GD,Sullivan JY.Extracardiac adverse effects of flecainide.Am J Cardiol 1984;53(5):101B-105B.
[115]Pfisterer M.Negative inotropic effects of antiarrhythmic drugs:a clinical point of view.J Cardiovasc Pharmaco 1991;17 Suppl 6:S44-47.
[116]Molina PE.Opioids and opiates:analgesia with cardiovascular,haemodynamic and immune implications in critical illness.J Intern Med 2006;259(2):138-154.
[117]Burjorjee JE,Milne B.Propofol for electrical storm;a case reportofcardioversion and suppression ofventriculartachycardia by propofol.Can J Anaesth 2002;49(9):973-977.
[118]Mulpuru SK,Patel DV,Wilbur SL,et al.Electricalstorm and termination with propofoltherapy:a case report.Int J Cardiol 2008;128(1):e6-8.
[119]Ricciardi MJ,Moscucci M,Knight BP,et al.Emergency extracorporealmembrane oxygenation(ECMO)-supported percutaneous coronary interventions in the fibrillating heart.Catheter Cardiovasc Interv 1999;48(4):402-405.
[120]Tsai FC,Wang YC,Huang YK,et al.Extracorporeal life support to terminate refractory ventricular tachycardia. Crit Care Med 2007;35(7):1673-1676.
[121]Pagel PS,Lilly RE,Nicolosi AC.Use of ECMO to temporize circulatory instability during severe Brugada electrical storm.Ann Thorac Surg 2009;88(3):982-983.
[122]Brunner ME,Siegenthaler N,Shah D,etal.Extracorporeal membrane oxygenation supportas bridge to recovery in a patient with electrical storm related cardiogenic shock. Am J Emerg Med 2013;31(2):467 e461-466.
[123]Kurisu S,Inoue I,Kawagoe T,etal.Temporary overdriving pacing as an adjunct to antiarrhythmic drug therapy for electrical storm in acute myocardial infarction.Circ J 2005;69(5):613-616.
[124]Tanabe Y,Chinushi M,Washizuka T,etal.Suppression of electrical storm by biventricular pacing in a patient with idiopathic dilated cardiomyopathy and ventriculartachycardia.Pacing Clin Electrophysiol 2003;26(1 Pt 1):101-102.
[125]Itoh M,Yoshida A,Takei A,et al.Electrical storm after cardiac resynchronization therapy suppressed by triplesite biventricular pacing and atrioventricular nodal ablation.Heart Rhythm 2012;9(12):2059-2062.
[126]Ajijola OA,Lellouche N,Bourke T,et al.Bilateral cardiac sympathetic denervation for the management of electrical storm.J Am Coll Cardiol 2012;59(1):91-92.
[127]Hayase J,PatelJ,Narayan SM,etal.Percutaneous stellate ganglion block suppressing VT and VF in a patient refractory to VT ablation.J Cardiovasc Electrophysiol 2013;24(8):926-928.
[128]Watanabe A,Fukushima Kusano K,Morita H,etal.Lowdose isoproterenol for repetitive ventricular arrhythmia in patients with Brugada syndrome.Eur Heart J 2006; 27(13):1579-1583.
[129]Bibawy JN,Parikh V,Wahba J,et al.Pantoprazole(proton pump inhibitor)contributing to Torsades de Pointes storm.Circ Arrhythm Electrophysiol 2013;6(2):e17-19.
[130]Ramee SR,White CJ,Svinarich JT,etal.Torsade de pointes and magnesium deficiency.Am HeartJ 1985;109(1):164-167.
[131]Shalaby AA,El-Saed A,Nemec J,et al.Exacerbation of electrical storm subsequent to implantation of a right vagal stimulator.Clin Auton Res 2007;17(6):385-390.
[132]Lee YS,Han SW,Kim KS,et al.Incessant monomorphic ventricular tachycardia associated with pneumococcal meningitis:a case report.J Cardiol 2007;50(2): 135-139.
[133]Bastiaen en R,Hedley PL,Ch ristiansen M,et al. Therapeutic hypothermia and ventricularfibrillation storm in early repolarization syndro me.Hea rt Rh yth m 2010;7(6):832-834.
[134]Chiladakis JA,Spiroulias G,Koutsogiannis N,et al. Short-coupled variant of Torsade de Pointes as a cause of electrical storm and aborted sudden cardiac death: insights into mechanism and treatment.Hellenic journal ofcardiology:HJC=Hellenike kardiologike epitheorese 2008;49(5):360-364.
[135]Chia PL,Loh SY,Foo D.Ventricular tachycardia storm:a case series and literature review.Med J Malaysia 2012; 67(6):582-584.
[136]Olivotti L,Moshiri S,Nicolino A,et al.Stress cardiomyopathy and arrhythmic storm in a 14-year-old boy.J Cardiovasc Med 2010;11(7):519-521.
✉Corresponding author:Dan Sorajja,MD,Division of Cardiovascular Diseases,Mayo Clinic Arizona,5777 E Mayo Blvd,Phoenix,AZ 85054. Tel/Fax:(480)342-0239/(480)342-1606,E-mail:sorajja.dan@mayo.edu.
Received 14 November 2014,Accepted 05 December 2014,Epub 15 January 2015
The authors reported no conflict of interests.
©2015 by the Journal of Biomedical Research.All rights reserved.
10.7555/JBR.29.20140147
 THE JOURNAL OF BIOMEDICAL RESEARCH2015年1期
THE JOURNAL OF BIOMEDICAL RESEARCH2015年1期
- THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Myocardin in biology and disease
- Optimalprogramming managementofventricular tachycardia storm in ICD patients
- Trigger elimination ofpolymorphic ventricular tachycardia and ventricular fibrillation by catheter ablation:trigger and substrate modification
- Neuraxialmodulation for treatmentof VT storm
- Prevalence ofenteric pathogen-associated community gastroenteritis among kindergarten children in Gaza
- Portalvein arterialization promotes liver regeneration after extended partialhepatectomy in a rat model
