Spasm of the near reflex: a common diagnostic dilemma?
Eleni Papageorgiou, Dimitrios Kardaras, Eftychia Kapsalaki, Efthymios Dardiotis, Asimina Mataftsi, Evangelia E. Tsironi
1Department of Ophthalmology, University Hospital of Larissa,Larissa 41222, Greece
2Department of Radiology, University Hospital of Larissa,Larissa 41222, Greece
3Department of Neurology, University Hospital of Larissa,Larissa 41222, Greece
42nd Department of Ophthalmology, Aristotle University of Thessaloniki, Thessaloniki 41222, Greece
Abstract
● KEYWORDS: accommodative spasm; bifocal glasses;convergence spasm; pseudomyopia; spasm of the near reflex; screen time
INTRODUCTION
Spasm of the near reflex (SNR) is an uncommon entity, which results from over-stimulation of the parasympathetic nervous system, and is clinically characterized by episodes of accommodation spasm (AS), esotropia with variable angle and pupillary miosis[1]. Patients usually present with intermittent episodes of diplopia and blurred vision. Further clinical manifestations are micropsia or macropsia, as well as nonspecific symptoms, such as fluctuation of vision, headache,ocular pain, and dizziness[2-4]. Some patients may demonstrate only AS (pseudomyopia) without esotropia and miosis. The condition has been also described in children, mainly in the prepubertal and pubertal age group in female patients[2-3].Although the most common aetiology for SNR is functional or psychogenic, it has been infrequently associated with head trauma[3,5-6], neurological disease, such as myasthenia gravis[2],multiple sclerosis[7], meningitis[7], pituitary tumor[8], Arnold-Chiari malformation[7], photosensitive epilepsy[7], stroke[7], and ocular or systemic drugs[1-3].
The rare association of SNR with underlying neurological conditions, and the fact that the signs and symptoms of SNR are usually intermittent and nonspecific, lead to frequent diagnostic problems, involvement of various medical subspecialties and unnecessary and stressful investigations.For example, SNR in paediatric patients has been occasionally misdiagnosed as bilateral sixth nerve paresis, horizontal gaze palsy, oculomotor apraxia, acute esotropia and retrobulbar optic neuritis[3,9-10].
Aim of this study is to report the clinical characteristics and diagnostic procedures used in patients with SNR across two specialist centres in Greece, in order to present common investigation strategies and diagnostic pitfalls.
SUBJECTS AND METHODS
Ethical ApprovalThe study was performed according to the Declaration of Helsinki, and was approved by the local Ethics Committee. All subjects or their legal guardians gave their written informed consent for inclusion of their data.This was a retrospective study of all patients diagnosed with SNR between November 2017 and November 2019 in the Paediatric Ophthalmology and Neuro-Ophthalmology Clinics of two tertiary referral centres.
The study included 22 patients. There were 20 children under 13 years of age and 2 adults, 23 and 33 years old. SNR was a clinical diagnosis on the basis of blurred vision, variable esotropia, miosis, and a difference of 2.00 dioptres (D) or more between manifest (dry) and cycloplegic (wet) retinoscopy,as defined previously[3]. All patients underwent visual acuity testing, orthoptic evaluation, assessment of refraction before and after cycloplegia, and dilated fundoscopy. In some of the patients, paediatric and neurological consultations,neuroimaging, lumbar puncture (LP), blood tests and electrophysiology were also performed. Screen use among children was assessed in hours/day according to parents’reports. Screen time included time spent watching television or videos, time spent on computers, video game consoles, mobile devices, or cell phones.
RESULTS
Table 1 summarizes the clinical findings at the initial and final examinations. There were 17 patients with AS and 5 patients with SNR. The age range was 7-33y (median=10y). There were 19 females and 3 males.
SymptomsFour children did not report any symptoms and were referred due to low academic performance. Eighteen patients (82%) complained of reduced or blurred vision and five of them reported reduced visual acuity in conjunction with diplopia (Video 1, online supplementary). Other symptoms included headache, dizziness, and ocular pain.
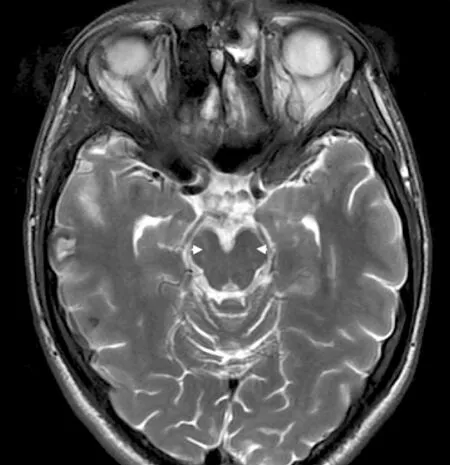
Figure 1 Axial T2 susceptibility weighted image Multiple small areas of hemosiderin deposits (appearing as small low signal areas on T2 images) are identified in the cerebral peduncles bilaterally (white arrowheads) and the reticular formation area on the left, and represent areas of diffuse axonal injury from the previous head trauma.
