Clinical performance of presbyopia correction with a multifocal corneoscleral lens
Woo Chan Park, Chae Hoon Kim, Sang Wook Jin
Department of Ophthalmology, Dong-A University College of Medicine, Busan 49201, Republic of Korea
Abstract
● KEYWORDS: presbyopia; multifocal lens; corneoscleral lens
INTRODUCTION
Presbyopia refers to the aging-related loss of ability or control to alter the lens to see nearby objects. Unlike refractive error, in which genetic and environmental factors affect the shape of the eyes, presbyopia occurs primarily in people aged 50-69y or older[1-3]. It is estimated that there were 1 billion people with presbyopia worldwide in 2005, and that number is expected to increase sharply to 1.9 billion people by 2020[4].
There are various strategies and modalities for correcting presbyopia. Strategies for correcting presbyopia include placing separate optical devices in front of the visual system or changing the direction of the gaze to look through optical zones of different optical powers[5], monovision[6-7], simultaneous images[8-9], pinhole depth of focus expansion[10], and restored accommodative dynamics[11]. Among these strategies,monovision is commonly used. Monovision is when an unbalanced correction between the two eyes corrects one more for far vision and the other for intermediate or near distances[2].However, monovision has some limitations, such as a reduction in contrast sensitivity and stereopsis and difficulty of adaptation[12-13]. The multifocal corneoscleral lens comprises a distance lens (D-lens) and a near lens (N-lens). The D-lens and N-lens have near vision at the center and far vision at the periphery. However, the D-lens has a larger peripheral area than center area, and the N-lens had a larger center area than peripheral area. Therefore, the multifocal corneoscleral lens could offer greater advantages than monovision in terms of contrast sensitivity, stereopsis, and adaptation.
Various nonsurgical and surgical modalities have also been attempted for presbyopia correction[5-17]. Nonsurgical modalities for presbyopia correction include using near spectacles[4-5], multifocal spectacles[4-5], and multifocal soft contact lenses (SCLs)[14-16]. These modalities for correcting presbyopia have some limitations. The use of near spectacles to correct presbyopia has the disadvantages of discomfort from having to wear glasses whenever needed and not being able to resolve intermediate vision. Multifocal spectacles have the advantage of resolving far, intermediate, and near vision all at once. However, they still have the disadvantage of being difficult to adapt to and causing discomfort. Multifocal SCLs for presbyopia correction can overcome the disadvantages of glasses. However, they also have the disadvantages of having low patient adherence due to discomfort when wearing them, exacerbation of dry eye symptoms, reduction in the efficacy of astigmatism correction due to inaccurate positioning of the SCL, and a low success rate due to fitting difficulty. Moreover, although there are industry-provided fitting guidelines, accurate prescriptions are still difficult to obtain due to the high number of subjective elements,such as slit-lamp biomicroscopic findings determined by ophthalmologists[12-13]. The corneoscleral lens was developed to overcome the disadvantages of SCL, such as exacerbation of dry eye and reduction in visual acuity (VA) due to dryness and astigmatism[18]. Surgical modalities include accommodative intraocular lens (IOL)[19], scleral expansion band[20], anterior ciliary sclerostomy[20], multifocal IOL[21-22], corneal surface surgery[20], and corneal inlay surgery[23].
The purpose of this study was to evaluate the efficacy and safety of the newly developed multifocal corneoscleral lenses for presbyopia correction with the aim of overcoming the disadvantages of existing presbyopia correction strategies and modalities.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Institutional Review Boards of the Dong-A University and conducted adhere to the tenets of the Declaration of Helsinki.Informed consent was obtained from each participant. This study was registered with the Clinical Research Information Service (KCT0004485).
The sample size was calculated using G*Power (Faul,Erdfelder, Lang, & Buchner, 2007). A minimum of 28 participants was required given an alpha of 0.05 and a 1-beta of 0.80. Consecutive enrollment of participants continued until the number of enrolled participants exceeded the required minimum number of participants. A prospective study was conducted on 40 patients with presbyopia involving myopia or hyperopia who were aged between 45 and 60y and had visited an outpatient ophthalmology clinic. Six participants dropped out. Thirty-four participants finished the study. Patients with the following characteristics were excluded from the study: 1)astigmatism >0.75 D, amblyopia, heterotropia or anisometropia(>1.00 D mean spherical equivalent difference between eyes);2) ophthalmic disease or abnormalities, including corneal endothelial dystrophy or guttata; 3) allergies to the contact lens; 4) systemic diseases such as diabetes, hypertension,or autoimmune disease; 5) history of eye surgery; and 6)others deemed inappropriate for the study by the principal investigator.
