前路手术与后路单开门手术治疗多节段颈椎退变的效果比较
冉波 曾勇
[摘要] 目的 比较前路融合手术(ACDF/ACCF)与后路单开门手术治疗多节段颈椎退变的效果。 方法 选取2008~2018年成都市第二人民医院收治的200例多节段退变性颈椎手术患者(≥3个椎体),根据治疗方法不同分为前路组和后路组,每组各100例。前路组行ACDF/ACCF手术,后路组行颈椎后路单开门扩大成形手术,对上述两组患者进行比较分析,比较两组患者术后伤口情况、有无肺栓塞、有无DVT形成、神经并发症发生情况、吞咽困难占比、住院时长及手术翻修率情况、住院费用及保守治疗的费用等。 结果 术后前路组的伤口感染占比、伤口裂口占比、伤口血肿占比、DVT占比、神经并发症占比、吞咽困难占比、住院时长占比、住院费用占比等指标均低于后路组,差异均有统计学意义(P<0.05)。术后前路组吞咽困难发生率6%,后路单开门手术组为1%,后路组吞咽困难发生率明显小于前路组。前路手術1个月内并发症发生的概率较低,其中伤口感染率为1%,后路手术伤口感染率为5%,前路组明显低于后路组。前路组的住院费用比较低,约(15 632±78)元,后路组住院费用较高,约(26 324±48)元。前路手术组住院时间较短约(8.7±1.2)d,后路手术组约(13.6±1.3)d。 结论 就治疗多节段颈椎退变来说,前路ACDF/ACCF手术较后路单开门手术的优点更多,有较低的并发症发生率,住院时间更短,住院费用更低。
[关键词] 多节段;颈椎病;前路;单开门;并发症
[中图分类号] R687.3 [文献标识码] B [文章编号] 1673-9701(2022)10-0077-04
[Abstract] Objective To compare the effect of anterior fusion surgery and posterior single open-door surgery in the treatment of multi-level cervical degeneration. Methods A total of 200 patients with multi-level cervical degeneration undergoing surgery in Chengdu Second People′s Hospital from 2008 to 2018 (≥ 3 affected segments) were colleoted and divided into the anterior approach group and the posterior approach group according to treatment methods,with 100 cases in each group.The anterior group underwent anterior cervical discectomy and fusion/anterior cervical corpectomy and fusion (ACDF/ACCF),and the posterior group underwent cervical posterior single open-door expansive laminoplasty. The above two groups were compared and analyzed, and the following indicators were compared between the two groups of patients:Postoperative wound conditions, occurrence of pulmonary embolism,deep venous thrombosis (DVT) formation and neurological complications,the proportion of