Patient #22 with Spasm of the Near ReflexThe patient presented with variable esotropia, abduction deficit,pseudomyopia and miosis. The miosis and abduction deficit resolve with occlusion of one eye by disrupting the binocular input necessary for convergence (Video 1, online supplementary).
RefractionVisual acuity was equal or less than 20/125 in three cases (14%), between 20/125 and 20/40 in eleven cases(50%) and equal or better than 20/40 in eight cases (36%).The duration of symptoms at the time of presentation ranged from 1d to 2mo. Bilateral visual involvement was reported in all patients. At presentation all patients presented with myopic refractive error, which showed fluctuation during dry retinoscopy (range -0.50 to -13 sph. D). After cycloplegia, 20 out of 22 patients had hypermetropia (range +0.25 to +2.50 sph. D),and two patients had myopia (range -1.00 to -2.50 sph. D).
InvestigationsSix patients (27%) had underwent brain magnetic resonance imaging (MRI) before evaluation by an ophthalmologist; however, only one patient (#18) had a history of a traumatic head injury due to a car accident 3 years ago (Figure 1). Patient #22 was initially assessed by a neurologist by means of brain MRI, LP, visual evoked potentials (VEPs) and acetylcholine receptor antibodies, in order to exclude multiple sclerosis and myasthenia gravis. Two children (#16 and #17) presented to the Paediatric Emergency Department with blurry vision and diplopia, which led to initial misdiagnosis of optic neuritis, brain MRI, LP and intravenous steroid therapy before presentation to an ophthalmologist. Two additional children (#7 and #15) had undergone brain MRI after a paediatric consultation, in order to exclude intracranial causes of reduced vision.
An anterior segment optical coherence tomography (OCT)before and after cycloplegia (Visante-OCT, Carl Zeiss Meditec, Dublin/USA) was performed in patient #16 (Figure 2).The change in anterior chamber depth after cycloplegia was0.28 and 0.21 mm in OD (Figure 2C) and OS respectively(Figure 2D). This is very similar to the reported change (mean 0.28 mm, range 0.14-0.44) among children without SNR, aged 4-14y[11]. Interestingly, mean screen time was 4±1.2h/d.
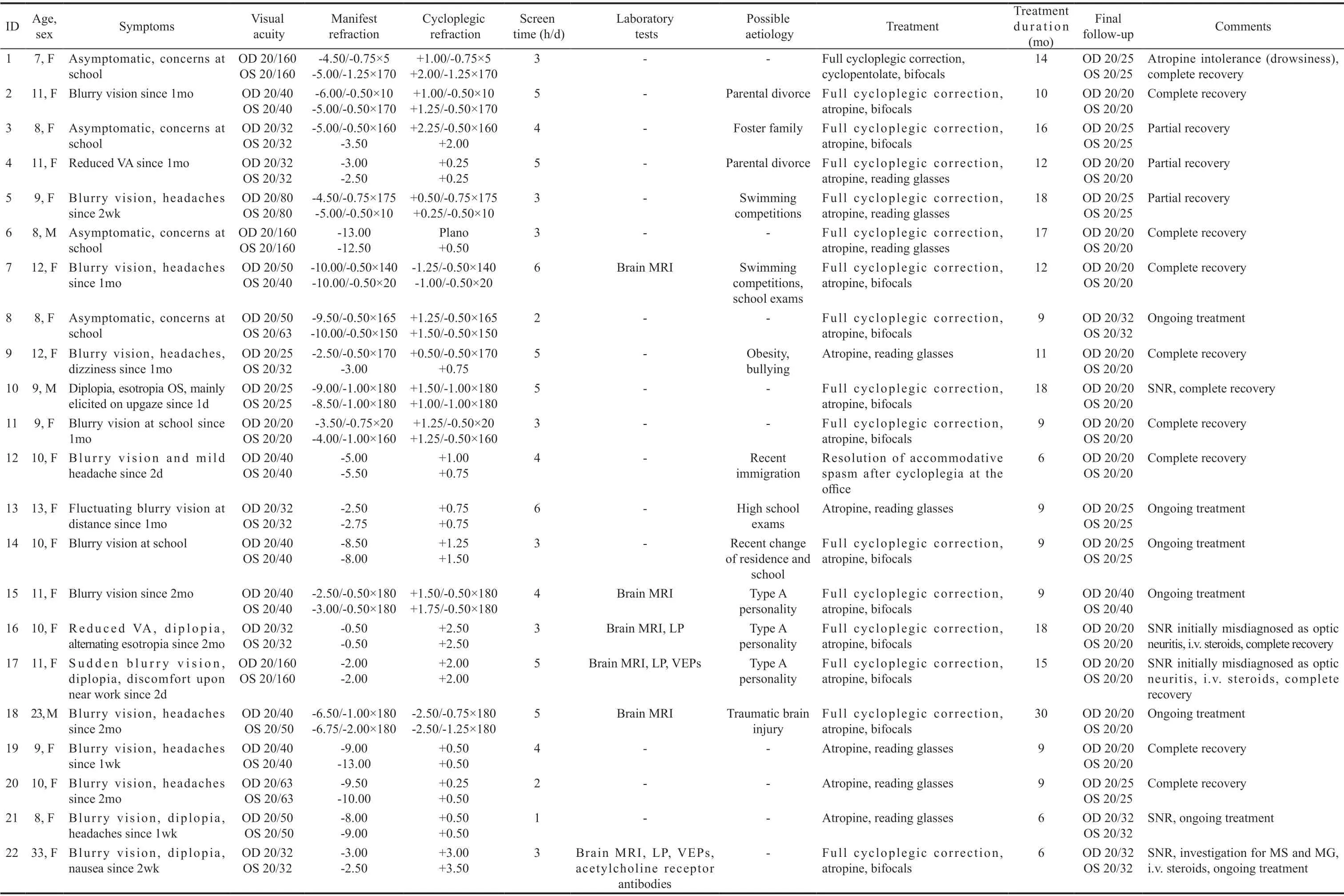
Table 1 Clinical findings at the initial and final examinations of the 20 children with accommodative spasm

Figure 2 Anterior segment OCT of patient #16 A: OCT before cycloplegia in OD; B: OCT before cycloplegia in OS; C: The change in anterior chamber depth after cycloplegia was 0.21 mm in OD; D: The change in anterior chamber depth after cycloplegia was 0.28 mm in OS.
AetiologyIn 21 out of 22 cases SNR was functional in origin,apart from patient #18, who had suffered a traumatic brain injury. In twelve patients (55%) concurrent social problems were reported by themselves or the caregivers, i.e. school exams, bullying, sport competitions, parental separation or divorce.