The multifocal corneoscleral lens used in the present study was the Onefit™ A (Blanchard Contact Lens Inc., Manchester,USA). The Onefit™ A has an overall diameter of 14.7 mm and comprises an optical zone for adjusting the curvature according to the sagittal height to ensure that the center does not come in contact with the cornea; a vaulting zone for adjusting the lens fit to ensure that the lens does not touch the corneoscleral junction; and a landing zone that sits on the conjunctiva. The multifocal corneoscleral lens is composed of a D-lens and an N-lens. All lenses were fabricated using Boston XO DK 100 (Polymer Technology Corporation, Boston, MA, USA)material.
The topographic radius of the curvature and the white-towhite length of the cornea were measured using tomography(Pentacam; Oculus Inc., Wetzlar, Germany) and RTVue-100 optical coherence tomography (Optovue Inc., Fremont,California, USA) to begin the fitting process with trial lens sets. A good fit was defined as having acceptable apical clearance (the distance between the posterior surface of the corneoscleral lens and the apex of the anterior corneal surface) and limbal vault (the distance between the posterior surface of the corneoscleral lens and the anterior corneal surface, measured vertically at 1.5 mm from the scleral spur).Fit was measured using the RTVue-100 after the patient had worn the corneoscleral lens for 30min and had shown no keratitis, conjunctival hyperemia, or ischemia due to compression of the conjunctiva by the peripheral edges of the corneoscleral lens on slit lamp microscopy after 1-2h of wearing the trial lens. RTVue-100 anterior segment optical coherence tomography (AS-OCT) was used to determine the appropriate conjunctival clearance, while the appropriate apical clearance and limbal vault were determined to be 150-175 μm and 80-100 μm, respectively. Subsequently, the holein-the-card test was performed to determine the dominant eye, and the decision was made to prescribe the D-lens for the dominant eye and the N-lens for the nondominant eye. An overrefraction exam was performed after the optimal lens was placed on the eye to determine the appropriate parameters.At far distance (5 m), overrefraction was performed to reach the optimal best corrected visual acuity (BCVA). At near distance (40 cm), a lens with the value determined during far distance overrefraction was placed in a trial frame, and the near vision was evaluated. When the ordered lenses arrived,the patients were instructed to visit the clinic. The patient tried on the first set of lenses ordered, and if they fit the patient’s corneosclera properly and there was good VA (i.e., if it was not inferior to the patient’s previous BCVA) and fit sensation,the patient was trained on how to use the plunger to insert and remove the lenses and on methods for using the lens solution(Queen’s Plurisol R SOLEKO Co., Italy) for cleaning, wetting,and storing the lenses. Similar to other corneoscleral and miniscleral lenses, corneoscleral lens application requires the bowl to be filled with solution. Preservative-free saline solution or preservative-free artificial tears are preferable. The patient is instructed to tilt his or her head forward and bring the lens up to the eyeball. There should never be a bubble under the lens after it is placed on the eye. The duration of lens-wearing time was set to four hours on the first day and increased by one hour each day, and the patients were instructed to visit the clinic again in one week. During the revisit, if how the lenses stayed in, the VA, and the fit sensation were all satisfactory, the patient was instructed to return within two weeks and at one month intervals thereafter. If the first pair of lenses ordered was unsatisfactory, the lenses were reordered after appropriately adjusting the lens parameters.
