Trabeculectomy with Ologen implant versus perfluoropropane gas bubble for open angle glaucoma in pseudophakic eyes
Ahmed S Elwehidy, Tharwat Mokbel, Hossam Youssef Abouelkheir, Waleed Abou Samra,Faried M Wagdy, Amr Mohammed Elsayed Abdelkader
1Department of Ophthalmology, Mansoura Ophthalmic Center,Faculty of Medicine, Mansoura University, Mansoura 35516,Egypt
2Department of Ophthalmology, Faculty of Medicine, Menofia University, Shebin El Kom 32512, Egypt
Abstract
● KEYWORDS: pseudophakic glaucoma; trabeculectomy with Ologen; trabeculectomy with perfluoropropane; Ologen;perfluoropropane
INTRODUCTION
Trabeculectomy with mitomycin C (MMC) demonstrated greater risk of failure among pseudophakic eyes with open angle glaucoma (OAG) compared to phakic ones in traditional studies[1-3]. This is explained by the higher concentration of the aqueous humor inflammatory cytokines after phacoemulsification. Such cytokines activate subconjunctival fibroblast proliferation and promote more ocular inflammation[4]. Thus, the risk of more bleb scarring and failure in such eyes is higher than the phakic status even with the use of antimetabolites[5]. Furthermore, such antimetabolites as MMC increase the hazards of more postoperative blebrelated complications, hypotony, choroidal detachment, and even endophthalmitis[6]. OlogenTM(Aeon Astron Europe B.V.,The Netherlands) is biodegradable collagen matrix implant and a wound-healing modulator. It had been introduced to reduce the risks of antimetabolites[7-9]. The ologen implant is traditionally placed over the scleral flap during glaucoma surgery. It optimizes wound healing and acts as a reservoir for bleb formation. It guides fibroblast migration patterns,down grades extracellular matrix deposition and minimizes fibrosis[6-7,10]. OlogenTMsaves the conjunctival bleb during the early postoperative period by acting as a mechanical barrier between the inner conjunctival and the outer episcleral surfaces as early contact between them induces excessive fibrosis and leads to flat and nonfunctional blebs[11].
Perfluoropropane (C3F8) is an inert, expanding gas, used in vitreoretinal surgery to tamponade retinal breaks. It can expand and last for several weeks after intravitreal injection. A longlasting non expansible concentration of C3F8 is created by mixing 14% C3F8 and 86% air. Injection of this bubble into the subconjunctival space during glaucoma operation provides a transient “spacer effect” between the inner conjunctival and the outer episcleral surfaces that lasts up to four weeks,covering the period of maximum postoperative inflammation.The spacing effect is expected to reduce fibrosis, maintain bleb formation and increase the success rate[12-13].The current study aimed to evaluate the efficacy and safety of these two methods of augmented trabeculectomy: Ologen implant versus C3F8 gas bubble in eyes with medically uncontrolled pseudophakic OAGs.
SUBJECTS AND METHODS
Ethical ApprovalThis was a comparative randomized study, included 57 pseudophakic eyes of 57 patients with medically uncontrolled OAG, presenting at Mansoura University Ophthalmic Center (a tertiary referral center,Egypt) between April 2013 and March 2020. This study was accepted by the Ophthalmology Department Local Ethics and Research Committee, obtained Mansoura faculty of medicine Institutional Research Board (IRB) approval (Code:R.20.08.1001.R1) and matches the requirements of the Declaration of Helsinki. All participants received a detailed description of the study design and the surgical techniques, and provided written informed consent. The study included merely eyes with previous phacoemulsification and posterior chamber intraocular lens (PCIOL) and had an intraocular tension (IOP)above 21 mm Hg inspite of the maximally tolerated antiglaucoma drugs. Eyes with closed angles or with previous intraocular surgery other than phacoemulsification were excluded.
