Bilateral choroidal detachment and exudative retinal detachment following laser peripheral iridotomy in a case of ocular Vogt-Koyanagi-Harada’s disease
Arijit Mitra, Arnab Das, Sumit Choudhury, Suchanda Sar, Debarpita Chaudhury
Department of Glaucoma, Disha Eye Hospitals Pvt.Ltd.,Barrackpore, Kolkata 700120, West Bengal, India
Dear Editor,
We present a case of bilateral choroidal detachment(CD) and exudative retinal detachment (ERD)following laser peripheral iridotomy (LPI) in a patient of ocular Vogt-Koyanagi-Harada’s disease (VKHD). A 42 yearold-lady presented to us with the complaint of sudden onset of pain, redness, and dimness of vision in her right eye for past two weeks. Her best-corrected visual acuity (BCVA) was 20/40 and 20/30 in right and left eye respectively. There were few large granulomatous, mutton fat type keratic precipitates (KP)in both eyes. Anterior chamber had grade 1+flare in both eyes and occasional cells in left eye and grade 1+cells in right eye.Pupil in left eye was 3 mm in diameter with normal reaction.Right eye pupil was 4.5 mm in diameter, irregular, mid-dilated,not reacting to light with posterior synechiae. Intraocular pressures (IOPs) were 42 and 14 mm Hg in her right and left eyes respectively. Gonioscopy showed occludable angles with peripheral anterior synechiae (PAS) in both eyes.
Approvalwas taken from the Ethics Committee of our hospital and the study was conducted in accordance with the principles of the Declaration of Helsinki. Informed consent was taken from the patient.
Fundus examination showed depigmentation of fundus with an orange-red discoloration with presence of retinal pigment epithelial clumps on the posterior pole in both eyes(Figure 1A-1B). The cup-disc ratio (CDR) was 0.3 in both eyes. There was no history of penetrating ocular trauma or surgery. These features were suggestive of probale, ocular(incomplete) VKHD since there were no associated cutaneous or neurological findings. A diagnosis of acute attack of angle closure in right eye in a patient of probable ocular (incomplete)VKHD in both eyes was made. Yttrium-Aluminium-Garnett(YAG) LPI in both eyes was done. Two LPIs were done in right eye at 2 o’clock (5.2 mJ, 3 shots) and 10 o’clock (5.2 mJ, 4 shots)positions and one LPI was done at 3 o’clock position (5.0 mJ,4 shots) in left eye. Patient was prescribed prednisolone acetate ophthalmic suspension, United States Pharmacopeia (USP)(1%), a fixed-dose combination of brimonidine tartrate 0.2%w/v and timolol maleate 0.5% w/v eye drop in both eyes, oral acetazolamide tablets (250 mg), one tablet twice daily for 5d and tablet prednisolone, 40 mg/d for one week.
At the follow-up visit after five days, the patient complained of further dimness of vision. On examination her BCVA was 20/120 in right eye and 20/80 in left eye. IOPs were 16 and 14 mm Hg in right and left eyes respectively. Anterior chamber reaction had subsided in both eyes. All LPIs were patent. Fundus examination showed CD inferiorly along with exudative-non-rhegmatogenous retinal detachment in both eyes. Submacular fluid was noted on examination of the posterior pole. Optomap retinal examination (OPTOS, widefield retinal imaging) confirmed the clinical findings (Figure 1C-1F). Spectral domain optical coherence tomography(SD-OCT) showed submacular fluid along with choroidal undulation in both eyes. Central foveal thickness (CFT) was 852 μm in right eye and 458 μm in left eye (Figure 1G and 1H). Axial lengths were 22.56 and 22.71 mm in right and left eye respectively. Patient was asked to continue antiglaucoma medication and topical steroids and topical atropine sulphate(1% w/v) eye drops was added in both eyes. The dose of oral steroids (presnisolone tablets) was increased to 60 mg/d for one week and then in tapering dose for one month.

Figure 1 Fundus photographs at presentation. Widefield retinal images and OCT images of both eyes of the patient five days after YAG laser iridotomy Fundus photographs of the right eye (A)and left eye (B) at presentation before YAG laser iridotomy. A, B:Depigmentation of the fundus resulting in an orange-red discoloration and presence of retinal pigment epithelial clumps in both eyes;C-F: The Optomap retinal examination (OPTOS, wide field retinal imaging) figures of both eyes 5d post YAG laser iridotomy; C, D:The right eye in straight gaze and upgaze respectively; E, F: The left eye in straight gaze and upgaze respectively and they show CD along with exudative non-rhegmatogenous retinal detachment in the inferior region of both eyes; G, H: SD-OCTof the right and left eye respectively 5d post YAG laser iridotomy which show submacular fluid along with choroidal undulation in both eyes. CFT is 852 μm in the right eye and 458 μm in the left eye.
