Cost-effectiveness analysis of tele-retinopathy of prematurity screening in lran
Seyed-Farzad Mohammadi, Ameneh Rahban, Sahel Darabeigi, Nastaran Salimi,Afsar Farahani, Alireza Lashay, Cyrus Alinia
1Translational Ophthalmology Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran 6719851351, Iran
2Department of Health Management and Economics, School of Public Health, Urmia University of Medical Sciences, Urmia 571478334, Iran
Abstract
● KEYWORDS: cost-utility analysis; incremental costeffectiveness ratio; quality adjusted life years; teleretinopathy of prematurity
INTRODUCTION
R etinopathy of prematurity (ROP) is the leading cause of blindness in premature infants worldwide[1]and is one of the leading causes of childhood blindness in developing countries, including Iran[2-4]. The incidence rate of ROP in different regions of Iran is reported as 6% to 42.5%, and in some studies, reaches 70%[2-5]. This statistic has been reported for other countries in the range of 6.6%-82%[3]. It is reported that about 57 600 neonates with ROP are born in Iran each year and anticipated this figure would be increased in the next years[6]. ROP disease is preventable if diagnosed in time[2].Otherwise, it is progressive and can lead to poor vision and even blindness. Early diagnosis can increase the effectiveness of treatment interventions and reduce disease costs by as much as 15-20 times[7]. It needs to know that even neonates with mild ROP are more likely to develop close myopia, amblyopia,and other long-term complications than normal babies[8-9].
The World Health Organization (WHO), regarding the importance of the ROP as an “avoidable disease,” included it in the priorities of the VISION 2020 program[10]. Since the prevention of ROP disease provides considerably healthy life years and decreases the financial burden of the disease for the patients, the screening program seems to be cost-effective[2-5].Tele-screening is an emerging technology that captures medical records and then sends them to a specialist for remote diagnosis. Various studies have proven that using the remote screening results in improved quality of life and elevate health outcomes. This method has high accuracy in diagnosis,provided that imaging is done by trained individuals[11].
Due to Iran’s sizeable geographic extent, tele-screening seems to be a feasible response to the unmet needs of the ROP diseases, particularly in remote areas. The launch of such a screening program due to its high start-up costs requires proof of its economic justification, which is done in the health system by economic evaluation tools. Therefore, the purpose of current study is to conduct a cost-effectiveness analysis for tele-ROP screening to identify ROP infants requiring treatment compared to no screening.
SUBJECTS AND METHODS
Ethical ApprovalThe Ethical Committee of Eye Research Center of Tehran University of Medical Sciences approves the study’s protocol (No.ERC/94/3). They verbally express their consent to participate in the study.
Overview of the Model StructureScreening strategy options including two tele-screening and no screening scenarios of premature neonates weighing less than 1500 g or birth before the 30thweek of pregnancy, to identify and treat newborns with ROP disease require treatment are modeled by decision tree analysis. The effectiveness of the scenarios is measured by quality adjusted life years (QALY) index, and the basis for our judgment to determine the cost-effectiveness of tele-screening scenario, compared to the no screening, is the incremental cost-effectiveness ratio (ICER).
In the tele-screening scenario, a reading center in the third-level referral hospital of the Iranian health system and 32 provincial screening centers is considered. For Tehran Province, the capital of Iran, two screening centers are intended. In these centers, all retinal images of suspected infants are taken by a trained nurse using an indirect ophthalmoscope and sent electronically to the reading center. In the reading center, an ROP specialist read the received images and decide about the ROP’s status of the infants, and he/she calls only the infants who need treatment to the referral hospital. In the base model,the coverage level of tele-screening scenario is considered as 80%. The no screening scenario is an approach that is currently being implemented in the country. In this method, some of the suspected infants referred to third-level referral hospitals in three ways: 1) Self-referral after the discharge of the babies from Neonatal Intensive Care Unit (NICU); 2) Examination of the neonates by a retinal specialist at the NICU center and referral of cases requiring treatment; 3) Sending the suspected neonates by ambulance to the referral centers to perform the needed examinations and return the baby to the NICU.