Preoperative EvaluationAll of the patients underwent a thorough ophthalmological examination, particularly estimation of the best corrected visual acuity (BCVA), slitlamp examination, IOP by Goldmann’s applanation tonometry,gonioscopy for angle grading using Schaffer’s grading system and dilated fundus examination. Visual field (VF) assessment was performed by SITA strategy perimetry (Humphrey, central 24-2 standard strategy). Optic nerve head was evaluated using a spectral domain optical coherence tomography (OCT;Topcon, Japan). The number of antiglaucoma medications was recorded.
Selected patients were randomized using “random computergenerated numbers” to undergo trabeculectomy with Ologen implant (group I: 29 eyes) or trabeculectomy with C3F8 gas bubble (group II: 28 eyes). All patients were scheduled for surgery and operated upon by a single surgeon (Elwehidy AS).
Surgical Procedures
Trabeculectomy with OlogenAfter fashioning a fornix based conjunctival flap, a quadrilateral (4×3 mm2) scleral flap was fashioned. Slow anterior chamber decompression was done through paracentesis. Kelly punch was used to excise a block(2×1 mm2) of trabecular meshwork followed by doing basal iridectomy. The corners of the scleral flap were fixated to the underlying sclera using minimal tension 10/0 nylon sutures that allow both filtration on minimal pressure and maintaining formed anterior chamber (AC) at the end of surgery.
A rectangular Ologen implant about 6 mm ×2 mm was placed over the scleral flap between the sclera and Tenon’s capsule.Lastly, the conjunctiva flap was repositioned using water-tight 10/0 nylon sutures.
Trabeculectomy with perfluoropropane gas bubbleGlaucoma surgery was done by conventional trabeculectomy with limbal based conjunctival flap as described by Takihara et al[14]with some modification in conjunctival closure. The conjunctival flap was tightened by continuous suturing in two separate layers. The Tenon’s capsule was sealed by 8/0 vicryl suture, while the conjunctiva was secured with 8/0 virgin silk suture. The C3F8 gas bubble was obtained from the gas container (Alcon, USA) using a compatible filter into a 1 mL insulin syringe. The non expansible concentration of C3F8 was prepared by making a mixture of 0.15 mL of C3F8 with 0.85 mL of filtered air.
Totally, 0.2 to 1 mL of such C3F8 non expansible concentration was injected as a single bubble into the subconjunctival space to cover the entire scleral flap using the injection system formed of 5 cm long silicone tube attached to 27-gauge cannula connected to 1 mL insulin syringe. The silicone tube was inserted into the subconjunctival space before securing the suture knots. The sutures were directly tightened upon removal of the silicone tube, holding the gas bubble in the subconjunctival space. The repaired incision was tested for leakage using fluorescein dye.
Postoperative TreatmentEyes were treated with topical steroids (dexamethasone acetate) and antibiotic (ofloxacin)eye drops five times daily with gradual taper over a 5wk period.Cyclopentolate eye drops were used 3 times daily for the first postoperative week and then discontinued. Topical anti-glaucoma medications (beta-blockers and/or carbonic anhydrase inhibitors) were prescribed in some patients only whenever needed.
Postoperative Follow-upThe follow up schedule was first postoperative day, after 1wk, at 1, 3, 6, 12, 18, 24, 30 and 36mo postoperative intervals. All of the patients underwent a thorough ophthalmological examination, including: assessment of the BCVA, IOP by Goldmann’s applanation tonometry and slit-lamp examination to evaluate bleb morphology and to detect postoperative complications. The clinical bleb morphology evaluation was based on the Moorfields’ bleb grading system with special reference to the bleb elevation, the degree of inflammation of the conjunctiva overlying the bleb and gas bubble features including the size (in mm), number and position (in or out of position).Visual field assessment was performed by SITA strategy perimetry (Humphrey, central 24-2 standard strategy) and optic nerve head was evaluated using a spectral domain OCT (Topcon, Japan) at 1y postoperative interval. Also, the number of antiglaucoma medications and their reduction percentage were noted.At the meantime, the surgical success rate was evaluated. IOP between 6 and 18 mm Hg together with ≥35% reduction of preoperative IOP without any antiglaucoma medications or supplementary glaucoma surgery during the entire follow-up period was considered as a complete success, while qualified success was defined as an IOP between 6 and 18 mm Hg together with ≥35% reduction of the preoperative IOP with the help of topical antiglaucoma medications without further glaucoma surgery. Surgical failure was defined as an IOP≥19 mm Hg in spite of the maximal use of antiglaucoma medication, or when an additional procedure such as needling or repeated trabeculectomy was needed to control the IOP.Surgical failure was also considered if there was loss of light perception or development of postoperative hypotony for ≥6wk with hypotony maculopathy. Postoperative hypotony was identified with IOP ≤5 mm Hg for >1wk after trabeculectomy.