dysphagia,length of hospital stay, surgical revision rate,the cost of hospitalization and conservative treatment, etc. Results The anterior approaoh group of postoperative wound infection, wound dehiscence, wound hematoma, DVT,neurological complications, dysphagia, length of hospital stay and hospitalization costs and other indicators in the anterior approach group were lower than those in the posterior approach group, with statistically significant differences(P<0.05).The incidence of anterior approaoh group after anterior surgery was 6%, while the postelior appvoaoh group was 1%, and the incidence of anterior approaoh group was significantly lower than the postelior appvoaoh group. The anterior approaoh group of complications occurring within one month after the anterior surgery was low, including wound infection rate of 1%. The wound infection rate for the postelior appvoaoh group was significantly lower than that for posterior surgery (5%).The hospitalization cost of anterior approaoh group was low, about (15 632±78)yuan,and the hospitalization cost of the postelior appvoaoh group is high, about (26324±48)yuan.The length of hospital stay for anterior approaoh group about (8.7±1.2)days was shorter than that for the postelior appvoaoh group about (13.6±1.3)days. Conclusion For the treatment of multi-level cervical degeneration, anterior ACDF/ACCF shows more advantages than posterior single open-door surgery, such as lower incidence of complications, shorter length of hospital stay and lower hospitalization cost.4B27B679-465B-4DBA-B467-5C1DE1F4884A
[Key words] Multi-level; Cervical spondylopathy; Anterior approach; Single open-door; Complication
