Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
Yu Di, Hai-Yan Xu, Jun-Jie Ye, Meng-Da Li
1Department of Ophthalmology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences,Beijing 100730, China
2Department of Ophthalmology, Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Tsinghua University,Beijing 102218, China
Abstract
● KEYWORDS: intraocular lymphoma; diagnostic vitrectomy;pathological examination; immunohistochemistry; gene rearrangement; flow cytometric immunophenotype
INTRODUCTION
Intraocular lymphoma is a rare lymphocytic malignancy that is mainly derived from B cells, and intraocular lymphoma has been estimated to represent 1.86% of ocular malignant tumors[1]. Intraocular lymphoma contains two main distinct forms: primary intraocular lymphoma (PIOL) is considered to be one of most common forms of intraocular lymphoma and a subtype of primary central nervous system lymphoma(PCNSL). Alternatively, intraocular lymphoma can originate from systemic lymphomas by metastasizing to the eye,which is known as secondary intraocular lymphoma (SIOL).Intraocular lymphoma is a typical representative of masquerade syndrome. It is easy to misdiagnose intraocular lymphoma as chronic uveitis, retinal vasculitis and scleritis, and the general survival after diagnosis is only 3-5y[2]. Therefore, early diagnosis and treatment are extremely important. At present,many cases of intraocular lymphoma are reported worldwide,but there are few systematic case summaries[3-5]. The present study analyzed the clinical data of a group of patients with intraocular lymphoma and summarized their clinical features,diagnoses, treatments, and prognoses, in order to improve the comprehensive understanding of ophthalmologists on intraocular lymphoma.
SUBJECTS AND METHODS
Ethical ApprovalThe study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board/Ethics Committee of Peking Union Medical College Hospital. This study was exempt from obtaining informed consent as it was a retrospective study and data analyses were performed anonymously.
PatientsThis study was retrospective in nature. Sixteen consecutive patients (28 eyes) with intraocular lymphoma were recruited at Peking Union Medical College (PUMC) Hospital,Department of Ophthalmology, between January 2004 and July 2019. Among them, 14 patients (24/28 eyes, 85.71%) had been misdiagnosed as uveitis, acute retinal necrosis, and retinal vasculitis.
Clinical ExaminationsAll patients underwent complete ophthalmic examinations, including measurement of best corrected visual acuity (BCVA) with a Snellen chart, intraocular pressure (IOP) evaluations by noncontact tonometry, anterior segment slit-lamp examination, fundus examination, ocular ultrasound, color fundus photography, fluorescein angiography,and optical coherence tomography (OCT). In addition,ultrasound biomicroscopy (UBM) was performed in patients with suspected ciliary body lymphoma, and brain magnetic resonance imaging (MRI) was performed to check whether the central nervous system (CNS) was involved.
Thirteen eyes (10 patients, bilateral, selected one eye; 3 patients unilateral) underwent diagnostic vitrectomy, and vitreous specimens were sent to the Peking Union Medical College Hospital Laboratory Department for cytopathology examination, immunohistochemistry, gene rearrangement and flow cytometric immunophenotypic analysis. Ten eyes(10 patients) were diagnosed as intraocular lymphoma by the results of cytopathology examinations in the fellow eyes. Five eyes (3 patients) were diagnosed as intraocular lymphoma according to analysis of the histopathological results of systemic lymphoma by one clinician [two patients had central nervous system lymphoma (CNSL), and one patient had paranasal sinus lymphoma].
TreatmentTwenty-three eyes were treated with intravitreal administration of methotrexate (MTX). Two patients (4 eyes)could not receive ocular treatment due to life-threatening lymphoma of the CNS. There was no need for ocular treatment for one patient (1 eye) because the fundus lesions regressed after systematic chemotherapy. In addition, nine patients received chemotherapy, and two patients received chemotherapy combined with brain radiotherapy.
Statistical AnalysisStatistical analyses were conducted using SPSS statistical software version 23.0 (IBM, Armonk,NY, USA). BCVA values were converted to logarithm of the minimum angle of resolution (logMAR) equivalents. All data are presented as the mean±standard deviation (SD). A paired t-test was used to compare visual acuity between the presenting state and the final follow-up state. The differences in data are reported with 95% confidence intervals (CIs). A two-tailed P value ≤0.05 was considered statistically significant for all analyses.