In both screening options, if the threshold ROP is identified and enters the treatment cycle, they will be examined at least at the 33rdweek of gestation and every two weeks until the age of 50wk of gestation. If the ROP disease is observed in the baby during this period, but the severity of the disease does not exceed grade 3, it will not be treated and will only be monitored until the end of the exam period, because we expect all of these babies will return to their normal state of vision.Nevertheless, if their severity will be higher than grade 3, they will probably need treatment. Threshold ROP is defined as “5 or more contiguous or 8 cumulative clock hours (30-degree sectors) of stage 3+ ROP in either zone 1 or zone 2”[12].
Costs CalculationOne hundred twenty-six randomly selected newborns with ROP required treatment were investigated in Farabi Eye Hospital in Tehran Province to determine the type of treatment received, the number of treatments received,and the cost of each of these treatments. For this reason, a questionnaire was developed to measuring the medical direct costs [visit, drugs, intravitreal bevacizumab (IVB) injection,laser therapy, and surgery] and non-medical direct costs (travel,accommodation, and food) for the baby and one companion. A parent of the infant completed the questionnaire in an interview way.
Establishment costs of tele-screening system include the cost of a reading center (a software technician, an ROP expert,and equipment needed including computers, color printers,and high-speed internet) and 32 screening centers located in provincial NICU equipped hospitals (including a trained nurse,an ocular fundus photography apparatus, a computer, and highspeed internet). We applied the bottom-up approach in the cost calculations. The Iranian Rial exchange rate for the U.S. dollar was considered as 39 000 Rial per one USD.
Effectiveness of the Screening ScenariosThe effectiveness of the screening scenarios is calculated using the QALY index. In current study, QALY is equal to the multiplication of neonate’s health utility value in Iranian life expectancy at birth,which is considered 75y. Health utility value was obtained based on Sharma’s recommendation using the formula of utility = 0.374X+0.514, where X is the average of neonate’s visual acuity, which is measured by Snellen chart, in the eye with better vision in different stages of ROP[13]. All QALY values in the base model are discounted annually by 5.8%. So,the total discounted QALY available to an Iranian is 17.97y[14].The study inputs and effectiveness related probabilities used in the model, along with the uncertainties associated with each one, are shown in Table 1.
