妊娠伴甲状腺功能减退症患者自然流产风险预测模型构建
彭任忠

【摘要】 目的:探讨妊娠伴甲状腺功能减退症患者自然流产的危险因素并构建预测模型,旨在为自然流产高危人群准确识别及早期干预提供更多指导。方法:回顾性纳入2018年1月—2023年1月于宜春市妇幼保健院就诊的妊娠伴甲状腺功能减退症患者共278例,根据是否发生自然流产分为自然流产组(n=40)和妊娠组(n=238)。采用单因素和多因素分析评估妊娠伴甲状腺功能减退症患者自然流产的独立危险因素,并基于独立危险因素构建偏回归系数模型方程式,分析该模型用于妊娠伴甲状腺功能减退症患者自然流产风险预测的临床效能。结果:单因素分析结果显示,两组糖化血红蛋白水平、甘油三酯水平、同型半胱氨酸(Hcy)水平、促甲状腺激素(TSH)水平及甲状腺过氧化物酶抗体(TPOAb)阳性比较,差异均有统计学意义(P<0.05)。logistic回归模型多因素分析结果显示,高糖化血红蛋白水平、高甘油三酯水平、高Hcy水平、高TSH水平及TPOAb阳性均是妊娠伴甲状腺功能减退症患者自然流产的独立危险因素(P<0.05)。根据logistic回归模型证实的妊娠伴甲状腺功能减退症患者自然流产的独立危险因素,构建自变量偏回归系数模型方程式:妊娠伴甲状腺功能减退症患者自然流产风险logit(Y)=1.68+1.63×糖化血紅蛋白(%)+1.85×甘油三酯(mmol/L)+1.48×Hcy(μmol/L)+0.60×TSH(mIU/L)+0.96×TPOAb阳性。受试者操作特征(ROC)曲线分析结果显示,上述临床模型用于妊娠伴甲状腺功能减退症患者自然流产风险预测的曲线下面积为0.90[95%CI(0.85,0.97)],最佳cut-off值为8.65,敏感度和特异度分别为86.15%、80.78%。结论:妊娠伴甲状腺功能减退症患者自然流产的发生与高糖化血红蛋白水平、高甘油三酯水平、高Hcy水平、高TSH水平及TPOAb阳性均有关,而基于上述指标构建的预测模型在指导临床医生早期准确识别自然流产高危人群方面显示出良好价值。
【关键词】 妊娠 甲状腺功能减退症 自然流产 危险因素 预测模型
Construction of Risk Forecasting Model for Spontaneous Abortion in Patients with Pregnancy Complicated with Hypothyroidism/PENG Renzhong. //Medical Innovation of China, 2024, 21(07): 150-154
[Abstract] Objective: To investigate the risk factors of spontaneous abortion in patients with pregnancy complicated with hypothyroidism and construct a forecasting model, in order to provide more guidance for accurate identification and early intervention of spontaneous abortion high-risk groups. Method: A total of 278 patients with pregnancy complicated with hypothyroidism treated in Yichun Maternal and Child Health Hospital from January 2018 to January 2023 were retrospectively included, and they were divided into spontaneous abortion group (n=40) and pregnancy group (n=238) according to whether spontaneous abortion occurred. Independent risk factors for spontaneous abortion in patients with pregnancy complicated with hypothyroidism were evaluated by univariate and multivariate analysis, and a partial regression coefficient model equation was constructed based on independent risk factors, and the clinical efficacy of this model in predicting spontaneous abortion risk in patients with pregnancy complicated with hypothyroidism was analyzed. Result: The results of single factor analysis showed that there were statistically significant differences in the levels of glycosylated hemoglobin, triglyceride, homocysteine (Hcy), thyroid stimulating hormone (TSH) and thyroid peroxidase antibody (TPOAb) positive between the two groups (P<0.05). Multivariate analysis results of logistic regression model showed that high levels of glycosylated hemoglobin, triglyceride, Hcy, TSH and TPOAb positive were independent risk factors of spontaneous abortion in patients with pregnancy complicated with hypothyroidism (P<0.05). According to the independent risk factors of spontaneous abortion in patients with pregnancy complicated with hypothyroidism confirmed by logistic regression model, the independent variable partial regression coefficient model equation was constructed: the spontaneous abortion risk of patients with pregnancy complicated with hypothyroidism logit (Y) =1.68+1.63×glycosylated hemoglobin (%) +1.85×triglyceride (mmol/L) +1.48×Hcy (μmol/L) +0.60×TSH (mIU) +0.96×TPOAb positive. Receiver operating characteristic (ROC) curve analysis results showed that the area under the curve of the above clinical model for predicting the risk of spontaneous abortion in patients with pregnancy complicated with hypothyroidism was 0.90 [95%CI (0.85, 0.97)], the optimal cut-off value was 8.65, and the sensitivity and specificity respectively was 86.15% and 80.78%. Conclusion: The occurrence of spontaneous abortion in patients with pregnancy complicated with hypothyroidism is associated with high glycosylated hemoglobin level, high triglyceride level, high Hcy level, low TSH level and TPOAb positive, and the forecasting model based on the above indicators shows good value in guiding clinicians to accurately identify high-risk groups of spontaneous abortion at an early stage.