RESULTS
Patient CharacteristicsSixteen patients (28 eyes) with intraocular lymphoma were included in the study. Of these patients, 7 were male (12 eyes), and 9 were female (16 eyes). Their mean age was 55.38±10.10y (range, 30-67y). Intraocular lymphoma was unilateral in four patients (25%) and bilateral in twelve (75%) patients. The mean diagnostic time and mean follow-up time were 10.06±19.84mo (range, 1-84mo)and 15.19±17.29mo (range, 0.5-60mo), respectively. Eleven patients presented with PIOL, of which eight patients subsequently developed CNSL. Three patients developed intraocular lymphoma subsequent to the diagnosis of systemic lymphoma. The organs affected included the paranasal sinuses,breasts and lymph nodes. In addition, two patients had PCNSL.Twenty-five eyes had vitreoretinal lymphoma, and three eyes had ciliary lymphoma.
Ocular Clinical FindingsAmong twenty-eight eyes, 15 eyes had blurred vision, 2 eyes had floaters, 7 eyes had blurred vision accompanied by floaters, 2 eyes had blurred vision accompanied by redness and pain, and 2 eyes had no symptoms. The initial BCVA were as follows: no light perception (NLP), 2 eyes; light perception (LP), 4 eyes; hand movement (HM), 1 eye; 20/2000 to 20/63, 11 eyes; 20/50 to 20/32, 3 eyes; and 20/25 to 20/20, 7 eyes. The initial mean BCVA was 1.03±0.19 logMAR. The initial IOP values were as follows: 10 to 21 mm Hg (1 mm Hg=0.133 kPa), 22 eyes; and 34 to 49 mm Hg, 6 eyes. In the anterior segment of the eyes,13 eyes were found to have anterior chamber cells and keratic precipitate (KP): 5 eyes had mutton-fat KP (Figure 1A), 1 eye had medium sized KP, 6 eyes had small grayish KP, and 1 eye had dust-like KP. In addition, 2 eyes had pseudohypopyon.Additionally, 4 eyes had iris posterior synechia, 2 eyes had iris posterior synechia and neovascularization, and 2 eyes had iris thickening with nodular areas of infiltration. Manifestations in the posterior segment of the eyes included vitritis in 18 eyes,vitreous hemorrhage in 2 eyes (Figure 1B, 1C), pars plana vitrectomy (PPV) combined with silicone oil tamponade in 2 eyes, and mild vitreous opacity in 6 eyes. Seventeen eyes had yellow-white subretinal lesions, of which 1 eye had retinal hemorrhage (Figure 1C-1E), 1 eye had white sheath of retinal blood vessels, 1 eye had optic disc edema with a white sheath of retinal blood vessels and retinal detachment, and 4 eyes had retinal hemorrhage and detachment. In addition, 1 eye had a“leopard spot” fundus, and 10 eyes had a normal fundus (Table 1).
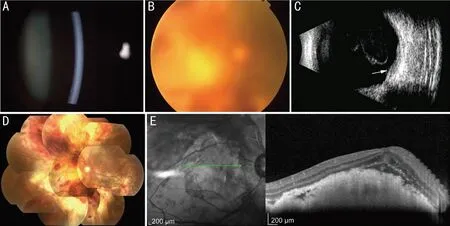
Figure 1 The right eye of a 38-year-old male with PIOL (Patient 11) A: Anterior segment photography showed mild anterior chamber inflammation with small mutton-fat keratic precipitates; B: Fundus photography revealed vitreous hemorrhage and a blurred fundus before surgery; C: B-scan ultrasound revealed vitreous opacity and subretinal lesions (white arrow); D: Fundus photography revealed yellow-white lesions with massive preretinal hemorrhage in the posterior pole after vitrectomy; E: OCT showed multiple hyperreflective signals in the inner retina and subretinal hyperreflective infiltration.
Laboratory ExaminationsVitreous samples of 13 eyes (13 patients) underwent cytopathologic analysis, and atypical lymphoid cells were observed in 11 eyes (11 patients), of which 3 eyes were subjected to immunohistochemistry and gene rearrangement analyses, 1 eye was subjected to immunohistochemistry and flow cytometric immunophenotypic analyses, and 7 eyes were subjected to gene rearrangement and flow cytometric immunophenotypic analyses. The pathological type for all eyes was confirmed as non-Hodgkin diffuse large B cell lymphoma. According to the results of the gene rearrangement and flow cytometric immunophenotypic analyses, the pathological type of 2 eyes with no tumor cells in vitreous samples was non-Hodgkin diffuse large B cell lymphoma. Furthermore, 10 eyes were diagnosed as intraocular lymphoma based on the cytopathological results of fellow eyes. In addition, 4 eyes (2 patients) and 1 eye (1 patient) were diagnosed as having non-Hodgkin diffuse large B cell lymphoma according to the histopathological results of brain and paranasal sinus tissues, respectively (Table 2).