颈椎病又称颈椎综合征,是颈椎骨关节炎、增生性颈椎炎、颈神经根综合征、颈椎间盘脱出症的总称,是一种以退行性病理改变为基础的疾患[1]。多节段颈椎退变是指3个或3个以上颈椎节段发生的退变[2]。目前颈椎手术治疗按入路方式主要分为前路和后路手术。前路手术包括椎间盘切除融合术(anterior cervical discectomy and fusion,ACDF)和椎体次全切融合术(anterior cervical corpectomy decompression and fusion,ACCF)[3-4]。后路手術主要包括椎板成形术、椎板切除术、单/双开门手术等[5-6]。因为颈椎前后路手术各有其优缺点,所以目前对于多节段颈椎退变性疾病,是行前路手术还是后路手术,目前仍有许多争论。本文总结成都市第二人民医院多节段退变性颈椎疾病手术病例,比较ACDF/ACCF与后路单开门手术在治疗3个椎体及以上的多节段颈椎退变性疾病的疗效差距以及一些并发症的差异,现报道如下。
1 资料与方法
1.1 一般资料
从成都市第二人民医院资料库中提取的多节段退变性颈椎病例进行回顾性研究,所纳入的患者为2008—2018年10年内的200例多节段退变性颈椎病手术患者,其中包括行前路ACDF和(或)ACCF或经后路行手术患者100例,后路单开门手术患者100例,随访时间为15~24个月(平均18个月),随访应答率为98%,失访率为2%。结果包括术后半年内的不良反应和术后半年内的再入院治疗及术后随访期间的翻修率等等。术后并发症包括术后神经系统并发症、伤口感染、伤口裂开、伤口血肿、吞咽困难、肺栓塞、深静脉血栓形成、住院时长、翻修率、住院费用、理疗费用等。并发症可在住院患者及门诊患者中进行总结统计与评估。
1.2 纳入与排除标准
纳入标准[7]:①平均年龄51岁(40~72岁),其中男100例,女100例;②颈椎退变性疾病患者;③≥3个椎体以上的ACDF/ACCF手术或后路单开门手术。
排除标准[8]:①前后路联合手术患者;②颈椎创伤患者;③颈椎肿瘤患者;④颈椎结核患者;⑤强直性脊柱炎所致颈椎畸形患者;⑥其他不明原因导致的颈椎畸形患者。
1.3 方法
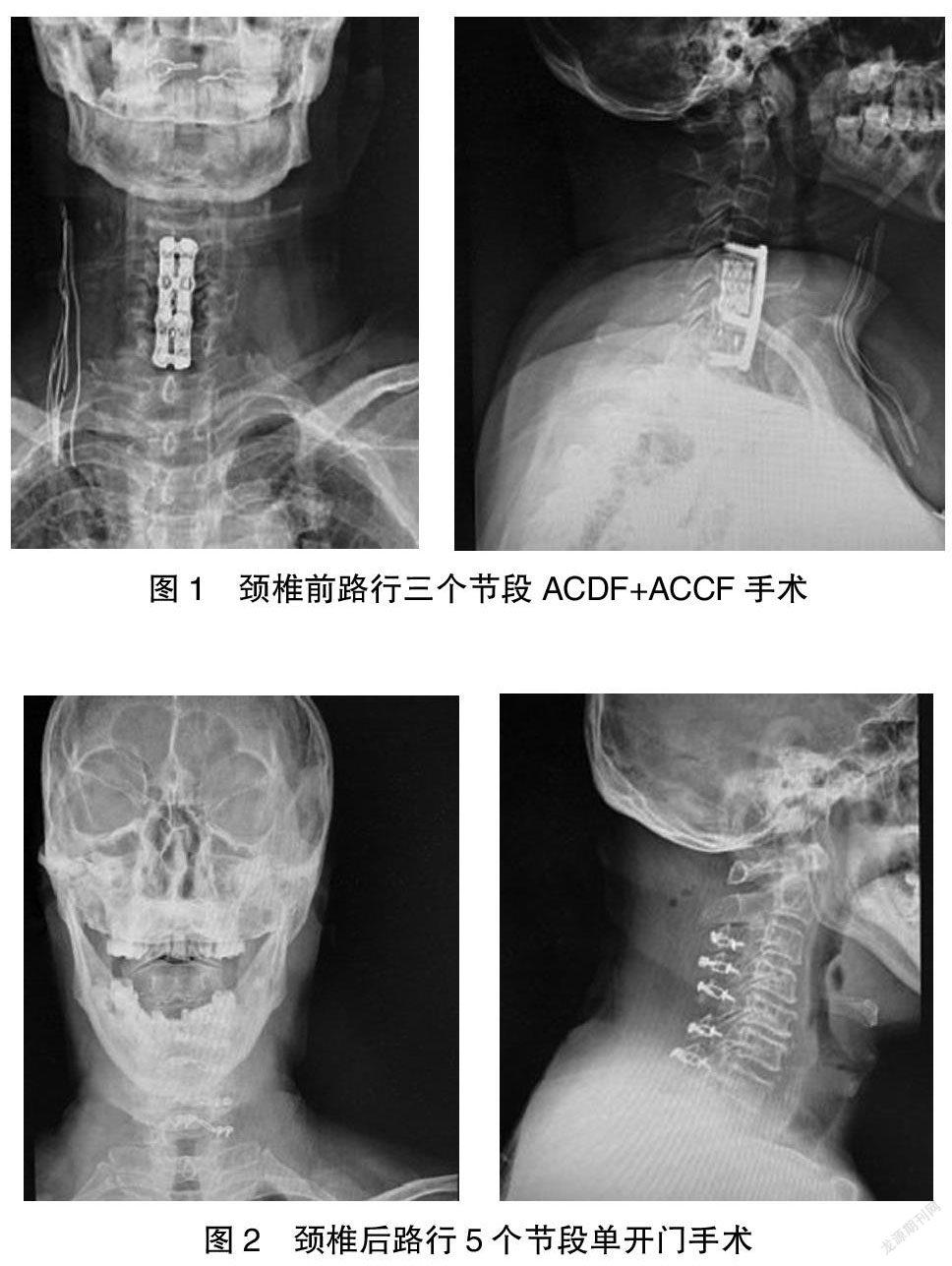
1.3.1 前路手术(ACDF/ACCF) 患者取仰卧位,全麻,颈部过伸位,常规消毒铺巾。做颈前路右侧横形切口,长约5 cm,切开皮肤、皮下组织、颈阔肌,沿颈椎血管鞘与内脏鞘之间进入椎前间隙,C臂定位病变椎间隙。ACDF:撑开钉撑开椎间隙,用刮勺、髓核钳、磨钻充分刮出病变间隙椎间盘及增生的椎体后缘骨赘,切开后纵韧带,切除神经根管增生之骨赘,减压充分。刮出椎间隙上下终板软骨,处理植骨床,置入装满自体骨的椎间融合器。在融合器前方放置合适钛板一枚。ACCF:咬除病变节段椎体,处理植骨床,放置装有自体骨的合适钛笼一枚,在钛笼前面放置合适钛板一枚。大量生理盐水冲洗伤口,逐层缝合伤口,放置一根血浆引流管。
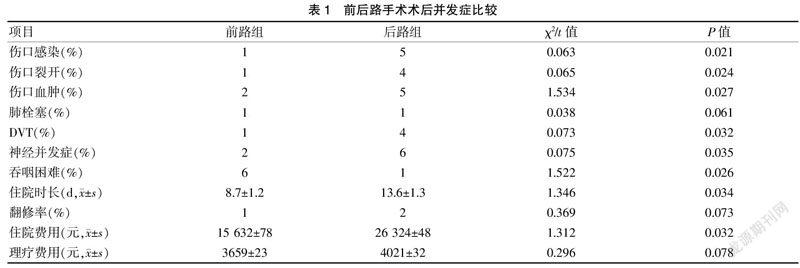
1.3.2 后路单开门手术 全麻后患者取俯卧位,常规消毒铺巾。取颈后路正中纵形切口,长约10 cm。切开皮肤、皮下组织、项韧带。沿双侧棘突及椎板行骨膜下剥离,显露两侧椎板与侧块交界处。使用磨钻于两次棘突根部开槽,于症状较重一侧使用椎板咬骨钳依次咬开椎板内外板全层,向对侧掀开椎板,并切除附着之黄韧带。于开门侧置入微型钛板固定。大量生理盐水冲洗,逐层缝合伤口,放置血浆引流管一根。见图1~2。
1.4 统计学方法
采用SPSS 17.0统计学软件进行分析,计量资料以均数±标准差(x±s)表示,对各组术前与术后比较采用配对t检验,组间比较采用独立样本的t检验,多组间比较采用单因素方差分析,计数资料以[n(%)]表示,组间比较采用χ2检验。P<0.05为差异有统计学意义。
2 结果
经过比较发现颈椎前、后路手术患者在年龄、性别、随访期限、骨形态发生蛋白的使用及伴随疾病等方面差别不大,除了吞咽困难和伤口血肿这两项外,几乎所有并发症发生率都是颈椎前路较低。其中伤口感染、裂开、伤口血肿、深静脉血栓形成以及神经系统并发症这几个方面,颈椎前路组发生率比后路组发生率低很多。见表1。
