A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
Wen-Yi Tang, Ting Zhang, Ke-Yan Wang, Qing Chang, Xin Huang, Ge-Zhi Xu
1Department of Ophthalmology, Eye and ENT Hospital of Fudan University, Shanghai 200031, China
2Shanghai Key Laboratory of Visual Impairment and Restoration, Fudan University, Shanghai 200031, China
3NHC Key Laboratory of Myopia, Fudan University, Key Laboratory of Myopia, Chinese Academy of Medical Sciences,Shanghai 200031, China
Abstract
● KEYWORDS: vitreoretinal surgery; epiretinal membranes peeling; residual posterior vitreous cortex; surgical needle;surgical technique
INTRODUCTION
Complete removal of the posterior hyaloid is an important vitrectomy procedure for treating vitreoretinal disorders,such as retinal detachment, highly myopic macular holes,diabetic macular edema, epiretinal membranes (ERMs), and ocular trauma[1-4]. Although posterior vitreous detachment(PVD) can be induced spontaneously or surgically, some residual cortex, visualized with triamcinolone acetonide (TA)staining[5-6], may attach tightly to the retinal surface and may be associated with recurrent retinal detachment, failed macular hole closure, or future ERMs.
Several surgical techniques to remove the residual posterior vitreous cortex using various instruments, including a vitrectomy probe, surgical forceps, and a Tano diamonddusted membrane scraper, have been described[4,7]. However,some of the residual vitreous cortex may remain in situ,especially in eyes with a mobile, detached, thin, or atrophic retina. Furthermore, Tano diamond-dusted membrane scrapers may not be available in developing countries, and the use of this scraper might result in subclinical retinal pigment epithelial damage or parafoveal scotoma[8]. As an alternative,we use syringe needles, which are widely available in the ophthalmologic operating room, by bending the tip into a hook prior to use. In this study, we describe our simple technique, in which we bend a 2 mL syringe needle (outer diameter, 0.6 mm; 23 gauge) into a hook and use it to remove the residual posterior vitreous or to facilitate inner limiting membrane (ILM) peeling during vitreoretinal surgeries. We report the efficacy and safety of using this instrument in a variety of vitreoretinal disorders.
SUBJECTS AND METHODS
Ethical ApprovalThis study was performed in accordance with the tenets of the Declaration of Helsinki, and was approved by the Institutional Review Board of the Eye and ENT Hospital of Fudan University (Shanghai, China). Written informed consent was provided by all patients before the procedures. The patients included underwent standard threeport pars plana vitrectomy (PPV) with a 23-gauge trocarcannula system (Constellation, Alcon, Fort Worth, TX, USA).All surgeries were performed by two surgeons (Huang X and Chang Q).
Surgical TechniqueA hook was made on the tip of a commonly used disposable needle (32 mm; outer diameter, 0.6 mm;23 gauge; Kindly Enterprise Development Group Co., Ltd.,Shanghai, China) by hitting it vertically and gently against a plate (Figure 1). The angle of the hook is 90° or 270° and the length is usually 20-30 μm. And it is carefully examined under a microscope prior to use. After core vitrectomy, 4 mg/0.1 mL of TA suspension (40 mg/mL; Kunming Jida Pharmaceutical Co. Ltd., Kunming, China) was injected into the vitreous cavity to visualize the posterior hyaloid. PVD was performed by aspiration via the vitrectomy probe in most cases. The residual cortex stained with TA was then gently removed using the hook (Figure 2). After staining the ILM with indocyanine green, the edge of the ILM was advanced by the hook and then peeled using ILM forceps (Figure 3). The procedures of making the hook are demonstrated in Video 1 (online supplementary). Intraoperative optical coherence tomography images were captured during the surgical procedures using the Rescan 700 (Carl Zeiss Lumera 700 with integrative HD OCT,Carl Zeiss Meditec AG).