[Key words] Pregnancy Hypothyroidism Spontaneous abortion Risk factors Forecasting model
First-author's address: Department of Obstetrics, Yichun Maternal and Child Health Hospital, Yichun 336000, China
doi:10.3969/j.issn.1674-4985.2024.07.034
甲状腺功能减退症是妊娠期常见合并症之一,包括临床和亚临床甲状腺功能减退症两类[1]。目前研究显示妊娠伴甲状腺功能减退症可影响胎儿神经智力发育,与妊娠结局不良关系密切,其中以自然流产最为常见[2-3]。以往有关妊娠伴甲状腺功能减退症与妊娠结局不良的报道较多,但不同研究间结论存在差异,且缺乏针对自然流产预测模型的报道[4-5]。基于以上证据,本研究回顾性纳入2018年
1月—2023年1月于宜春市妇幼保健院就诊的妊娠伴甲状腺功能减退症患者共278例,根据是否发生自然流产分组,探讨妊娠伴甲状腺功能减退症患者自然流产的危险因素并构建预测模型,旨在为自然流产高危人群准确识别及早期干预提供更多指导。
1 资料与方法
1.1 一般资料
纳入2018年1月—2023年1月于本院就诊的妊娠伴甲状腺功能减退症孕妇共278例。(1)纳入标准:①单胎妊娠;②尿人绒毛膜促性腺激素(hCG)阳性;③妊娠4~12周筛查证实有甲状腺功能减退症[6];④临床资料完整。(2)排除标准:①妊娠前存在内分泌系统疾病;②异位妊娠;③要求终止妊娠;④合并其他严重内外科疾病;⑤拒绝配合治疗或评估。根据妊娠28周内是否发生自然流产分为自然流产组(n=40)和妊娠组(n=238)。研究方案经本院医院伦理委员会批准。
1.2 方法
登录医院电子病历系统收集患者年龄、孕前体重指数、孕周、既往分娩情况、孕次、既往流产情况及实验室指标等资料。实验室指标包括糖脂代谢指标(空腹血糖、餐后2 h血糖、糖化血红蛋白、总胆固醇、甘油三酯、高密度脂蛋白胆固醇、低密度脂蛋白胆固醇)、甲状腺功能相关指标[促甲状腺激素(TSH)、游离三碘甲腺原氨酸(FT3)、游离甲状腺素(FT4)、同型半胱氨酸(Hcy)]及甲状腺过氧化物酶抗体(TPOAb)表达情况,上述指标均由本院检验科完成,其中TPOAb检测采用化学免疫发光法,检测试剂盒由中山汇康生物技术有限公司提供。随访至妊娠28周,记录自然流产情况,包括生化妊娠、难免流产、不全流产、完全流产及稽留流产。
1.3 统计学处理
采用SPSS 24.0软件处理数据。计量资料以(x±s)表示,比较采用t检验;计数资料以率(%)表示,比较采用字2检验法;多因素分析采用logistic回歸模型,将单因素分析中妊娠伴甲状腺功能减退症患者自然流产的影响因素纳入logistic回归模型,并根据自变量偏回归系数构建模型方程式,描绘受试者操作特征(ROC)曲线评估模型预测效能。P<0.05为差异有统计学意义。