TreatmentThe treatment offered to all patients consisted of careful explanation of the condition, atropine 1% eye drops and full cycloplegic correction by means of bifocal glasses. The dosing scheme of atropine was analogous to disease severity,ranging between once daily and once per week. In one patient,AS resolved before initiation of atropine, possibly due to office cycloplegia.
Mean duration of treatment was 13mo (range 6-30mo). In all cases atropine was gradually tapered over a period of several weeks. At final follow-up, all patients had a visual acuity of 20/25 or better in both eyes. Twelve patients experienced complete resolution of symptoms. Three patients reported occasional blurry vision after cessation of treatment,without evidence of disease recurrence on ophthalmological examination, hence they were classified as having partial resolution of the condition.
DISCUSSION
This study provides evidence that SNR may be underrecognized,as a large percentage of patients underwent a series of laboratory tests before ophthalmological assessment. Five patients in this study (23%), four children and one adult,had undergone a brain MRI due to unexplained visual loss,before a cycloplegic refraction indicated the diagnosis of SNR. Further paraclinical investigations, such as LP and VEPs were also pursued, perhaps reflecting the need to avoid missing more ominous diagnoses in a sensitive population.Three patients in our series even received intravenous steroid treatment before ophthalmological assessment. Because of the diplopia, esotropia and blurry vision, patients with SNR may be initially mistaken as having a unilateral or bilateral sixth nerve palsy or optic neuritis and undergo extensive neurologic and neuroimaging investigations[9-10]. Some of these tests are invasive, especially for children, costly and time-consuming. Extraocular muscle surgery performed on patients with SNR who were incorrectly diagnosed has been also reported[10]. Affected children may be also misdiagnosed as having childhood esotropia, nystagmus blockage syndrome divergence insufficiency, horizontal gaze palsy, oculomotor apraxia, convergence retraction nystagmus, and true myopia[12].Additionally, young children may be reluctant in reporting visual loss, or may not be able to describe a visual disability.Especially AS may be underdiagnosed in children, as it is not accompanied by esotropia, which can be easily noticed by an adult observer. Hence, considering SNR in patients presenting with episodic diplopia with normal conjugate eye movements and intermittent blurry vision, is important not only for ophthalmologists, but also for neurologists,paediatricians and emergency department staff. Assessment of refraction before and after cycloplegia is an easy, non-invasive,and cost-effective test, which establishes an accurate and prompt diagnosis, avoiding the need for costly and stressful procedures.