RESULTS
We have used the hook in a variety of vitreoretinal disorders and found it especially effective for removing the residual posterior vitreous cortex in patients with pathological myopia and a thin, fragmentary posterior hyaloid or in patients with diabetic macular edema with a taut posterior hyaloid. We have also used the hook to advance the free edge of the ILM while peeling it, and to strip thin, immature ERM in patients with proliferative vitreoretinopathy (PVR). Intraoperative optical coherence tomography demonstrated that the retina was not damaged during the removal of the residual posterior vitreous cortex or the creation of epiretinal and ILM flaps (Figure 4).Thus far, we have used this hook in 1091 patients, with a mean follow-up period of 13.1±6.5mo (Table 1). In the 551 eyes with rhegmatogenous retinal detachment (RRD), 434 cases (78.8%)were primary RRD and 117 cases (21.2%) were recurrent PVR-related RRD. In the 156 eyes with full-thickness macular hole (MH), 107 cases (68.6%) were idiopathic while 49 cases(31.4%) were highly myopic. In the 143 eyes with vitreous hemorrhage (VH), 78 cases (54.5%) were complicated with diabetic tractional retinal detachment (TRD), 38 cases(26.6%) were due to branch retinal vein occlusion, 20 cases(14.0%) were due to diabetic VH, 4 cases (2.8%) were due to retinal tear, and 3 case (2.1%) was due to polypoidal choroidal vasculopathy. In the 90 eyes with pathologic myopic foveoschisis, 70 cases (77.8%) were with fovea detachment.Intraoperatively, we observed focal, limited retinal hemorrhage when advancing the edge of the ILM in areas where more aggressive maneuvers were performed in 55 eyes (5.0%; Table 2). However, no serious cases of intraoperative complications concerning the use of the hook, such as VH, iatrogenic retinal break or RRD, or inadvertent lens touching, were encountered.During the follow-up, 33 eyes (3.0%) suffered from recurrent PVR-related RRD. Twenty-eight eyes (2.6%) experienced recurrent VH. Twelve eyes (1.1%) developed new-onset RRD. Ten eyes (0.9%) developed new-onset MH. No cases of endophthalmitis were noticed.
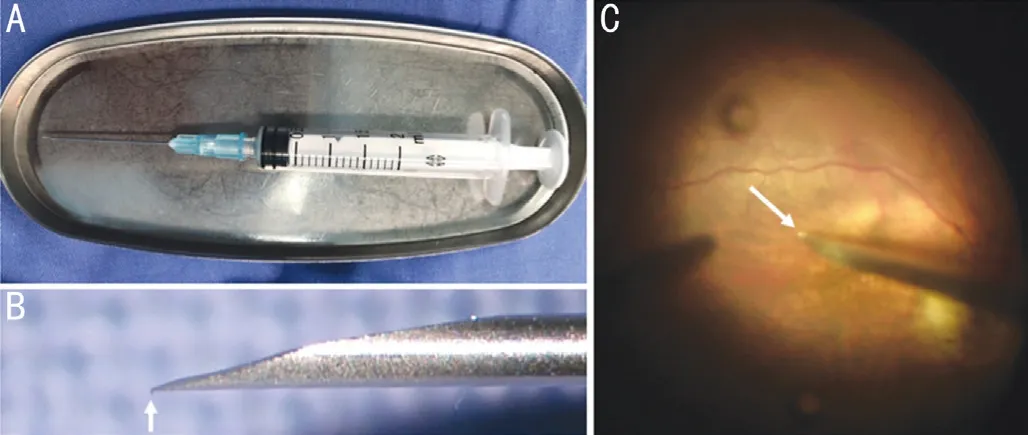
Figure 1 Preparing a hook using a conventional syringe needle A:A conventional, disposable 2 mL syringe needle; B: The hook (white arrow)is created by hitting the needle against the plate; C: Intraoperative image showing the hook (white arrow) inserted into the eye.
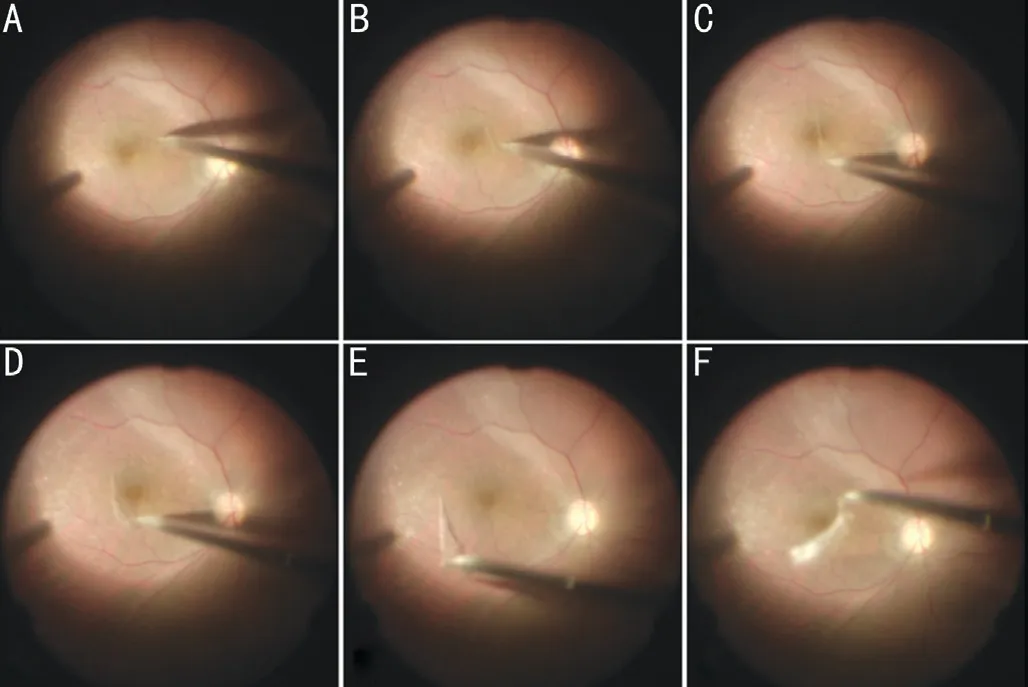
Figure 2 Sequence of intraoperative images showing the surgical strategy for removing the residual vitreous cortex in an eye with rhegmatogenous retinal detachment The residual vitreous cortex,visualized with triamcinolone acetonide, can been seen in the macula as a white dot island, and was successfully removed using the hook.