Follow-upThe final BCVA were as follows: 20/25 to 20/20,4 eyes; 20/50 to 20/32, 6 eyes; 20/2000 to 20/63, 9 eyes; count finger (CF), 1 eye; HM, 3 eyes; LP, 4 eyes; and NLP, 1 eye.The final mean BCVA was 1.00±0.19 logMAR (P=0.980).Compared with the initial BCVA (P=0.980), visual acuity improved in 15 eyes (54%), remained unchanged in 5 eyes(18%) and decreased in 8 eyes (29%). The final IOP values were as follows: 9 to 21 mm Hg, 24 eyes; and 30 to 51 mm Hg, 4 eyes. Anterior segment inflammation disappeared in 8 eyes and was reduced in 5 eyes, of which pseudohypopyon disappeared in 2 eyes. Iris nodular infiltration disappeared in 2 eyes. The posterior segment manifestations of the eyes included mild vitreous opacity in 20 eyes, mild vitritis in 1 eye, and PPV combined with silicone oil tamponade in 7 eyes. Fundus lesions disappeared in 9 eyes and were relieved in 6 eyes; 3 eyes showed no changes, and the remaining 10 eyes’ fundus were normal (Table 3).
DISCUSSION
In recent years, with the rapid development of diagnostic technology and the in-depth understanding of intraocular lymphoma, the diagnostic rate has increased significantly.The incidence of intraocular lymphoma in ocular diseases has been reported in Japan to be approximately 21 per 100 000[6], and the incidence in the United States has increased more than threefold in the past 15y[7]. Intraocular lymphoma typically affects seniors aged 50-60 years old, and it has also been reported that the age of onset could be 15-85 years old, with most patients being female. Intraocular lymphomas are bilateral in approximately 60%-90% of patients but are often asymmetrical at presentation, to the extent that the disease may seem unilateral. In this study, the mean age of onset was 55.38±10.10y, and 56.25% (9/16) of patients were female, 75% (12/16) of patients had bilateral disease, and 66.7% (8/12) of patients with PIOL developed CNSL during diagnosis and treatment.
Intraocular lymphoma can be divided into vitreoretinal lymphoma and uveal lymphoma. Intraocular lymphoma secondary to PCNSL and SIOL are usually confined to thevitreoretinal and choroid, respectively. However, predominant involvement of the retina and vitreous without uveal infiltration in patients with systemic lymphoma is extremely rare[8-9]. Salomão et al[10]reviewed the clinical data of 13 patients with intraocular lymphoma, among whom 3 patients had systemic lymphoma involving the vitreous and retina,and the ocular manifestations were similar to those of primary vitreoretinal lymphoma. In this study, patient 15 developed intraocular lymphoma after the diagnosis of breast lymphoma.The ocular manifestations included vitritis in both eyes and a“leopard spot” fundus in the right eye, but the bilateral choroid was not involved. Furthermore, patient 1 was diagnosed with PCNSL, but UBM revealed lesions that grew over the pars plana of the ciliary body. Therefore, it is important for patients with a diagnosis of vitreoretinal lymphoma to undergo systemic evaluation in addition to CNS evaluation. Moreover,examinations of other ocular tissues in addition to the vitreous and retina cannot be ignored in patients with PCNSL.