DiagnosisThe diagnosis of SNR is clinical and can be made promptly on the basis of ophthalmological findings in the great majority of cases. Patients with isolated AS exhibit blurred vision (especially for distant objects), fluctuating vision, asthenopia, ocular discomfort, poor concentration, and headaches[3]. Refraction with and without cycloplegia will establish a greater myopia on dry compared to wet retinoscopy,the difference ranging from 1 to 10 D[6]. A diagnostic hint for the clinician is that visual acuity before cycloplegia usually fluctuates, does not correlate with the degree of pseudomyopia and does not improve substantially by using minus corrective lenses. This is possibly due to the fact that the episodes of SNR are intermittent and may be elicited by attempts to fixate on an object or by looking at a specific gaze direction[1]. In addition to pseudomyopia, in patients with SNR the apparent limitation of abduction under binocular conditions will disappear when one eye is patched[10]. Miosis will also resolve when either eye is occluded[13]. Observation of miosis is a useful clinical sign that simplifies the diagnosis, but it can be difficult to notice especially in children. Although definite conclusions should be based on a larger sample of patients, it seems that anterior segment OCT is not helpful in the diagnosis of SNR, as it did not demonstrate any particularities in the structure nor in anterior chamber depth changes upon cycloplegia. A careful neurologic and neuro-ophthalmologic examination will ensure that an associated central nervous system disorder is not the cause of the spasm[12,14]. Further neuroimaging and laboratory tests will be required only in very rare instances, based on the history and additional symptoms.
AetiologyRegarding the aetiology, 21 out of 22 cases of SNR in the present series were nonorganic, with 12 out of 22 (55%) children or their caregivers reporting difficulties at home or school. This compares well with previous studies on the frequency of underlying anxiety in children with functional visual loss, which was at 36% in the study by Lim et al[15], at 40% in the study by Catalano[16], at 60% in the study by Bain et al[17], and at 90% in Keltner et al’s study[18]. Additionally, our data suggest that we encounter this condition more often in the last few years and one can speculate that there is a link with the widespread usage of electronic gadgets and excessive amount of time spent in front of digital screens. In the present study,90% of children presented prolonged daily screen time (>2h/d). These findings are in agreement with recent studies from Greece and Sweden, which showed that a large percentage of children exceed the recommended guidelines for daily screen time[19-20]. Hence accommodative disorders, such as AS, may become more frequent in children in the future, and larger studies should determine if prolonged screen use is a definite risk factor for the development of AS in children[21-22].
In the present study only one patient (#18) had a history of traumatic brain injury, consistent with previous reports that organic causes of AS are rare[1,3]. In this case, AS was evident even after 30mo of treatment with atropine[6]. Post-traumatic AS may represent traumatic activation or disinhibition of putative brainstem accommodation centers[6,23]. Neuroimaging reports of patients with SNR due to head trauma are rare and suggest a possible lesion of the upper brainstem, the left temporal lobe, the frontal and parieto-occipital lobes, and the cerebellum[24]. Our patient had multiple lesions in the cerebral peduncles, and the reticular formation area, suggesting that the midbrain is probably the region associated with post-traumatic AS.
TreatmentThe most common problems that clinicians face in the management of children with AS are the refraction to prescribe and the pharmacological protocol to treat the condition. Although nonorganic AS can resolve spontaneously over time, treatment is usually indicated because of the symptoms. Management should begin with identification of the underlying aetiology and simple reassurance that that the condition does not cause an irreversible visual or neurologic disorder. Treatment options include cycloplegic agents, full cycloplegic correction, bifocal lenses, partial occlusion, miotic agents, referral for psychiatric counselling, surgery, and botulinum toxin.
In this study, the combination of cycloplegic agents (atropine 1% or cyclopentolate 1% eye drops) and bifocal spectacles(near addition +2.50 sph. D) was the first-line treatment of AS. This treatment scheme was successful in 60% of patients, while 20% of patients reported partial resolution of symptoms. Long-term follow-up, prolonged use of cycloplegic medications, and gradual weaning of treatment are suggested, as recurrence of AS has been reported following discontinuation of treatment[3,25-26].
This study demonstrated that, although SNR is rarely associated with neurologic disease, a large percentage of patients are subjected to redundant neuroimaging and paraclinical investigations. Due to the widespread usage of digital screens and electronic devices the condition may be encountered more often in the near future. Hence, clinicians should be aware of the clinical spectrum of SNR, in order to avoid unnecessary investigations and treatment.
ACKNOWLEDGEMENTS
Conflicts of Interest: Papageorgiou E,None;Kardaras D,None;Kapsalaki E,None;Dardiotis E,None;Mataftsi A,None;Tsironi EE,None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