The study analyzed the change in binocular VA at far distance(5 m), intermediate distance (100 cm), and near distance (40 cm),satisfaction and discomfort with wearing the lenses, central corneal thickness (CCT), corneal endothelial cell count,binocular stereopsis, and tear break-up time (BUT). VA at far and intermediate distances was measured by the Logarithmic Visual Acuity Chart 2000 New ETDRS (Precision Vision),and VA at near distance was measured by the Jaeger near VA chart. CCT and corneal endothelial cell count measured at 1wk after the multifocal corneoscleral lens was removed. To assess satisfaction with wearing the lenses, five items (fit sensation,VA at far distance, VA at intermediate distance, VA at near distance, and ease of handling) were surveyed after one month of wear, and the responses were graded on a 1- to 5-point scale.In this survey, a higher value indicates better performance,and the baseline satisfaction score of the participant was 1.For discomfort, six items (dryness, eye irritation, foreign body sensation, redness, fogging, and halo) were surveyed, and the responses were graded on a 1- to 5-point scale. In this survey,a lower value indicates better performance, and the baseline discomfort score of the participant was 1. CCT was measured by tomography (Pentacam; Oculus, Wetzlar, Germany), while corneal endothelial cell count was measured by specular microscopy (Konan NSP-9900; Konan Medical, Inc., Hyogo,Japan). Binocular stereopsis was measured at a distance of 40 cm (16 inches) using the Titmus Stereo Test (2009 Stereo Optical Co., Inc.). Slit lamp microscopy was used to assess corneal staining, corneal edema, corneal neovascularization(NV), and conjunctival hyperemia. Corneal staining was determined using reference photographs[24]. Abnormal corneal staining findings were defined as grades 2-5. Corneal edema was graded as follows: 1) grade 0=no edema; 2) grade 1=none to minimal; 3) grade 2=mild to moderate (visible iris details);4) grade 3=moderate to severe (obscuring iris details); and 5)grade=marked (obscuring pupil)[25]. Abnormal corneal edema was defined as grades 1-5. Corneal NV was determined using reference photographs[24]. Abnormal corneal NV findings were defined as grades 1-3. Conjunctival hyperemia was determined using reference photographs (Contact Lens Research Unit grading scales)[26]. Abnormal conjunctival hyperemia findings were defined as grades 3-4. Moreover, spherical equivalent values calculated by manifest refraction were used to divide the patients into myopia (spherical equivalent refraction less than -0.50 D), emmetropia (spherical equivalent refraction between -0.5 D and 0.5 D), and hyperopia (spherical equivalent refraction greater than 0.50 D) groups, and the survey results for satisfaction, discomfort, and willingness to continue to wear the corneoscleral lenses were compared and analyzed among the groups.
Statistical AnalysisSPSS for Windows (SPSS Version 22.0 Inc., Chicago, IL, USA) was used for statistical analysis. The Wilcoxon signed rank test was used to compare the changes in BCVA, CCT, corneal endothelial cell count, binocular stereopsis, and BUT from before lens use to after 4wk of continuous wearing of the corneoscleral lenses. A onesample Z-test was used to compare the changes in corneal staining, corneal edema, corneal NV, and conjunctival hyperemia. The Mann-Whitney U test was used to compare satisfaction, discomfort, and willingness to continue to wear the corneoscleral lenses among the myopia, emmetropia, and hyperopia groups. The results with P<0.05 were considered statistically significant.
RESULTS
From a total of 40 participants, data from 34 participants were used in the final analysis after excluding four participants who were lost to follow-up and two participants who dropped out because of poor compliance with lens fitting during the study. Regarding sex, there were 7 males (20.6%) and 27 females (79.4%), and their mean age was 53.0±4.9y. The mean uncorrected binocular visual acuity (UCVA) at far,intermediate, and near distances was 0.33±0.42, 0.39±0.34,and 0.44±0.31 (logMAR), respectively. The mean pupil size under 500 lx was 4.78±0.57 mm. The mean total number of corneoscleral lens fitting trials required before a good fit was achieved was 1.46±0.29 times (Table 1).