Diagnosis Accuracy of the Screening ScenariosThe sensitivity and specificity of the remote diagnosis of ROP disease with fundus photography apparatus were reported in Jackson et al’s[15]study as 0.933 and 0.902, respectively. These characteristics for the competitive scenario are reported as 0.867 and 0.962, respectively, by Jackson et al[15]. Allocation of accuracy values for each branch of screened infants in thedecision tree model was applied using the Bayesian theory considering the prevalence rate of 26.1% of ROP in infants below the threshold[2]. The rate of referral for ROP cases requires treatment based on our calculations was considered as 50%.

Table 1 Inputs of the decision tree modeling for cost-utility analysis of ROP screening scenarios
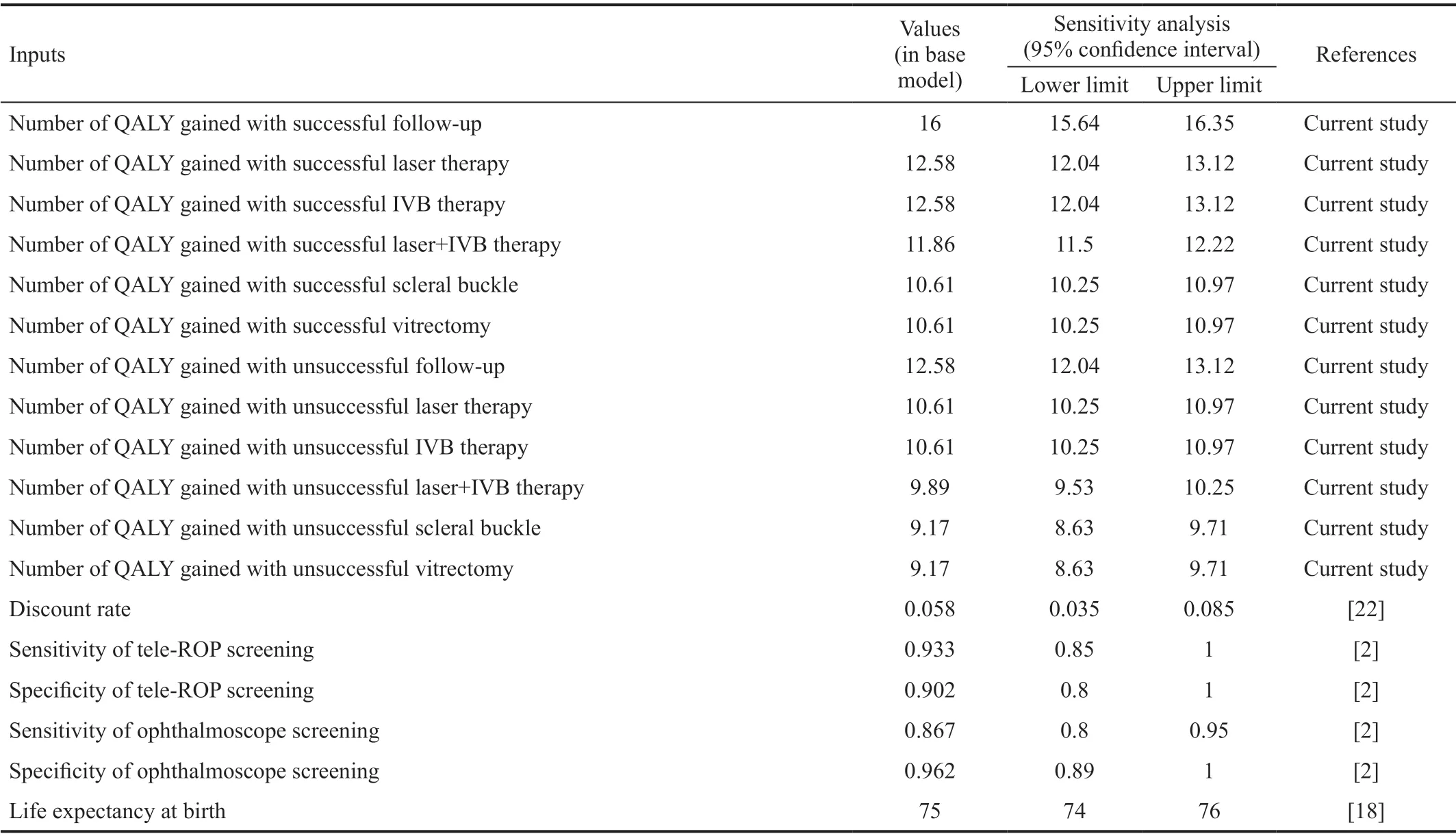
Table 1 Inputs of the decision tree modeling for cost-utility analysis of ROP screening scenarios (Continued)
Cost-Utility AnalysisThe screening strategies’ effectiveness is calculated as the sum of annual discounted QALY’s for a lifetime. While the costs are considered only for the year that screening and treatment services achieved. It is also assumed that the life expectancy of the Iranians is not affected by ROP disease. The final results are calculated using ICER formula, which defined by the difference in cost between two studied screening scenarios, divided by the difference in their effectiveness.
The obtained result is compared with 4616 USD (180 million Rial), a cost-effectiveness threshold, or monetary value of one gained QALY for Iranian people in 2017. If the calculated ICER is less than the above figure, the ROP disease screening scenarios in Iran are cost-effective and otherwise are not costeffective. The figures for cost and effectiveness are calculated using the Monte Carlo simulation that generated 1000 random iteration of the data. Current study is conducted from a societal perspective.
Deterministic Sensitivity AnalysisDue to the uncertainty about model inputs, a one-way sensitivity analysis was performed on the model to determine the effect of changes in the values of model parameters on results. The most important of these variables include the discount rate, treatment costs,cost of setting up a tele-screening system, the coverage rate,the rate of self-referral of the patients, and the disease’s prevalence rate. As shown in Table 1[1-2,15-22], the lower and upper limit of each variable is determined based on the 95%confidence interval of that variable. TreeAge Pro 2012 software(TreeAge Software) was used for this analysis (Table 1).