Table 1 Demographic and preoperative data mean±SD, range, median
Statistical AnalysisData were collected, computed then evaluated by statistical package for social science (IBM SPSS)version 24 for windows. Validation of the data for normality was done using Shapiro-Wilk’s test. Descriptive statistics were calculated in the form of mean±SD, range and median.Wilcoxon and Chi-square tests were used to compare the preoperative and postoperative variables in each group. The comparison between the two groups was done using Mann-Whitney test for non Gaussian numerical and ordinal variables while Chi-square or fisher’s exact test for nominal variables.Kaplan-Meier survival analysis estimated the mean success time and probabilities of success in the both groups. P value of less than 0.05 was considered significant.
RESULTS
Fifty-seven eyes of 57 patients with uncontrolled open-angle pseudophakic glaucoma were recruited in this study. Cases were randomly categorized into two groups; 29 patients were allocated in group I (trabeculectomy with Ologen) while 28 patients were assigned in group II (trabeculectomy with C3F8 gas bubble). All patients had completed at least 36mo followup. Table 1 demonstrates the demographic and preoperative data of the patients in both groups. There was no statistically significant difference between both groups in all parameters.
The IOP was significantly reduced in both study groups at all postoperative follow up intervals 1wk, 3, 6, 12, 18, 24, 30 and 36mo, P<0.001. The final IOP percentage reduction even after 36mo was 57.58% in group I compared to 52.84% in group II.Pre- and postoperative IOP values were demonstrated in Table 2.The number of preoperative anti-glaucoma medications was considerably reduced after 36mo of follow up from 3.24±0.4 to 0.48±0.98 in group I and from 3.18±0.4, to 0.60±1.1 in group II, P<0.0001. Similarly the preoperative VF mean deviation(MD) and preoperative VF pattern standard deviation (PSD)reported statistically significant improvement in both groups.However, there was no statistically significant difference between the other pre- and postoperative variables among both groups. Data were demonstrated in Table 3.
Although IOP and most of the other criteria did achieved statistically significant improvement in each of the study groups separately, however, the results were initially comparable in between the two groups. IOP reduction difference remained statistically insignificance up to 12mo offollow up. However, group I achieved a statistically significant reduction over group II during the last 24mo of follow up. Data were shown in Table 2. Both groups had a more or less similar effect on other tested parameters (antiglaucoma medication,C/D ratio, BCVA, RNFL thickness, VF MD and VF PSD) after 36mo follow up. Data was demonstrated in Table 3.