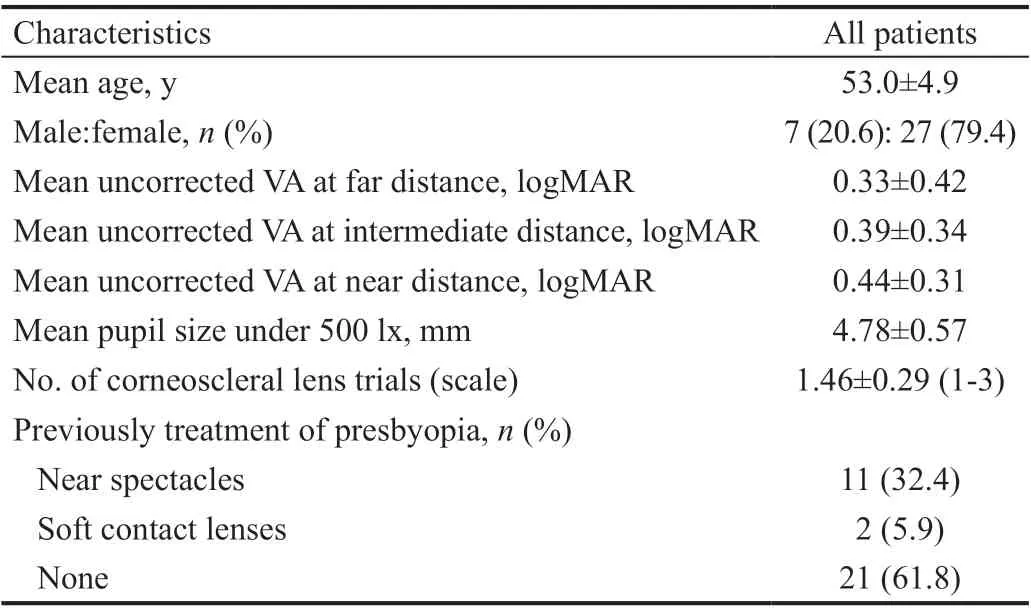
Table 1 Clinical and demographic data of the patients n=34

Table 2 Comparison of UCVA and contact lens corrected binocular VA logMAR
The results of the comparison of UCVA and contact lens corrected binocular VA are shown in Table 2. The corneoscleral lenses corrected binocular VA was better than the UCVA.These differences were statistically significant (Table 2).
Comparisons of CCT, corneal endothelial cell count, binocular stereopsis, and BUT before and 4wk of continuous wear of the corneoscleral lenses showed no statistically significant differences (Table 3).
Satisfaction with wearing corneoscleral lenses was surveyed after 4wk of continuous wearing of the corneoscleral lens.Table 4 shows the mean score for fit sensation, VA at far distance, VA at intermediate distance, VA at near distance, and ease of handling.
Regarding discomfort with wearing corneoscleral lenses after 4wk of continuous wear, the mean scores for dryness, eye irritation, foreign body sensation, redness, fogging, and halo are shown in Table 5.