2 结果
2.1 妊娠伴甲状腺功能减退症患者自然流产的单因素分析
单因素分析结果显示,两组糖化血红蛋白、甘油三酯、Hcy、TSH水平及TPOAb阳性比较,差异均有统计学意义(P<0.05),见表1。
2.2 妊娠伴甲状腺功能减退症患者自然流产多因素分析
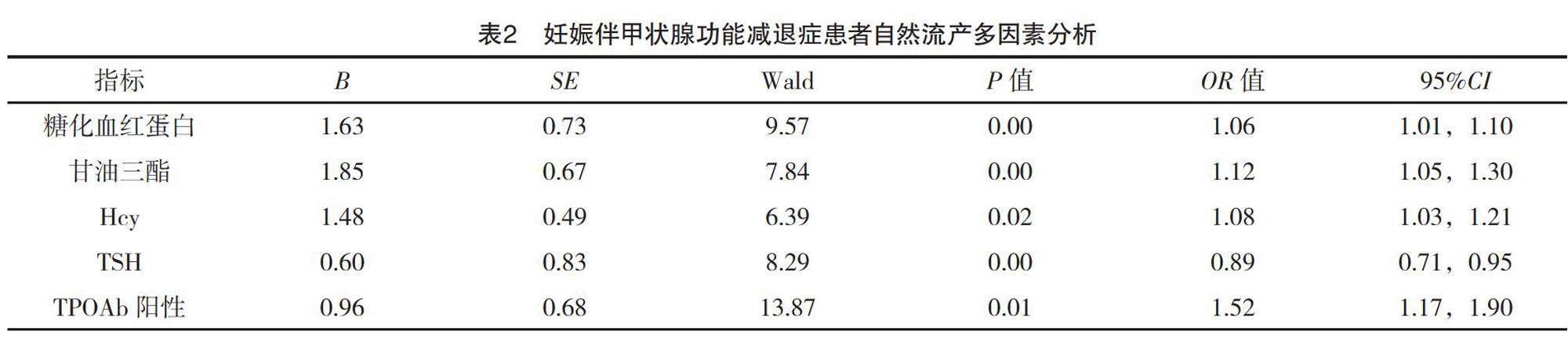
logistic回归模型多因素分析结果显示,高糖化血红蛋白水平、高甘油三酯水平、高Hcy水平、高TSH水平及TPOAb阳性均是妊娠伴甲状腺功能减退症患者自然流产的独立危险因素(P<0.05),见表2。
2.3 妊娠伴甲状腺功能减退症患者自然流产风险预测模型构建及预测效能分析
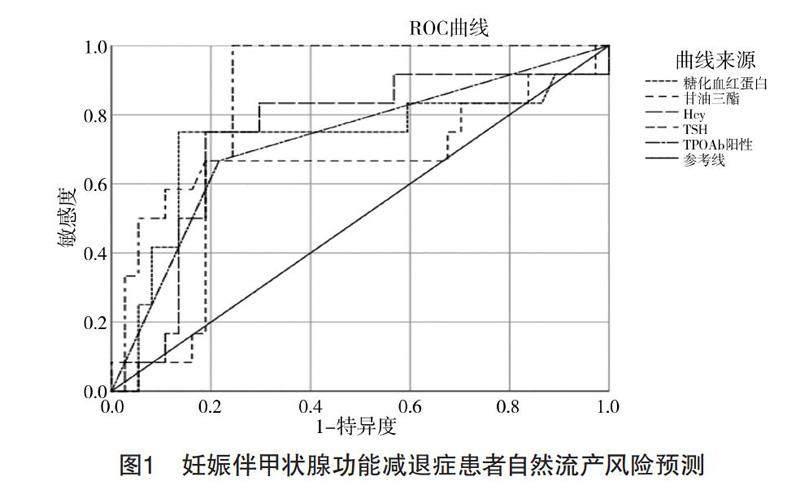
根据logistic回归模型证实的妊娠伴甲状腺功能减退症患者自然流产的独立危险因素,构建自变量偏回归系数模型方程式:妊娠伴甲状腺功能减退症患者自然流产风险logit(Y)=1.68+1.63×糖化血红蛋白(%)+1.85×甘油三酯(mmol/L)+1.48×Hcy(μmol/L)+0.60×TSH(mIU/L)+0.96×TPOAb阳性。ROC曲线分析结果显示,上述临床模型用于妊娠伴甲状腺功能减退症患者自然流产风险预测曲线下面积为0.90[95%CI(0.85,0.97)],最佳cut-off值为8.65,敏感度和特异度分别为86.15%、80.78%。见图1。
3 讨论
流行病学报道显示,妊娠伴甲状腺功能减退症发生率为0.3%~5.0%,其中以亚临床甲状腺功能减退症更为常见[7]。本研究纳入妊娠伴甲状腺功能减退症患者共278例中,出现自然流产40例,自然流产率发生率为14.39%,与以往报道结果相符[8]。进一步单因素和多因素分析结果证实,高糖化血红蛋白水平、高甘油三酯水平、高Hcy水平、高TSH水平及TPOAb阳性均是妊娠伴甲状腺功能减退症患者自然流产的独立危险因素。
以往研究提示,妊娠期女性糖脂代谢紊乱状态下可导致或加重血管壁损伤,影响胎盘血流灌注,导致胎盘供氧量降低及胎儿生长发育异常;而甲状腺功能减退持续可导致糖脂代谢紊乱问题加重,最终形成恶性循环[9-10]。本研究结果中,妊娠伴甲状腺功能减退症自然流产患者中,糖化血红蛋白及甘油三酯水平均更高,进一步支持以上观点。近年来研究提示Hcy可能参与到妊娠伴甲状腺功能减退症的发生发展过程中[11-12]。本研究结果证实高Hcy水平是妊娠伴甲状腺功能减退症患者自然流产的独立危险因素,笔者认为这可能与Hcy水平升高可造成胎盘血管床微血栓形成、胎盘血管局部梗死及蜕膜血管坏死等有关,进而导致胎盘血流灌注不足及胎盘功能受损[13-15]。