DISCUSSION

Figure 3 Sequence of intraoperative images demonstrating the surgical strategy in which the hook was used to create a ILM flap in a highly myopic eye with a macular hole and retinal detachment The ILM is stained with indocyanine green. The hook was used to advance the edge of the stained ILM (A, B; white circle in B). The ILM forceps were then used to grasp the flap (white circle in C) and to complete the peeling of ILM (D).

Figure 4 The 6 mm×6 mm intraoperative optical coherence tomography images showing the creation of epiretinal membrane flap (arrow in C) without damage to the retina using the blunt hook.
Cortical vitreous remnants commonly adhere to the retina after PVD during TA-assisted PPV. A histopathological analysis revealed residual posterior vitreous cortex in the foveal area after spontaneous PVD in 44% of 59 autopsied eyes[9].Kimura et al[1]found perimacular remnants of the vitreous cortex due to surgically induced PVD during vitrectomy in six of nine patients with RRD. The posterior hyaloid cortex is a major component of the ERM[10]. Residual vitreous cortex can provide a scaffold for cellular proliferation and cause retinal thickening and wrinkling, which may contribute to vitreoretinal interface disorders that affect the visual outcome[11-12]. Therefore, complete removal of the residual vitreous cortex from the retina is a critical step in vitrectomy for optimal therapeutic outcomes and to reduce postoperative complications.
In this study, we used a technique in which we formed a hook from a conventional needle, that facilitated the complete removal of the residual posterior vitreous cortex from the retina. There are several advantages of this technique. First,the hook can be made quickly and cheaply (Video 1, online supplementary). Reusable instruments, including scrapers and retinal brushes, may be worn down with frequent use over a long period of time, whereas needles are disposable. Second,the hook can be used widely for either diffuse or focal residual posterior vitreous cortex as defined in previous studies[5,7]. In particular, it facilitated the separation of the posterior vitreous cortex following retinal detachment in young patients, as well as in patients with pathological myopia or diabetic retinopathy in which a diffuse, thin vitreous cortex is frequently observed,even after surgical PVD[5]. The hook was also useful when advancing the free edge of the ILM. We also confirmed that this blunt hook could be used safely, with no cases of iatrogenic retinal break or detachment, or VH. The focal and limited retinal hemorrhages can be absorbed shortly after the surgeries. And during the follow-up, no additional or more frequent complications related to the use of the hook was noted compared with previous studies[13-14]. The hook can also be prepared using a standard disposable needle (38 mm; outer diameter 0.5 mm; 25 gauge) for 25 gauge trocar-cannula vitrectomy,with similar effectiveness and safety to that observed with 23 gauge procedures. The hook should be prepared with care,without applying too much force or hitting it against a surface too hard, otherwise the hook may be too large to be inserted into a 23-gauge or 25-gauge cannula.

Table 1 Baseline characteristics of the patients in this study

Table 2 Intraoperative and postoperative complication profile in this study
In summary, our simple technique using a conventional syringe needle shaped into a hook is a suitable for removing the residual posterior vitreous cortex removal or to peel the ILM. This hook can be used in a wide variety of vitreoretinal surgical procedures.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.81770944; No.81800846); Shanghai Hospital Development Center (No.SHDC2020CR2041B).
Conflicts of Interest:Tang WY,None;Zhang T,None;Wang KY,None;Chang Q,None;Huang X,None;Xu GZ,None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
- Bilateral choroidal detachment and exudative retinal detachment following laser peripheral iridotomy in a case of ocular Vogt-Koyanagi-Harada’s disease