The comparison results for corneal staining, corneal edema,corneal NV, and conjunctival hyperemia based on slit lamp microscopy are shown in Table 6. Corneal staining, corneal edema, corneal NV, and conjunctival hyperemia were not significantly different between baseline and after 4wk of continuous wearing of corneoscleral lenses.
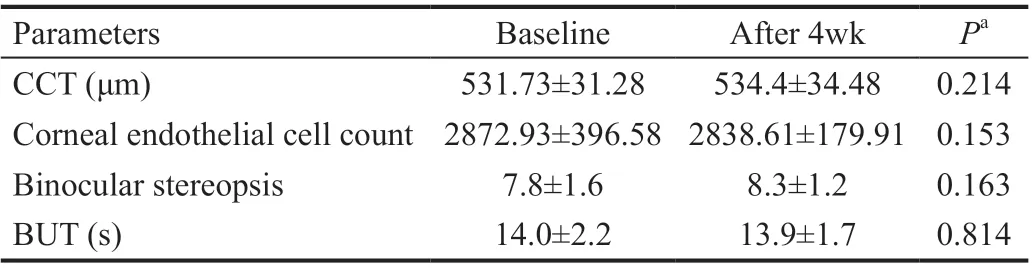
Table 3 Comparison of CCT, corneal endothelial cell count,binocular stereopsis, and BUT
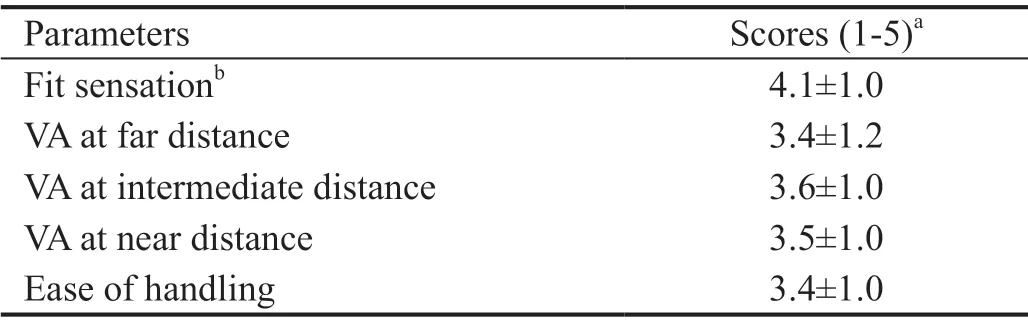
Table 4 Response scores for the satisfaction questions
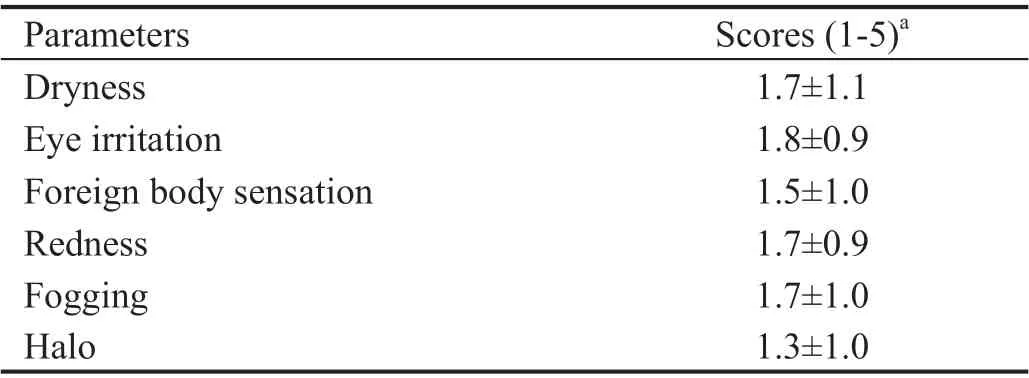
Table 5 Response scores for the discomfort questions
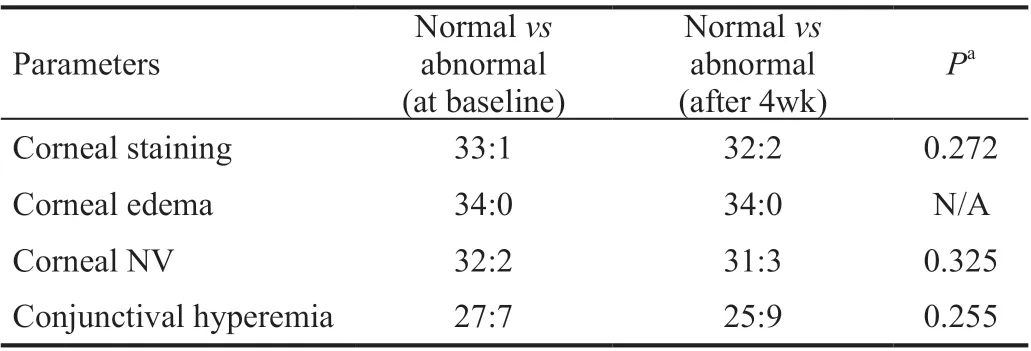
Table 6 Comparison of corneal staining, corneal edema, corneal NV, and conjunctival hyperemia
The comparison results for the myopia, emmetropia, and hyperopia groups are shown in Table 7. The patients in the myopia group had higher satisfaction scores for VA at far distance, VA at near distance, and ease of handling after wearing the corneoscleral lenses than the patients in the emmetropia and hyperopia group did. The patients in the myopia group showed significantly greater willingness to continue to wear the corneoscleral lenses than the patients in the emmetropia and hyperopia groups did.
