Tolosa-Hunt Syndrome with underlying latent tuberculosis: a diagnostic dilemma
Abdullah Ashraf Rafique Ali, Tajunisah Iqbal, Justin Yeak, Norlina Ramli
1University Malaya Eye Research Centre, Department of Ophthalmology, University of Malaya, Kuala Lumpur 50603,Malaysia
2Department of Ophthalmology, Faculty of Medicine,University of Malaya, Kuala Lumpur 50603, Malaysia
3Ophthalmology Department, Faculty of Medicine, Universiti Teknologi MARA, Sungai Buloh, Selangor 47000, Malaysia
Dear Editor,
I am Dr. Abdullah Ashraf from Department of Ophthalmology, University of Malaya, Malaysia. I write to present a case of Tolosa-Hunt Syndrome (THS)with underlying latent tuberculosis which became an interesting diagnostic and management challenge. THS is a rare disease with an estimated incidence of 1-2 cases per million population[1]. It is characterized by unilateral painful ophthalmoplegia caused by granulomatous inflammation of the cavernous sinus. However, it is a diagnosis of exclusion and other causes of painful ophthalmoplegia need to be ruled out before the diagnosis of THS can be made[2]. For this case report, written informed consent was obtained from the patient, and the study was conducted in accordance with the Declaration of Helsinki.
CASE REPORT
A 37-year-old gentleman with no known medical illness presented to the Emergency Department complaining of inability to open his left eye for one week. It was preceded by a two-week history of left sided periorbital pain extending to the left temporal region. He came from an area which tuberculosis(TB) was endemic; however, he was asymptomatic of TB.He was initially investigated at another hospital for the same complaint and had computed-tomography (CT) brain done,where he was told to have ‘eye stroke’ and was discharged without medications. However, the headache worsened over the next one week, associated with nausea and vomiting.
On presentation, the left eye looked mildly proptosed with complete ptosis and ophthalmoplegia (Figure 1). It was also noted to be deviated slightly downward and outward.Snellen best corrected visual acuity for both eyes was 6/6.The right pupil was 3 mm in size and the left pupil was dilated at 6 mm and non-reactive to light, however reverse relative afferent pupillary defect was absent. Light brightness,red saturation and color vision were normal for both eyes.Hertel’s exophthalmometry showed a reading of 17 mm for the right eye and 20 mm for the left eye at 115 mm distance between lateral orbital walls. The conjunctiva was white with no corkscrew vessels. Posterior segment examination of both eyes was normal with no evidence of optic disc swelling.Right eye examination was normal. Intra-ocular pressure (IOP)was 18 mm Hg for both eyes. Other cranial nerves were intact,and there were no other neurological deficits. At this juncture,the possibility of an orbital apex or cavernous sinus mass was considered.
An urgent contrasted CT scan of the brain was obtained, and it was initially reported as normal. Following that, an urgent CT angiography (CTA)/CT venography (CTV) was requested, and it reported the presence of a bulky left cavernous sinus with ill-defined enhancing lesion obliterating the left orbital apex.Subsequently, a magnetic resonance imaging (MRI)/magnetic resonance angiography/magnetic resonance venography was done that showed an ill-defined, heterogeneously enhancing bulkiness in the left cavernous sinus, which was seen continuous with the left superior orbital fissure as well as the left orbital apex. This mass had a maximal thickness measuring 0.9 cm at the left cavernous sinus (Figure 2). The differential diagnoses at this point include tumor such as meningioma, granulomatous disease such as tuberculosis or sarcoidosis and THS.

Figure 1 Complete ptosis of the left eyelid with complete ophthalmoplegia of the left eye.