本研究結果还显示,高TSH水平及TPOAb阳性均可增加妊娠伴甲状腺功能减退症患者自然流产发生风险。已有研究显示,妊娠早期TSH水平升高可导致螺旋动脉侵入不足,影响子宫胎盘血液循环及胎盘发育,最终造成自然流产发生[16-17];亦有学者报道认为,女性自然流产与TSH水平升高有关,推测TSH水平变化可能干扰血清丙二醛及超氧化物歧化酶表达,导致脂质过氧化增加,从而增加自然流产风险[18]。TPOAb是自身免疫性甲状腺疾病中常见抗体之一,TPOAb阳性提示甲状腺存在明显炎症,加重机体免疫抑制状态,影响甲状腺储备功能,从而加重甲状腺功能损伤[19]。有报道提示,TPOAb阳性女性流产的风险往往更高,TPOAb阳性已被证实与流产及其他妊娠不良事件发生风险成正相关[20]。
确定妊娠伴甲状腺功能减退症患者自然流产危险因素并构建预测模型能够更精准指导临床医生早期识别自然流产高危人群,从而制订更为科学合理的预防干预方案,最大限度改善妊娠结局。既往研究显示,基于logistic回归模型自变量偏回归系数构建预测模型已被广泛用于临床良恶性病变罹患风险预测及预后评估,并显示出良好准确性及稳定性。本研究基于相关独立危险因素构建自变量偏回归系数模型方程式并进一步ROC曲线分析结果显示,上述临床模型用于妊娠伴甲状腺功能减退症患者自然流产风险预测曲线下面积为0.90[95%CI(0.85,0.97)],最佳cut-off值为8.65,敏感度和特异度分别为86.15%、80.78%,提示上述临床模型在妊娠伴甲状腺功能减退症患者自然流产风险预测方面显示出良好效能,考虑到相关指标临床较为常用,故更适合在基层医院推广应用。
综上所述,妊娠伴甲状腺功能减退症患者自然流产发生与高糖化血红蛋白水平、高甘油三酯水平、高Hcy水平、高TSH水平及TPOAb阳性均有关,而基于上述指标构建的预测模型在指导临床医生早期准确识别自然流产高危人群方面显示出良好价值。
参考文献
[1]唐萍,王其美.妊娠期亚临床甲减孕妇不同孕期TSH水平变化及对低出生体重儿的预测价值研究[J].中国妇产科临床杂志,2021,22(3):246-248.
[2] COOMARASAMY A,DHILLON-SMITH R K,PAPADOPOULOU A,
et al.Recurrent miscarriage: evidence to accelerate action [J].Lancet,2021,397(10285):1675-1682.
[3] LEE S Y,PEARCE E N.Testing, monitoring, and treatment of thyroid dysfunction in pregnancy[J].J Clin Endocrinol Metab,2021,106(3):883-892.