前路组在住院天数方面也明显少于后路手术组,前路约组(8.7±1.2)d,后路组约(13.6±1.3)d。前路组手术翻修率也低于后路组(1% vs. 2%)。前路组手术翻修手术时间比较差异无统计学意义(P>0.05)。前路组平均医疗费用明显低于后路组,前路组费用(15 632±78)元,后路组费用(26 324±48)元。
3 讨论
目前治疗颈椎退变性疾病的手术方式主要就是前路ACDF/ACCF及后路单开门手术。已有研究[9-10]表明,前路ACDF/ACCF手术有其优缺点。优点是直接切除椎间盘、椎体等前路的脊髓压迫因素,还可恢复颈椎体间的高度及颈椎的生理曲度,重建颈椎的稳定性。缺点是手术操作难度大,有椎体间融合失败的风险,有损伤颈部食管及动脉的风险。后路单开门手术的优点是手术操作难度较小,对脊髓损伤的风险较小,可解除脊髓后方的压迫。其缺点在于不能恢复颈椎的生理曲度,对颈椎后方结构的稳定影响较大,不能直接解除颈椎前方的压迫。所以对退变性颈椎疾病而言,考虑前路手术还是后路手术,一直是学术界争论的问题。
手术并发症方面,既往文献[11-12]显示,前路手术常见的并发症包括颈部血肿、喉头水肿、吞咽困难、内固定松动移位、脑脊液漏等等,后路手术常见的并发症包括轴性疼痛和C5神经根麻痹。因此,单纯从颈椎前后路手术的并发症种类来讲,似乎颈椎前路手术并发症更多,但这些并发症出现的概率如何尚无定论,目前此类研究很少。4B27B679-465B-4DBA-B467-5C1DE1F4884A
目前多節段退变性颈椎病行前路ACDF/ACCF或后路单开门手术后并发症比较的文献很少,Abiola等[13]研究认为多节段脊髓型颈椎病患者行颈椎前路手术并发症与后路手术无明显差异,只是前路手术创伤小,出血少,颈部软组织受影响较小,对术后颈椎活动度影响大于后路手术。但是本文研究结果却与Abiola不同,本文研究结果可提供一个详尽客观的证据以证明前路手术在很多方面均优于后路手术。
本研究发现,除了吞咽困难,其他并发症术后发生率均是前路低于后路,尤其是手术切口的相关问题、神经并发症的出现概率等,前路手术出现概率很低。由此可见,颈椎前路手术在很多方面均优于颈椎后路手术。Wikstrom等[14]曾报道前路手术组伤口感染、伤口裂开、深静脉血栓形成发生率明显低于后路手术组,这与本研究结果类似。但最近也有其他研究分析[15-16]显示,前路手术术后并发症更多,术后翻修率及手术创伤发生率更高。对于这两个报道大相径庭的原因,笔者认为是研究对象的样本偏差所致。本研究中所纳入的研究对象来自于本院近十年的患者,随机筛选,其代表性更强,研究结果也更客观真实。
有文献表明[17-19],前路和后路手术在治疗单节段颈椎病方面花费并无明显差异,但在治疗多节段颈椎病方面花费差异明显。本文也对比了两种手术入路的医疗花费。发现后路手术在医疗费用方面确实比前路要多很多,颈椎后路手术费用几乎接近前路手术的两倍,究其原因,本研究认为跟住院天数更长有关,颈椎后路手术住院天数约为15 d,颈椎前路手术住院时间约为9 d,由此可见,颈椎后路手术住院时间也接近前路手术的两倍。
钟远鸣等[20]研究认为颈椎前路及后路手术患者在术前和术后的物理治疗期间采用的治疗措施基本一致,所花费用也相差不多,这与本研究结果一致。本研究发现颈椎前路手术的理疗费用约为3700元,颈椎后路手术的理疗费用约为4000元,两者的费用比较,差异无统计学意义(P<0.05)。
综上所述,尽管本研究有其局限性,但研究结果提供了一个重要的新依据,以便于选择多节段退变性颈椎病是行前路还是后路手术治疗。本文特地强调前路手术的临床及经济学优点,认为前路手术在治疗多节段颈椎退变方面更有利。
[参考文献]
[1] 刘涛,邱水强,黄宇峰,等.颈前路椎间融合术后矢状位参数变化与临床疗效的相关性研究[J].中华骨科杂志,2018,38(2):79-85.