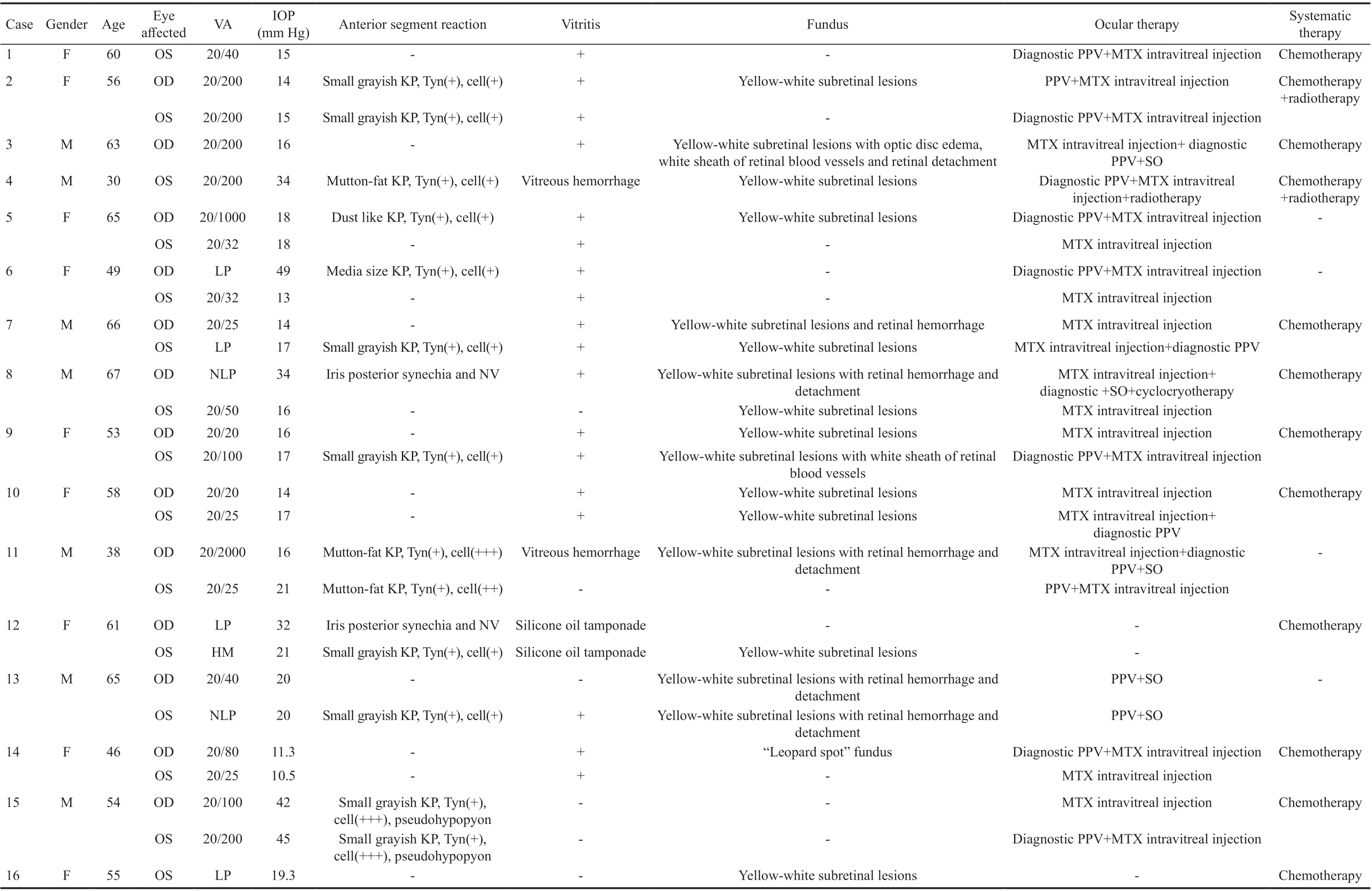
Table 1 The initial ocular findings and therapies

Table 2 Diagnostic methods of intraocular lymphoma
The clinical manifestations of intraocular lymphoma are diverse due to the different involved sites. Blurred vision,floaters or both are the most commonly reported symptoms.However, at early stages of the disease, patients may not complain of any symptoms. In our study, 24 eyes (86%) had blurred vision, floaters, or a combination of both; 2 eyes had redness and pain due to secondary glaucoma, and 2 eyes had no symptoms. It was noted in a previous report that upon slit-lamp examination, anterior segment inflammation was typically absent or minimal[11]. However, Abu Samra et al[12]proposed that anterior reaction and pseudohyphema may be present, especially in patients with SIOL. In this study, 14 eyes (50%) had anterior segment inflammation, and 2 of them presented with a pseudohypopyon in the inferior angle due to SIOL. The typical presence of vitritis on posterior segment examination is large clumps or sheets of cells on vitreous strands. Other common findings include the presence of multiple creamy lesions that are deep in the retina or the retinal pigment epithelium[13]. Twenty-one eyes (75%) had vitritis,and 17 eyes (61%) had yellow-white creamy subretinal lesions in our study. Additionally, some of the atypical findings that have been previously reported include hemorrhagic retinal vasculitis, optic disc edema, and choroidal detachment[8].In our case series, atypical findings included 4 eyes with retinal hemorrhage and retinal detachment, 1 eye with retinal hemorrhage, 1 eye with retinal vasculitis, and 1 eye with retinal vasculitis, optic disc edema and retinal detachment. During the follow-up, 5 eyes (4 patients) had silicone oil tamponade due to the retinal detachment and 2 eyes (1 patient) had silicone oil tamponade before visiting our hospital.