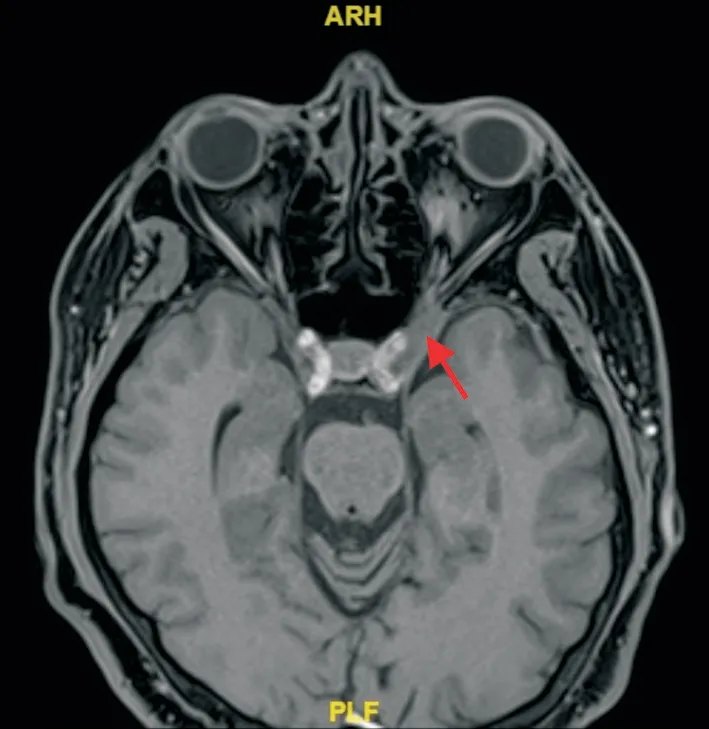
Figure 2 T1-weighted, fat suppressed MRI brain showing an ill-defined, heterogeneously enhancing bulkiness in the left cavernous sinus, which was seen continuous with the left superior orbital fissure as well as the left orbital apex (red arrow).
Peripheral blood picture showed normal hemoglobin, white blood cells (WBC) and platelet levels. The red blood cells and WBC appeared normal microscopically. Erythrocyte sedimentation rate was raised (27 mm/h). Thyroid function test was normal. Screening for hepatitis B, hepatitis C, human immunodeficiency virus (HIV) and syphilis was negative.Serum angiotensin converting enzyme (ACE) level was normal and serum anti-nuclear antibody returned as negative.The chest X-ray was clear with no hilar lymphadenopathy.However, the TB skin induration (Mantoux test) was positive with a reading of 20 mm.
In view of the positive Mantoux test, the patient was referred to the Infectious Disease team who requested for a biopsy sample of the mass to confirm the presence of TB granuloma.After consultation and group discussion with the Neurosurgical and Radiological teams, it was decided that biopsy was too risky and difficult. Instead, the patient was admitted for lumbar puncture to rule out other infectious etiologies, in particular central nervous system TB. Lumbar puncture produced a clear cerebrospinal fluid (CSF) that was negative for inflammatory or atypical cells. Glucose level was normal, but the protein count was mildly elevated (0.56 g/L). The CSF TB polymerase chain reaction (PCR) and acid-fast bacilli (AFB) test were negative, which ruled out active TB infection. CSF virology and culture were also negative.

Figure 3 Examination of 1wk post steroid therapy, showing resolution of left eye ptosis, with improvements of extraocular muscle movements of the left eye (medial -3, lateral 0, superior -2 and inferior -1).
Based on the investigation results, a presumed diagnosis of THS was made, and the patient was treated with intravenous methylprednisolone 1 g once daily for the next 5d. Oral isoniazid 300 mg with oral pyridoxine 20 mg once daily was also initiated for the next 6mo to cover for latent TB due to the positive Mantoux test and slightly elevated protein in the CSF.Day 1 after intravenous methylprednisolone administration, the patient reported reduction of his headaches which completely resolved after completing the steroid therapy. The ptosis and extraocular muscle movement also gradually improved(Figure 3). Patient is currently under follow up to track his recovery process.