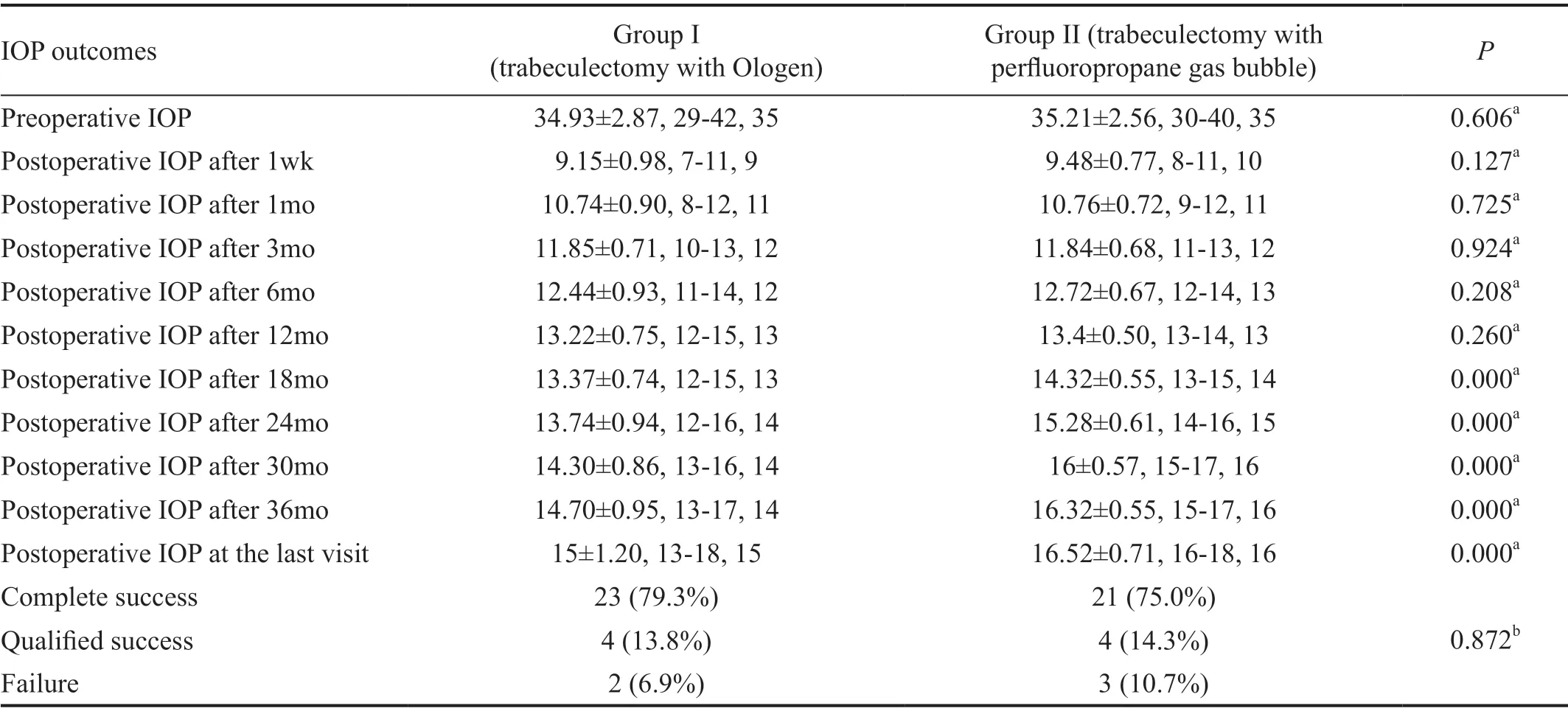
Table 2 Comparison of IOP outcomes between the two groups at different follow up time points and success rate mean±SD, range, median; mm Hg
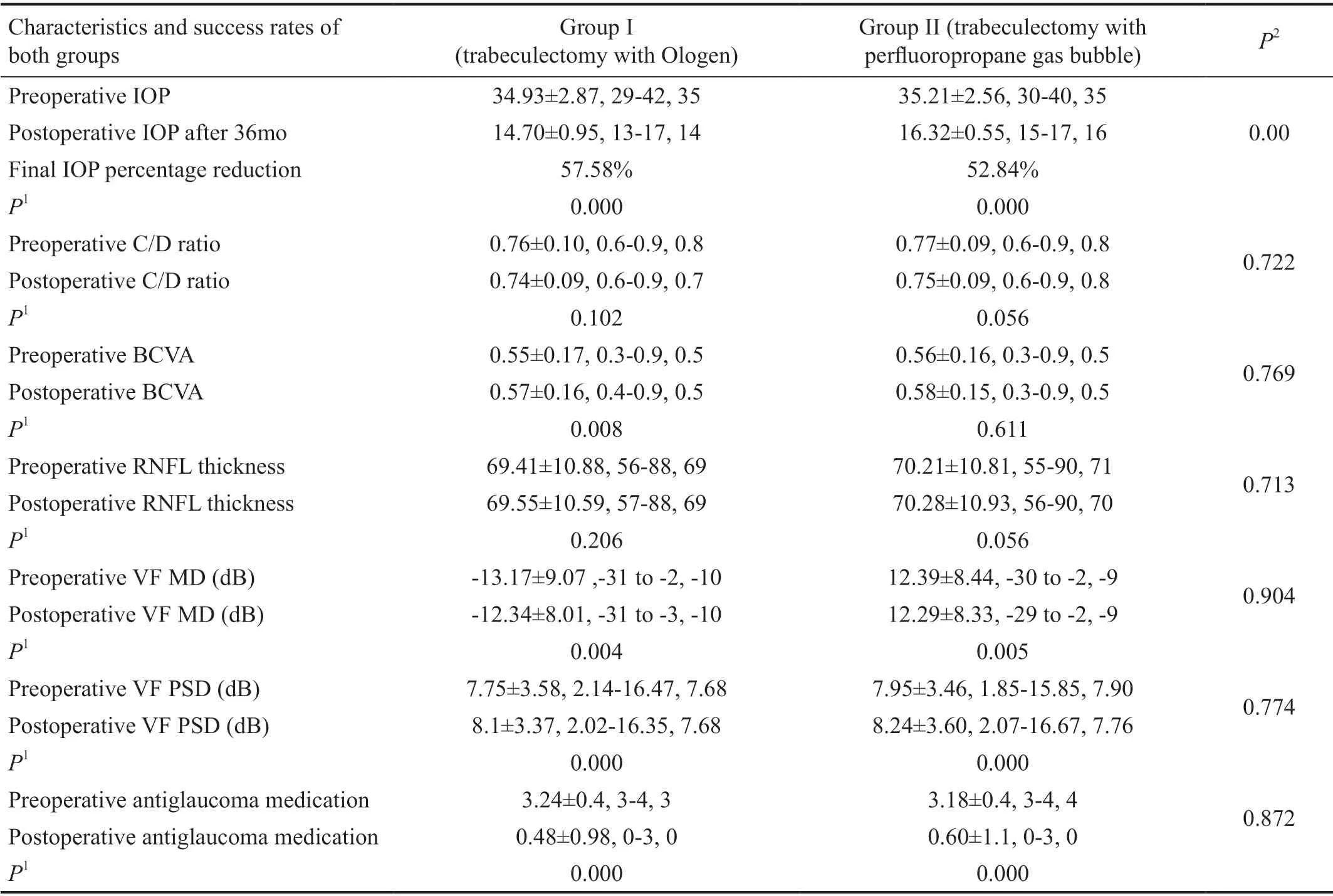
Table 3 Pre- versus postoperative characteristics and success rates of both groups mean±SD, range, median
In group I, complete success was obtained in 23 cases (79.3%)and qualified success in 4 cases (13.8%) while failure was noted in 2 cases (6.9%) by the end of 36mo of follow up.similarly in group II complete success was obtained in 21 cases(75.0%) and qualified success in 4 cases (14.3%) while failure was noted in 3 cases (10.7%) by the end of 36mo. Data were shown in Table 2.
Kaplan-Meier survival analysis curve for the probability of postoperative success rate in both groups was shown in Figure 1. The mean survival time was 35.37±0.448mo in group I and 34.28±0.95mo in group II with an insignificant difference between them (P value 0.588).