RESULTS
The total cost of establishing a tele-ROP disease screening system is just over 1.5 million USD. Of this amount, about 1.36 million USD is needed to set up referral centers in provincial centers and about 177 thousand USD to set up a reading center. Therefore, considering the 43 813 newborn infants with ROP each year, the per capita cost required to set up a screening system for each patient with ROP in the country is estimated at 35.13 USD (Table 2).
The total cost of identifying and treating an ROP case in telescreening and no screening strategies were obtained as 108.72 and 63.52 USD, respectively, and also lifetime discounted QALY gained on average for a treated infant are calculated as 15.39 for tele-screening scenario and 15.11 for no screening scenario. Therefore, the ICER of tele-screening strategy against the competitive screening strategy was achieved as 161.43 USD (Table 3).
Findings of the sensitivity analysis show that the lowest and highest ICER values were related to the lower limit for thepatient’s follow-up cost in the tele-screening scenario (98.59)and the upper limit of the discount rate (245.61). In general,the uncertainty about the discount rate variable and the rate of self-referral of patients had the highest and lowest effects on the results, respectively (Table 4).

Table 2 Costs of setting-up a tele-ROP screening system in Iran(in USD)

Table 3 Incremental cost effectiveness ratio of tele-ROP screening against no screening for threshold ROP
DISCUSSION
Tele-ROP screening by setting up screening and referral centers in NICU-equipped hospitals leads to improve access to needed healthcare services and prevention of ocular complications but needs a notable budget. The findings of the current study show that the establishment of the tele-ROP screening system versus no screening requires an additional 45.20 USD per infant with ROP and instead gives him/her more 0.28 QALY (15.39 QALY versus 15.11 QALY). It should be noted that with a discount rate of 0.058, the total QALY available to an Iranian with a life expectancy of 75y is 17.976. Therefore, if ROP infants enter the process of tele-ROP screening, they will lose only 2.585 QALYs, but if he/she is not identified and managed through the screening system, and the current self-referral approach continues, he/she will lose 2.665 QALYs on the average.
The calculated ICER for tele-screening scenario against no screening strategy is 161.41 USD per QALY gained. This figure is much lower than the cost-effectiveness threshold(4616 USD), so establishing the tele-ROP screening system in Iran is very cost-effective and should be considered a priority of the national health system. Interestingly, the sensitivity analysis results have confirmed the cost-effectiveness of the tele-screening strategy in all conditions of uncertainty.Considering the limitations and weaknesses in identifying,following up, and treating newborns with ROP requiring treatment, the tele-screening system seems to be a very suitable option for increasing coverage rate of the patients, reducing ocular complications related to ROP and increase community satisfaction, because there will no longer be any need forfamilies to have unnecessary travels to receive unnecessary healthcare services.

Table 4 One-way sensitivity analysis and incremental costeffectiveness ratio of tele-ROP screening against no screening for threshold ROP
The results of current study are consistent with the findings of Jackson et al[15]and Javitt et al[23]in the United States. In a study by Jackson et al[15], researchers have proven that remote screening is more cost-effective than face-to-face screening with the ophthalmoscope. The average cost per QALY gained in the neonatal tele-screening strategy of babies weighing less than 1500 g, was 3193 USD, and for infants weighing less than 1251 g, was 2807 USD.
In comparison, the ophthalmoscopic screening strategy values were 5617 and 4410 USD, respectively[15]. Javitt et al[23]also reported the average cost-effectiveness of disease management(ophthalmoscopic screening and cryotherapy-treated) at about 2488 to 6045 USD per QALY gained in 1988. The results of these studies directly with the findings of our results are not comparable because the structure of health systems and,therefore, the cost of disease management is different, and more importantly, the results of our and their studies are reported by ICER and average cost-effectiveness ratio indexes,respectively.