[4] DONG A C,MORGAN J,KANE M,et al.Subclinical hypothyroidism and thyroid autoimmunity in recurrent pregnancy loss: a systematic review and meta-analysis[J].Fertil Steril,2020,113(3):587-600.
[5] XU D,ZHONG H.Correlation between hypothyroidism during pregnancy and glucose and lipid metabolism in pregnant women and its influence on pregnancy outcome and fetal growth and development[J].Front Surg,2022,28(9):863286.
[6]《妊娠和产后甲状腺疾病诊治指南》(第2版)编撰委员会,中华医学会内分泌学分会,中华医学会围产医学分会.妊娠和产后甲状腺疾病诊治指南(第2版)[J].中华围产医学杂志,2019,22(8):505-506.
[7]胡静,王海宁,曾琳,等.孕早期双胎妊娠甲状腺功能减退对妊娠结局的影响[J].中国妇产科临床杂志,2022,23(3):228-231
[8] LEDUC-ROBERT G,IEWS M,ABDELKAREEM A O,et al.
Prevalence of thyroid autoimmunity and effect of Levothyroxine treatment in a cohort of 1064 patients with recurrent pregnancy loss[J].Reprod Biomed Online,2020,40(4):582-592.
[9] CIGROVSKI BERKOVI? M,HERMAN MAHE?I? D,MARINKOVI? RADO?EVI? J,et al. Hypothyroidism and pregnancy: still a controversial issue[J].Gynecol Endocrinol,2020,36(9):776-780.
[10] DHILLON-SMITH R K,TOBIAS A,SMITH P P,et al.The prevalence of thyroid dysfunction and autoimmunity in women with history of miscarriage or subfertility [J].J Clin Endocrinol Metab,2020,105(8):302-310.
[11] JANSEN S,LEDUC-ROBERT G,ABDELHAFEZ F F,et al.
Temporal trends in thyroid-stimulating hormone and live birth rate in subclinical hypothyroid patientss in a recurrent pregnancy loss population [J].Eur J Obstet Gynecol Reprod Biol,2022,277(10):21-26.
[12] DONNAY S,FAJARDO C,FERN?NDEZ-GARC?A J C,
et al.Diagnosis, treatment, and management of gestational hypothyroidism. The TIROGEST study[J].Endocrinol Diabetes Nutr (Engl Ed),2020,67(1):36-42.
[13] LI M,HE Y,MAO Y,et al.Preconception thyroid-stimulating hormone levels and adverse pregnancy outcomes[J].Clin Endocrinol (Oxf),2022,97(3):339-346.
[14] KN?SGAARD L,ANDERSEN S,HANSEN A B,et al.
Maternal hypothyroidism and adverse outcomes of pregnancy[J].Clin Endocrinol (Oxf),2023,98(5):719-729.
[15] CARVALHO B R,N?CUL A P,BENETTI-PINTO C L,et al.
Reproductive outcomes in cases of subclinical hypothyroidism and thyroid autoimmunity: a narrative review[J].Rev Bras Ginecol Obstet,2020,42(12):829-833.
[16] RIGHINI M,ROBERTEBADI H,CREMONESI A,et al.Risk of neonatal hypothyroidism in newborns from mothers exposed to CTPA during pregnancy: ancillary data from a prospective outcome study[J].J Thromb Haemost,2022,20(11):2550-2555.
[17] DONG A C,MORGAN J,KANE M,et al.Subclinical hypothyroidism and thyroid autoimmunity in recurrent pregnancy loss: a systematic review and meta-analysis[J].Fertil Steril,2020,113(3):587-600.
[18] KOYYADA A,ORSU P.Role of hypothyroidism and associated pathways in pregnancy and infertility: clinical insights[J].Tzu Chi Med J,2020,32(4): 312-317.
[19] DING Z,LIU Y,MARAKA S,et al.Pregnancy and neonatal outcomes with Levothyroxine treatment in women with subclinical hypothyroidism based on new diagnostic criteria: a systematic review and meta-analysis[J].Front Endocrinol (Lausanne),2021,12(5):797423-797429.
[20] ZHANG Y,LIU Y,LI Z,et al.Comparison of reproductive outcomes in subclinical hypothyroidism women with high-normal versus low-normal thyroid-stimulating hormone levels after treatment with levothyroxine [J].Clin Endocrinol (Oxf),2023,98(3):426-435.
(收稿日期:2024-01-08) (本文編辑:陈韵)