Bleb morphology at 36mo postoperatively according to the Moorfield’s bleb-grading system was demonstrated in Table 4 and showed no statistically significant difference between both groups. C3F8 gas bubble remained as a single bubble till the end in 22 cases, while in 6 cases, bubble fragmented into small bubbles. Twenty-five bubbles remained in position over the scleral flap till the end while only 3 bubbles moved out of their place. The C3F8 bubbles in the blebs remained for 14.6±2.99d(range, 10-24d; median, 14d) until the complete resolution. All filtering blebs remained mildly to markedly elevated during the existence of the bubble. No evidence of severe conjunctivitis was observed over the gas bubbles.
Encapsulated bleb was the most frequently encountered postoperative complication in both groups. Bleb revision was needed in 5 eyes, 2 in group I and 3 in group II. However,Ahmed glaucoma valves (AGV; FP-7) were implanted in 3 eyes (one in group I while 2 in the group II) after failure of bleb revision. Other temporary postoperative complications as transient hypotony, shallow AC, subtle choroidal detachment and minor IOP spikes were conservatively managed till complete resolution. No sight-threatening complications were reported during the period of follow-up in both groups.Statistical analysis reported no significant difference in between both groups. Complications were demonstrated in Table 5.
DISCUSSION
This study aimed to evaluate the efficacy and safety of using two different adjuvants with augmented trabeculectomy;Ologen implant versus C3F8 gas bubble in pseudophakic eyes with medically-uncontrolled OAG. The study evaluated the role of subconjunctival non expansible C3F8 gas bubbles,via a “spacer” effect, in augmented trabeculectomy at greater risk of failure[12-13]and comparing its effect with the wellestablished efficacy of Ologen as an adjuvant treatment with trabeculectomy in different studies[6-7,15]. The current study revealed that both groups were effective in reducing IOP and this effect was maintained throughout the entire postoperative follow up period. IOP levels of both groups were initially comparable. However, the group I did achieved slightly more reduction over the group II at the end of follow up period.The authors hypothesize a reason for this. Ologen implants maintain the potential subconjunctival space mechanically keeping the filtration in a controlled fashion. This effect guards against overfilteration and hypotony together with reducing adhesions between the episcleral surface and the conjunctiva at the mean time. Ologen implants allow for a diffusely functioning bleb and this mechanical effect remains until implant’s degradation, which may last for up to 6-9mo[16].
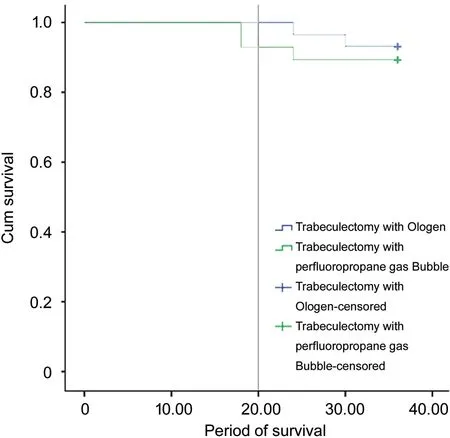
Figure 1 Kaplan-Meier survival analysis curve for the probability of postoperative success rate.