The findings of Brown et al[24]confirmed that laser-therapy is more cost-effective than cryotherapy in the treatment of patients with ROP because the average cost per QALY obtained in these treatment methods was 678 and 1801 USD in 1998,respectively. In another related study by Castillo-Riquelme et al[21]in the United Kingdom, it was found that the cost per child screened by the standard digital camera by trained nurses in NICU centers and indirect eye ophthalmoscopes by eye surgeons were 604 and 523 USD, respectively. While this figure for the scenario of screening by a portable digital camera by a trained nurse was 280 USD, which is less than the previous two strategies.
By comparing the achieved ICER for tele-ROP screening with other interventions in the health system, the value and priority of establishing this preventive strategy for receiving the budget is well understood. Imani and Golestani[25]have shown that the most cost-effective drug for controlling multiple sclerosis type Relapsing-Remitting is the Avonex, with an ICER of 607 397 USD. This ratio has been reported as 249 392 USD for the treatment of immune tolerance induction using the bone protocol compared to the Malmo protocol[26], as 516.33 to 126 238 USD for the screening of diabetes type 2 diseases against no screening in different countries[27], and as 6264 USD for breast cancer screening program in Iranian villages[28].Compared with the other interventions, remote screening of ROP disease is much more cost-effective and should be ranked at the top of the league table of all interventions in the Iranian Health System.
Study’s Strengths and LimitationsOne of our study’s strengths, compared to similar studies[15-23,29], is considering the coverage rate of the screening program and the selfreferral rate in the no screening scenario. As shown in the sensitivity analysis results, cost-effectiveness findings change significantly with changes in screening coverage rate and selfreferral rate of the patients in the range of 95% confidence intervals. However, they still confirm the cost-effectiveness of the tele-screening strategy. In reality, one should not expect all babies to be born in hospitals equipped with NICUs and have full access to the screening center. However, in the case of remote screening or no screening, a portion of the population will be self-referred to specialized ophthalmology centers. Considering the sensitivity and specificity of the fundus photography apparatus in the tele-screening scenario and ophthalmoscope in no screening scenario is the another strength of the study. Because in both scenarios, the accuracy of diagnosis is not 100 percent, which leads to the loss of some false-negative patients and the following up the false positive cases and therefore leads to imposing unnecessary costs to the health system and imposing disutility on the needy patients. This subject highlights the sensitivity of identifying,diagnosing, and determining the ROP patients who required medical treatment from the legal point of view. It needs to lay down the laws in this area to eliminate the related risks that threaten the executive staff, especially the ROP specialist, who makes the final decision on the infant’s referral or non-referral.Besides, in current study, for the first time, all treatments associated with ROP disease include follow-up the cases, laser therapy, IVB injection, laser therapy plus IVB injection, scleral buccal surgery, and vitrectomy in the analysis of the results,which led to the reporting the probabilities of receiving, the cost, the utility, and ultimately the QALY obtained in each of these treatment methods. Another advantage of current study,compared to Jackson et al[15]study, is the use of the societal approach in cost analysis, which has led to considering the medical and non-medical direct costs of receiving ROP cares.In contrast, in the study of Jackson et al[15], only medical direct costs included visits and treatment is considered.
Current study is not without limitations and the results of the study should be interpreted in light of these constraints.In the cost calculations, only public sector expenditures are considered, while part of childbirth is done at private centers with much higher tariffs. Taking into account private sector tariffs will raise the ICER’s value, which will require further study to address its magnitude. Due to the lack of economic stability in the Iran market, the price of medical equipment such as fundus photography and ophthalmoscope is variable and growing. Another limitation of the study was the nondifferentiation of the infants based on unilateral or bilateral ROP involvement due to a lack of access to relevant statistics in infants born in Iran.
ACKNOWLEDGEMENTS
Authors’ contributions:Mohammadi SF, Darabeigi S, Farahani A, Lashay A have been participated in conceptualization/design, collecting data, manuscript review.Rahban A and Salimi N have been participated in collecting data, literature search, and preparing manuscript. Alinia C has been participated in conceptualization/design, collecting data,analyzing statistical, preparing, and editing manuscript.
Foundation:Supported by the Deputy of Health of Iranian Ministry of Health (No.1602005000).
Conflicts of Interest:Mohammadi SF,None;Rahban A,None;Darabeigi S,None;Salimi N, None;Farahani A,None;Lashay A,None;Alinia C,None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