After one week, her BCVA had improved to 20/30 in right eye and 20/40 in left eye. IOP was 14 mm Hg in both eyes with patent LPIs (Figure 2A and 2B). OPTOS imaging showed almost complete resolution of the CD and ERD (Figure 2C-2F).SD-OCT images showed marked resolution of submacular fluid and choroidal undulation in both eyes (Figure 2G and 2H).CFT had reduced in both eyes. Topical and oral steroids,atropine eye drops, and anti-glaucoma medication were continued. At last follow up her BCVA was 20/20 in both eyes.The submacular fluid and the CD and ERD had completely resolved. She was advised regular follow-ups at Retina and Glaucoma Departments.
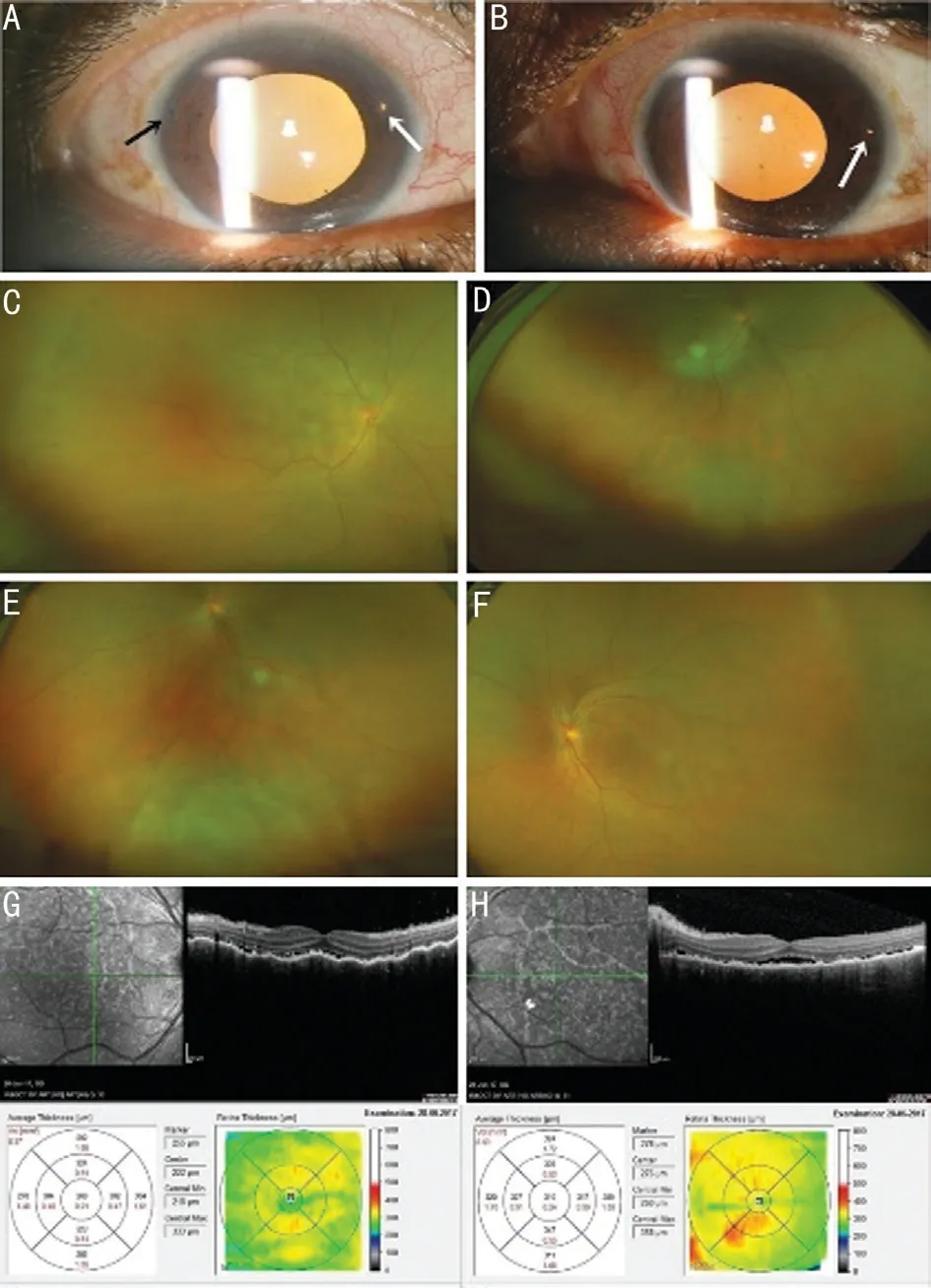
Figure 2 Fundus photographs, widefield retinal images and OCT images of both eyes after conservative management A,B: Slit lamp photographs of the right and left eyes respectively. KP and pigments on the back of the cornea of both eyes. Two patent LPI’s can be seen in the right eye at 10 and 2 o’clock positions and one patent LPI can be seen in the left eye at 3 o’clock position.C-F: The Optomap retinal examinations (OPTOS wide field retinal imaging) figures of both eyes. C, D: The right eye in straight gaze and upgaze respectively; E, F: The left eye in straight gaze and upgaze respectively and they show almost complete resolution of the CD and the exudative non-rhegmatogenous retinal detachment in both eyes. G,H: SD-OCT of the right and left eye respectively which shows marked resolution of the submacular fluid along with choroidal undulation.CFT is 268 μm in the right eye and 310 μm in the left eye.