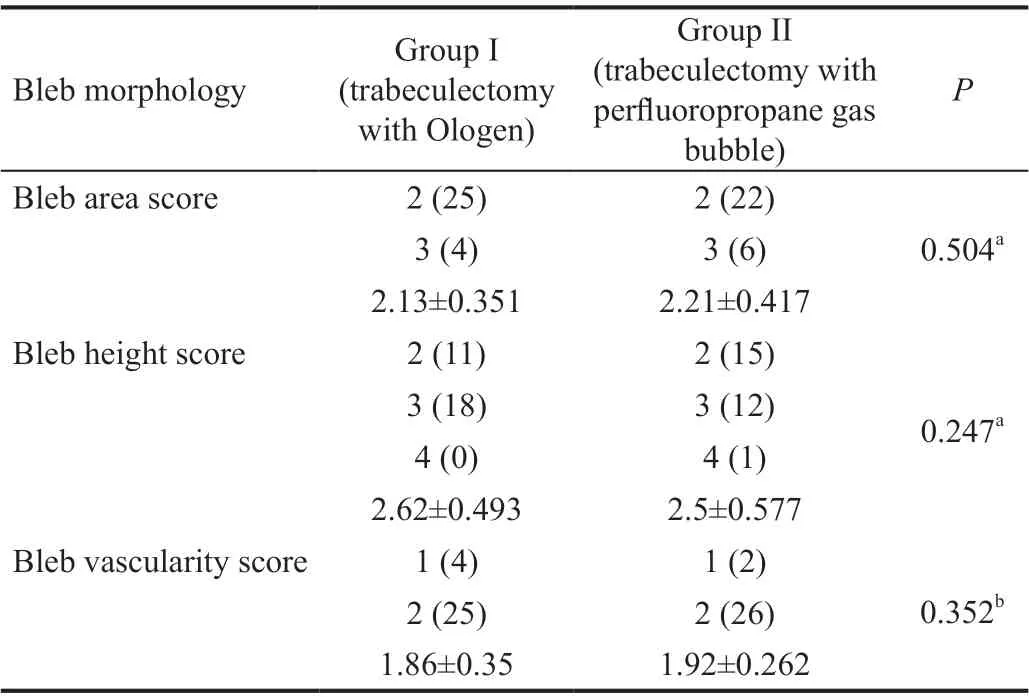
Table 4 Bleb morphology at 36th month postoperatively according to the Moorfield’s bleb-grading system Grade (n)

Table 5 Postoperative complications n (%)
The IOP reductions in group I of the current study were 64.4% and 62.15% at 6mo and 12mo after trabeculectomy with ologen implant. These IOP reductions were greater than that reported with other surgical procedures[14,17]. Takihara et al[14], studied the efficacy of trabeculectomy with MMC in 25 eyes with pseudophakic OAG with IOP reductions of 59.8% and 58.4% at 6 and 12 postoperative months. Another study compared the 3-year outcome of AGV versus Ex-Press miniature glaucoma shunt in 92 eyes with pseudophakic OAG.The IOP reductions at 12, 24 and 36mo postoperatively were 56.9%, 55.6% and 53.2% in the AGV group and 49.4%, 42.1%and 43.1% in the Ex-Press group[17].
Similarly, the IOP reductions in group II of the present study were 63.87%, 61.94% and 59.3% at 6, 12 and 18mo after C3F8 gas bubble augmented trabeculectomy. These reductions in IOP were greater than that reported by Lu et al[12]who evaluated the effect of subconjunctival retention of C3F8 gas on trabeculectomy in 16 eyes of 16 patients under 35 years old with OAG. They reported IOP reductions of 50.2%, 44% and 41.3% at 6, 12 and 18 postoperative months[12]. Also in group II of the current study, the IOP reduction at 18thpostoperative month (59.3%) was greater than that reported by Wong and Seah[13]who studied the use of C3F8 gas bubble in augmented trabeculectomy in 20 patients with medically uncontrolled glaucoma. They reported an IOP reduction of 46.9% after 16mo of follow-up.
The IOP-lowering medications in the current study were reduced from mean baseline values of 3.24 and 3.18 to mean values of 0.48 and 0.6 medications respectively in both groups at the end of the 36thpostoperative month. These reductions were of great statistical significance (P<0.001). Likewise,comparing the mean preoperative and the mean eventual postoperative VF MD and PSD, there were statistically significant improvements in both groups at the end of the follow up period. However, the mean values of the BCVA, C/D ratio and RNFL thickness achieved some improvements from the baseline in both groups but these improvements were not statistically significant during 36mo of follow up.