DISCUSSION
THS is characterized by orbital/periorbital/hemicranial pain with either partial or complete ophthalmoplegia and ptosis. It is caused by an idiopathic granulomatous inflammation of the cavernous sinus and/or superior orbital fissure which may lead to the compression of any of the structures contained within[3].The 3rdInternational Classification of Headache Disease(ICHD-3 beta) diagnostic criteria for THS is as follows: A.Unilateral pain meeting criterion C; B. Both of the following:1) Granulomatous inflammation of the cavernous sinus,superior orbital fissure or orbit demonstrated by MRI or biopsy;2) Paresis of one or more of the III, IV and/or IV ipsilateral cranial nerves; C. Evidence of causality demonstrated by both of the following: 1) Headache preceding paresis of the III, IV and/or VI nerves for <2wk or developed with it; 2) Headache located around the eye and ipsilateral eyebrow; D. Not better explained by another diagnosis of ICHD-3 beta[4].
As THS is an idiopathic granulomatous inflammation,systemic granulomatous diseases such as sarcoidosis and tuberculosis should be ruled out before considering it. This is especially important in tuberculous meningitis, as the untreated meningitis might be exacerbated by steroid treatment[5]. In our case, the possibility of sarcoidosis was decreased by the normal serum ACE level. Chest X-ray was unremarkable but the positive Mantoux test suggested TB as the cause of the granuloma. However, in view of the patient being asymptomatic of TB, and with the CSF showing negative results for TB PCR and AFB, the treatment was directed more towards THS with intravenous steroids. In this case, isoniazid was also administered to cover for possible latent TB.
Although very rare, tuberculoma in the cavernous sinus presenting as cavernous sinus syndrome has previously been reported in the literature[6]. In many of the cases, the diagnosis was obtained through surgical removal of the tuberculoma and the resultant histopathological report. In two of the cases,the diagnosis was confirmed by extra central nervous system lymph node biopsy. Biopsy of the cavernous sinus lesion itself is technically difficult and rarely indicated, except for patients with rapidly progressive neurologic impairment, high risk for malignant diseases, lack of steroid responsiveness, or unusual or persistent changes on MRI[2]. We did consult the neurosurgeons about the possibility of biopsy in our patient and it was deemed as too risky and difficult. Hence other investigations such as TB PCR on the CSF sampling was done which turned to be negative.
Systemic corticosteroids are the main treatment choice for THS. Improvement in headache and ophthalmoplegia after adequate administration of steroid therapy was one of the diagnostic criteria for THS[7]. The pain usually resolve within 3d of onset of steroid treatment, but the cranial nerve palsies required a longer duration for resolution[8]. Our patient fits this criterion as there was an almost immediate resolution of his headache and gradual improvement of ophthalmoplegia after commencement of intravenous steroid therapy. Currently there is no standardized dosage and duration for the steroid treatment, with various authors reported to have given between 3 to 5d of intravenous steroid therapy. Successful treatment with oral steroid therapy alone has also been reported[1]. However,it is important to caution that a number of inflammatory,neoplastic and lymphoproliferative diseases may be masked by steroid treatment[9].
This case also highlights the need for having a high index of suspicion while treating patients with painful ophthalmoplegia,even when imaging reported normal findings. The first two CT brain scans of our patient did not show any cavernous sinus abnormalities. Other authors also reported to have had normal CT findings before MRI revealed the pathology in the cavernous sinus[10-11]. Gadolinum-enhanced MRI is the modality of choice for visualising lesions in the cavernous sinus and superior orbital fissure. Thus it must be performed for proper evaluation of the region even if the CT showed normal results[12].
In conclusion, THS is a rare disease and a diagnosis of exclusion. Proper examination and investigation, especially to rule out other granulomatous diseases, need to be performed to arrive at a proper diagnosis. Prompt steroid treatment should be administered once the diagnosis of THS is established, as steroid treatment has both diagnostic and therapeutic value in this disease.
ACKNOWLEDGEMENTS
Conflicts of Interest:Rafique Ali AA,None;Iqbal T,None;Yeak J,None;Ramli N,None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