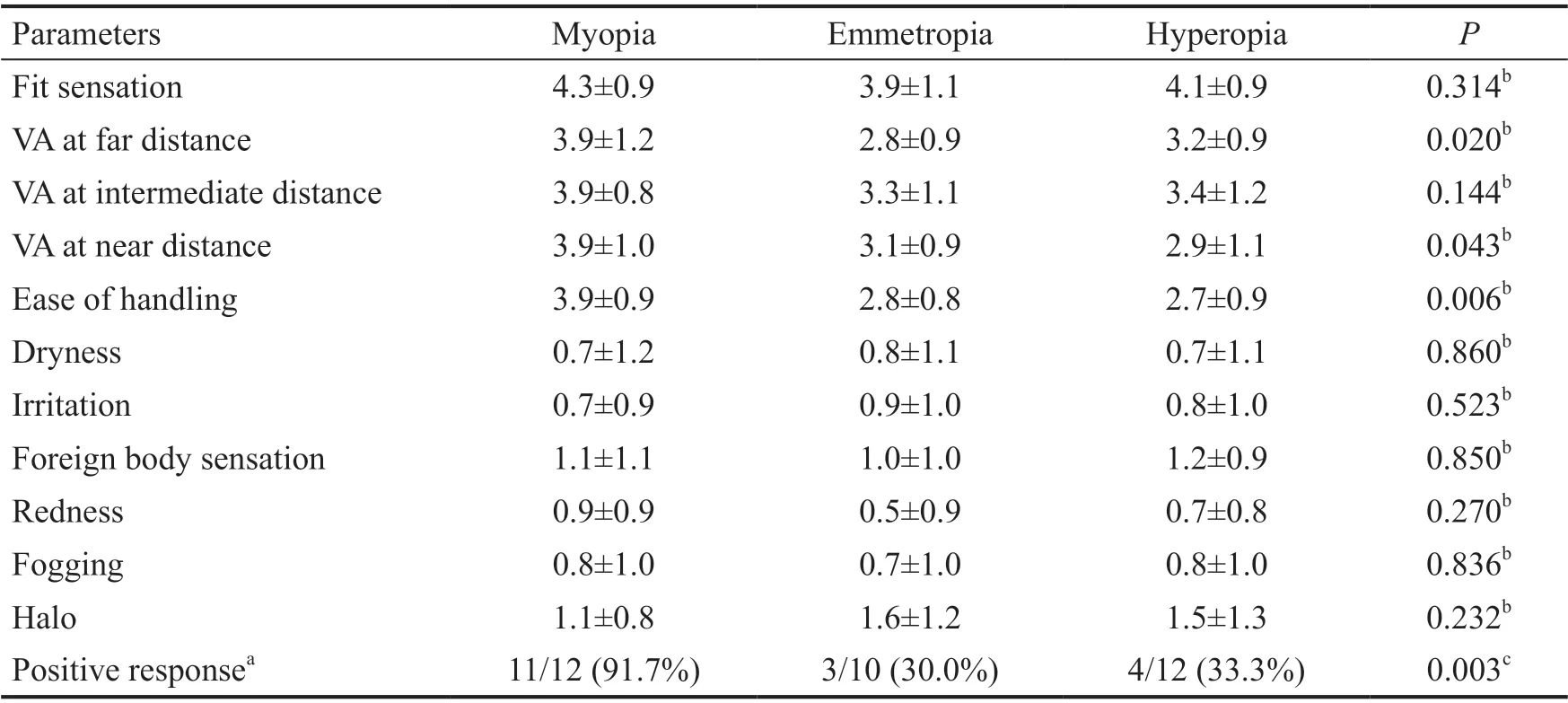
Table 7 Comparison among the myopia, emmetropia, and hyperopia groups
DISCUSSION
Presbyopia is a refractive condition in which the accommodative ability of the eye is insufficient for near vision work due to aging. Many studies have suggested strategies and modalities to correct presbyopia. However, these methods had some limitations, such as reduced contrast sensitivity and stereopsis,difficulty of adaptation, and dryness. The present study was a single-center, prospective experimental study that aimed to investigate the presbyopia correction effect of a multifocal corneoscleral lens to overcome the disadvantages of existing presbyopia correction strategies and modalities.
Sivardeen et al[6]demonstrated that a presbyopia-correcting contact lens using the monovision technique had a good correction effect and clear focus. Labiris et al[7]demonstrated that pseudophakic monovision seems to be an effective method for correcting presbyopia, with high rates of spectacle independence and minimal dysphotopsia side effects. Richdale et al[27]conducted a prospective randomized controlled trial study on the efficacy of multifocal and monovision SCLs for presbyopia. They demonstrated that multifocal SCLs provide excellent visual acuity without compromising stereoacuity. We confirmed that the multifocal corneoscleral lens is efficacious for presbyopia correction. In our study, the corneoscleral lens improved VA at far, intermediate, and near distances to logMAR 0.08±0.11, 0.10±0.12, and 0.10±0.12, respectively.In addition, the participants had high satisfaction with wearing multifocal corneoscleral lenses for presbyopia correction. The efficacy for presbyopia correction observed in our study was consistent with the findings of previous studies using other presbyopia correction strategies or modalities.