This was consistent with the growing evidence of slight reversal of structural glaucomatous damage after controlling the IOP[18]. Some studies reported improvements in structural measurements following effective reduction in IOP with glaucoma surgery as a reversal in disc cupping or significant decreases in cup depth as well as increase in RNFL thickness measurements[19-21]. Additionally, the improvement of ocular surface health following the reduction of IOP-lowering medication use together with the successful surgical IOP control may contribute to improvement of BCVA.
The current study demonstrated no significant difference between the 2 groups regarding anti-glaucoma medications,VF changes (MD and PSD), C/D ratio, RNFL thickness and BCVA at the end of the follow up period.
In spite of the relatively rigid criteria of success of the present study, the overall outcome of groups I and II was very encouraging with a total success of 93.1% and 89.3% respectively.
In the current study, bleb morphology at 36mo postoperatively according to the Moorfield’s bleb grading system showed no statistically significant difference between both groups. In group II, all the filtering blebs remained mildly to markedly elevated during the existence of C3F8 gas bubble with no evidence of severe conjunctivitis observed over the gas bubbles. The C3F8 gas bubbles in the blebs remained for 14.6±2.99d (range, 10-24d; median, 14d) till the complete absorption. Wong and Seah[13]reported that their gas bubbles remained in the conjunctival bleb for a mean duration of 17d with the range between 13-27d. They also noted the absence of excessive conjunctival inflammation overlying the gas bubble.Also microscopic inspection of their animal study tissues did not indicate any upregulation in the number of inflammatory cells[13].
In terms of complications, encapsulated bleb was the most frequently encountered postoperative complication encountered in the present study in both groups (6.9% in the group I versus 10.7% in the group II). Bleb revision was needed in 5 eyes, 2 in group I and 3 in group II. AGV (FP-7) were implanted after failure of bleb revision in 3 eyes (one in group I and 2 in group II). Temporary complications as transient hypotony, shallow AC, subtle choroidal detachment and minor IOP spikes were conservatively managed till complete resolution. No sightthreatening complications were reported during the period of follow-up in both groups.
To the best of the authors’ data, this is the first study to report on these techniques in the surgical management of glaucoma in pseudophakia. However this study has its limitations as the relatively small number of studied eyes and the enrolment of only one type of challenging glaucoma (glaucoma in pseudophakia). This study methods should be applied in more high risk cases and on a larger number of eyes with different types of refractory glaucomas to assess their efficacy over primary trabeculectomy and antimetabolite-aided trabeculectomy.
In conclusion, both methods of augmentation of trabeculectomy with either Ologen implant or C3F8 gas bubble were associated with strict long term IOP control with evident safety in eyes with medically-uncontrolled OAG in pseudophakic eyes.Although both surgical procedures produced a remarkable IOP reductions over the entire three years of follow-up, however group I achieved a statistically significant reduction over the group II during the last 24mo of follow up. Bleb augmentation with C3F8 gas bubble was proved to decrease early postoperative adherence within the first two postoperative weeks when the risk of inflammation and bleb failure is at their maximum. Besides, its relative safety and simplicity as well as making a good use of materials and instruments readily accessible in most ophthalmic operating rooms.
ACKNOWLEDGEMENTS
Conflicts of Interest:Elwehidy AS,None;Mokbel T,None;Abouelkheir HY,None;Samra WA,None;Wagdy FM,None;Abdelkader AME,None.
 International Journal of Ophthalmology2021年4期
International Journal of Ophthalmology2021年4期
- International Journal of Ophthalmology的其它文章
- Prevalence and risk factors of dry eye disease in young and middle-aged office employee: a Xi’an Study
- YM155 inhibits retinal pigment epithelium cell survival through EGFR/MAPK signaling pathway
- Clinical features and treatment outcomes of intraocular lymphoma: a single-center experience in China
- Trends in research related to high myopia from 2010 to 2019: a bibliometric and knowledge mapping analysis
- A simple new technique for the induction of residual posterior vitreous cortex removal and membrane peeling
- Differential degeneration of rod/cone bipolar cells during retinal degeneration in Royal College of Surgeons rats