The identification of lymphoma cells is considered the gold standard for the diagnosis of intraocular lymphoma. Velezet al[14]proposed that the presence of tumor cells in anterior uveal structures makes it possible to achieve a diagnosis of intraocular lymphoma through less invasive measures.However, aqueous samples are frequently nonconfirmatory due to the scant cellularity of the sample[12,15]. Diagnostic vitrectomy has several advantages, including improved vision by clearance of vitreous debris and maximizing the sample size. In our study, 13 eyes underwent diagnostic vitrectomy, and the vitreous was positive for malignant cells in 11 eyes (84.6%). Furthermore, immunohistochemistry,gene rearrangement and flow cytometric immunophenotypic analyses can not only clarify the pathological type of intraocular lymphoma but also improve its diagnosis rate.Venkatesh et al[16]proposed that immunocytology increased the rate of diagnosis from 30% (using cytology alone) to 70%.Suigita et al[17]reported that the sensitivity and specificity of molecular examination (IgH gene rearrangement by PCR)for the diagnosis of intraocular lymphoma were 96% and 100%, respectively. In our study, tumor cells were not found by cytopathology examination in patients 8 and 11. However,combined with immunohistochemistry, gene rearrangement and flow cytometric immunophenotypic analyses confirmed non-Hodgkin diffuse large B cell lymphoma. Besides that, we did not perform a retinal or choroidal tissue biopsy because the diagnosis could be made from the above examination results and the patients’ medical history.

Table 3 The follow-up time and final ocular findings
Due to the rarity of intraocular lymphoma, standard and optimal therapy has not been defined, and although intraocular lymphoma cells are highly radiosensitive and chemosensitive,the overall survival rate is still quite low. Intravitreal injection of MTX was found to be effective in inducing clinical remission of intraocular lymphoma, and Frenkel et al[18]proposed that it can be used as a first-line treatment for intraocular lymphoma. In our study, 23 eyes (82.1%) received intravitreal administration of MTX, of which 16 eyes had improved or unchanged visual acuity. The International Primary CNS Collaborative Group (IPCG) recommended guidelines to treat PIOL patients without CNS or systemic involvement: a) If only one eye is involved, local therapy is used. b) f both eyes are involved, there is still a preference toward local therapy,although systematic treatment should not be excluded[19].However, Riemens et al[20]proposed that the use of systematic chemotherapy was not proven to prevent CNSL and was associated with more severe adverse effects than local treatment for patients with isolated primary vitreo retinal lymphoma. In this study, 10 patients developed CNSL, and they were referred to the hematology department and radiotherapy department for chemotherapy or combined radiotherapy. Among them, eight patients had a good prognosis, and two patients had advanced disease because their tumor involved the CNS.
The present study has several limitations. The small sample size and retrospective nature are the major limitations of our study and may have contributed to the low morbidity rate. Another limitation is that chorioretinal biopsies should be performed if vitreous samples fail to provide diagnostic tissue. This type of examination increases the reliability for diagnosing and excluding intraocular lymphoma involving the retina or choroid. However, due to permanent defects in biopsied nerves and irreversible visual impairment, we did not perform this examination.
In conclusion, the clinical manifestations of intraocular lymphoma are diverse, and the misdiagnosis rate is high.Cytopathological analysis of vitreous should be considered to improve the diagnostic rated, which is one of gold standards for the diagnosis of intraocular lymphoma. In addition, immunohistochemistry, gene rearrangement and flow cytometric immunophenotypic analyses can improve the diagnostic rate. Furthermore, ocular chemotherapy or radiotherapy regimens might preserve visual acuity, and a multidisciplinary team (MDT) provides patients with intraocular lymphoma with individualized treatment.
ACKNOWLEDGEMENTS
Authors’ contributions:Di Y and Xu HY carried out the entire procedure including the collection of medical records,statistical analysis, drafting the manuscript and manuscript revision. Ye JJ conceived of the study, coordinated and participated in the entire process of drafting and revised the manuscript. Li MD contributed to manuscript revision. All authors read and approved the final manuscript.
Conflicts of Interest: Di Y,None;Xu HY,None;Ye JJ,None;LiMD,None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
- Bilateral choroidal detachment and exudative retinal detachment following laser peripheral iridotomy in a case of ocular Vogt-Koyanagi-Harada’s disease