We know that VKHD is a systemic condition which is associated with a non infectious granulomatous panuveitis. In 2001, the first International Workshop on VKHD proposed diagnostic criteria that rely on specific ocular and systemic criteria[1]. In its complete form, VKHD is defined as a nontraumatic bilateral panuveitis and is associated with integumentary, neurological/auditory signs[2]. Probable (ocular) VKHD is characterized as matching ocular manifestations but in the absence of extraocular manifestations[3].
Incidence of glaucoma noted in cases of VKHD is between 6%-45%[4]. In VKHD, ocular hypertension, open angle glaucoma, angle-closure glaucoma, glaucoma due to combined mechanisms and secondary glaucoma have been described[4]. Potential mechanisms of glaucoma secondary to uveitis include blockage of the trabecular meshwork with inflammatory cells, prostaglandin-induced IOP elevation,swelling of the trabecular meshwork (trabeculitis), peripheral anterior synechia formation, pupillary block with secondary angle closure and corticosteroid induced IOP elevation[4-5].In our case the chronic anterior-chamber inflammation was probably the cause for anterior rotation of the ciliary body and subsequent pupillary block and angle closure. Acute angleclosure has been noted to be the presenting manifestation of VKHD in a few reported cases as was seen in our case[6].
If a patient of VKHD presents with a shallow chamber with normal or moderately raised IOP with no PAS then treatment with topical and oral steroids and mydriatic-cycloplegic eye drops results in resolution of the episode[4]. If however the presentation is with pupillary block, angle closure,raised IOP and presence of PAS, the treatment is on the lines of management of an acute attack of angle closure and intervention in the form of LPI, surgical peripheral iridotomy or trabeculectomy may be required[4,6]. Cases of VKHD with angle closure may have CD with ERD preintervention, that is, before an LPI is done[6]. Our patient had no evidence of ERD or CD at presentation. There is no evidence in literature of the development of bilateral CD and ERD post YAG laser iridotomy in a case of VKHD as was seen in our case.
The age of the patient, axial length, refractive correction,amount of laser energy used, IOP at the time of the procedure,medications used pre-procedure and post-procedure were nothing out of the ordinary and could not shed any light as to the probable cause. The close temporal relationship between the procedure and the appearance of subjective symptoms suggests that probably Nd:YAG LPI had some role in the development of the CD and ERD in this VKHD patient. Uveal effusion or ERD can and does occur fairly commonly in nanophthalmic eyes spontaneously or following laser treatment or surgical intervention[7]. Salehi et al[8]reported a case of choroidal effusion after argon laser peripheral iridoplasty but such an occurrence after an iridotomy is extremely rare. Kaden et al[9]had reported a case of choroidal effusion after LPI in a case of uveitis. However their patient was a 60-year-old hypermetropic lady who was a known case of juvenile rheumatoid arthritis with history of recurrent uveitis and she had undergone treatment for a retinal tear. So there were a number of associated factors which might have been individually or collectively responsible for the development of choroidal effusion in that particular case. Clinically evident or subclinical uveal effusion, detected by ultrasound, may be seen in untreated eyes with primary angle-closure glaucoma(PACG) or acute attack before or after LPI[10]. In the study done by Kumar et al[10]in PACG patients using ultrasound biomicroscopy (UBM) the authors noted the prevalence of uveal effusion in 14.2% of newly diagnosed PACG patients before an LPI was performed and in 7.1% of patients after an LPI had been done.
This case brings to light a lot of important issues. It shows that CD and ERD may occur in a case of VKHD presenting with pupillary block after an LPI has been performed. Thus even though at presentation there may be no evidence of an ERD or CD, the possibility of such an event occurring after the laser procedure should be kept in mind. The possibility of subclinical effusion being present in untreated eyes with primary angle-closure disease, nanophthalmos and probably in eyes with VKHD should also be kept in mind. Thus the possibility of an uveal effusion developing in these eyes post laser iridotomy may not be as uncommon as it is thought to be.Even though most of these effusions are subclinical there is the chance that a clinically significant effusion may develop in a small percentage of these patients.
ACKNOWLEDGEMENTS
Conflicts of Interest: Mitra A,None;Das A,None;Choudhury S,None;Sar S,None;Chaudhury D,None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