Presbyopia correction strategies and modalities have their limitations. The limitation of using near and multifocal spectacles for presbyopia correction has been reported in various studies. Image jump as the wearer’s fixation axis crosses the top edge of the bifocal and distortion of peripheral vision with the progressive lens may make the patient’s judgment of object position and movement in the local environment less certain. This in turn can lead to a significantly increased risk of accidents in elderly, at-risk individuals,particularly when descending stairs[5,16]. When presbyopia occurs in people who had previously worn SCLs, they continue to wear SCLs for far-distance tasks and use near spectacles for near-distance tasks. The disadvantages of this method include the inconvenience of having to wear and take off the spectacles and discomfort and limitations during outdoor activities.
Another presbyopia correction method is far vision correction using an SCL in one eye and a near vision correction SCL in the other eye. However, this method has reduced contrast,stereopsis and difficulty of adaptation[12-13]. We compared stereopsis before and 4wk after the continuous wearing of multifocal corneoscleral lenses. In our study, there was no significant reduction in stereopsis. Reduced stereopsis was not observed because the multifocal corneoscleral lens did not use the monovision technique. Therefore, a multifocal corneoscleral lens might be provide an alternative for presbyopic patients who have experienced reduced stereopsis when using a monovision technique with an SCL.
The usefulness and safety of multifocal SCLs for presbyopia correction have already been reported in various studies.However, this method has the disadvantage of exacerbating dry eye symptoms and corneal disease. In addition, lens fluctuation caused by dryness could affect astigmatism and VA[14-16].Corneal and handling problems induced by SCLs are important issues in healthy corneas. Several studies have reported that corneoscleral lenses can overcome the disadvantages of SCLs since they do not come in direct contact with the cornea[28].The present study also checked the risk of exacerbation of dry eye symptoms and corneal disease in healthy corneas before and after wearing multifocal corneoscleral lenses. The results showed no specific findings that would indicate that exacerbation developed after wearing the lenses. Therefore,it is believed that multifocal corneoscleral lenses could be a good alternative for presbyopia correction in patients who have difficulty wearing SCLs due to dry eyes or corneal disease.
The present study used spherical equivalent values to divide the patients into myopia, emmetropia and hyperopia groups and conducted surveys to determine each group’s satisfaction, discomfort, and willingness to continue to wear the corneoscleral lenses. The results showed that the patients in the myopia group had higher satisfaction scores for VA at far distances, VA at near distances, and ease of handling after wearing the corneoscleral lenses than did the patients in the emmetropia and hyperopia groups. The three groups showed similar scores for the discomfort survey. Moreover, the patients in the myopia group showed significantly greater willingness to continue to wear the corneoscleral lenses than the patients in the emmetropia and hyperopia groups did. These differences may have occurred because patients with myopia are more receptive to wearing lenses due to their experience of having worn spectacles for a long time, unlike patients with emmetropia and hyperopia. The fact that high satisfaction can be achieved by prescribing corneoscleral lenses to patients with presbyopia who already had myopia should be considered when prescribing corneoscleral lenses to patients with presbyopia.
This study had the following limitations. First, the sample size was insufficient to allow comparisons among the three groups (myopia, emmetropia and hyperopia), and the 4-week follow-up period was not enough to evaluate the safety of the corneoscleral lens. Second, this investigation did not include a control group, such as a multifocal SCL group, to compare with the multifocal corneoscleral lens group. Therefore, we believe that additional long-term studies are needed. Third, pupil size could affect visual performance. In addition, refractive error is associated with pupil size as age and luminance[29-31].Therefore, when we choose a lens design and add power, we should consider each participant’s pupil size pupil size. In our study, we could not consider this aspect. However, the present study was valuable in that it prospectively analyzed the presbyopia correction effect of multifocal corneoscleral lenses to verify their usefulness and safety.
In conclusion, the Onefit™ A multifocal corneoscleral lens could be an excellent option for presbyopia correction since wearing such lenses does not cause serious ophthalmic complications.
ACKNOWLEDGEMENTS
Foundation:Supported by the Dong-A University Research Fund.
Conflicts of Interest: Park WC, None;Kim CH, None;Jin SW, None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