[2] 张磊,章君鑫,刘昊,等.颈前路ROI-C与后路单开门治疗多节段脊型颈椎病的对比[J].中国矫形外科杂志,2018, 26(23):2123-2129.
[3] 缪健荣,周志平,田守进,等.传统钛板加Cage与ROI-C治疗颈病术后矢状位参数的变化[J].南京医科大学学报(自然科学版),2018,38(11):1572-1575.
[4] Fan XW,Wang ZW,Gao XD,et al.The change of cervical sagittal parameters plays an important role in clinical outcomes of cervical spondylotic myelopathy after multi-level anterior cervical discectomy and fusion[J].J Orthop Surg Res,2019,14(1):429.
[5] Kimura A,Shiraishi Y,Inoue H,et al.Predictors of persi- stent axial neck pain after cervical laminoplasty[J].Spine,2018,43(1):10-15.
[6] Kato M,Namikawa T,Matsumura A,et al.Effect of cerv ical sagittal balance on laminoplasty in patients with cervical myelopathy[J].Global Spine J,2017,7(2):154-161.
[7] Xiao R,Miller JA,Lubelski D,et al. Quality of life out- comes following cervical decompression for coexisting Parkinson's disease and cervical spondylotic myelopathy[J]. Spine J,2016,16(11):1358-1366.
[8] 任志伟,杜恒,杨益民,等.颈椎前后路手术治疗多节段脊髓型颈椎病疗效对比观察[J].山东医药,2018,58(23):85-88.
[9] Wang T,Wang H,Liu S,et al. Anterior cervical discec tomy and fusion versus anterior cervical corpectomy and fusion in multilevel cervical spondylotic myelopathy:A metaanal-ysis[J].Medicine(Baltimore),2016,95(49):e5437.
[10] Alonso F,Voin V,Iwanaga J,et al.Potential mechanism for some postoperative C5 palsies:An anatomical study[J].Spine,2018,43(3):161-166.4B27B679-465B-4DBA-B467-5C1DE1F4884A
[11] Morishita S,Yoshii T,Okawa A,et al.Perioperative com-plications of anterior decompression with fusion versuslaminoplasty for the treatment of cervical ossification ofthe posterior longitudinal ligament:Propensity score matching analysis using a nationwide inpatient database[J].Spine,2019,19(4):610-616.
[12] Xinyuan L,Zhenxiong J,Lei S,et al.Prevalence of ossifi-cation of posterior longitudinal ligament in patients withdegenerative cervical myelopathy:Cervical spine 3D CT observations in 7210 cases[J].Spine,2020,45(19):1320-1328.
[13] Abiola R,Rubery P,Mesfin A.Ossification of the posterior longitudinal ligament:Etiology,diagnosis,and outcomes of nonoperative and operative management[J].Global Spine,2016,6(2):195-204.
[14] Wikstrom L,Nilsson M,Brostrom A,et al.Patients' self -reported nausea:Validation of the Numerical Rating Scale and of a daily summary of repeated numerical rating scale scores[J].Clin Nurs,2019,28(5-6):959-968.
[15] Cheng J,Liu P,Sun D,et al. Correlation of cervical and thoracic inlet sagittal parameters by MRI and radiography in patients with cervical spondylosis[J].Medicine( Baltimore),2019,98(7):e14 393.
[16] Yoshida G,Alzakri A,Pointillat V,et al.Global spinal alignment in patients with cervical spondylotic myelopathy[J].Spine(Phila Pa 1976),2018,43(3):E154-E162.
[17] Lee CK,Shin DA,Yi S,et al. Correlation between cervical spine sagittal alignment and clinical outcome after cervical laminoplasty for ossification of the posterior longitudinal ligament[J].J Neurosurg Spine,2016,24(1):100-107.
[18] Yuan W,Zhu Y,Zhu H,et al. Preoperative cervical sagittal alignment parameters and their impacts on myelopathy in patients with cervical spondylotic myelopathy:A retrospective study[J].Medicine(Baltimore),2017,56(5):e4027.
[19] 周英杰,柴旭斌.對多节段脊髓型颈椎病诊断治疗的一些看法[J].中国骨伤,2016,29(6):561-565.
[20] 钟远鸣,莫日养,梁梓扬,等.脊髓型颈椎病的手术治疗研究进展[J].中国全科医学,2018,21(8):998-1002.
(收稿日期:2021-11-01)4B27B679-465B-4DBA-B467-5C1DE1F4884A

