ERCP结合腹腔镜胆囊切除术在老年胆囊结石合并胆总管结石患者中的运用
陈聪 安代红 陶锐


【摘要】 目的:探讨ERCP联合LC在老年胆囊结石合并胆总管结石的安全性和有效性。方法:回顾性分析2013年1月-2019年9月在本院同一次住院期间先后进行ERCP和LC的68例胆囊结石合并胆总管结石老年患者进行临床资料。根据年龄将患者分为高龄组(≥75岁)和老年组(≥65岁且<75岁),高龄组31例,老年组37例。比较两组并发症发生情况及手术指标。结果:两组均无死亡病例及30 d内再住院病例。高龄组一次性结石取尽率、LC手术时间、中转开腹率、出血量分别为93.5%、(56.32±19.35) min、0、10.00(5.00,10.00) mL均低于老年组的97.3%、(61.08±33.46) min、5.41%、12.89(10.00,10.00) mL,差异均无统计学意义(P>0.05)。高龄组ERCP手术时间、LC术后住院时间、ERCP和LC间隔时间分别为(44.58±14.43) min、(5.64±2.09) d、(3.74±1.71) d均长于老年组的(41.73±14.76) min、(5.14±1.75) d、(3.31±1.67) d,但差异均无统计学意义(P>0.05)。两组均无术后出血和穿孔发生。高龄组ERCP术后急性胰腺炎发生率为9.7%高于老年组的5.4%,高龄组LC术后肺部感染、呼吸机脱机延迟发生率均为0,均低于老年组的2.7%和5.4%,差异均无统计学意义(P>0.05)。結论:对于存在胆囊结石和胆总管结石的老年患者,在同一次住院期间内完成ERCP和LC是安全、可行的。
【关键词】 内镜逆行胰胆管造影术 腹腔镜胆囊切除术 胆囊结石 胆总管结石
Application of ERCP Combined with Laparoscopic Cholecystectomy in Elderly Patients with Cholecystolithiasis Complicated with Choledocholithiasis/CHEN Cong, AN Daihong, TAO Rui. //Medical Innovation of China, 2021, 18(28): 129-133
[Abstract] Objective: To investigate the safety and efficacy of ERCP combined with LC in elderly patients with cholecystolithiasis complicated with choledocholithiasis. Method: Clinical data of 68 elderly patients with cholecystolithiasis complicated with choledocholithiasis who underwent ERCP and LC successively during the same hospitalization period from January 2013 to September 2019 in our hospital were retrospectively analyzed. According to age, patients were divided into the old elderly group (≥75 years old) and the young elderly group (≥65 years old and <75 years old), with 31 cases in the old elderly group and 37 cases in the young elderly group. The incidence of complications and surgical indicators were compared between two groups. Result: There were no death or rehospitalization within 30 d in both groups. The one-time stone extraction rate, LC surgical time, conversion rate and blood loss in the old elderly group were 93.5%, (56.32±19.35) min, 0, 10.00 (5.00, 10.00) mL, respectively, which were lower than 97.3%, (61.08±33.46) min, 5.4%, 12.89 (10.00, 10.00) mL in the young elderly group, but the differences were not statistically significant (P>0.05). ERCP surgical time, postoperative hospital stay, ERCP and LC interval in the old elderly group were (44.58±14.43) min, (5.64±2.09) d, (3.74±1.71) d, respectively, which were longer than (41.73±14.76) min, (5.14±1.75) d, (3.31±1.67) d in the young elderly group, but the differences were not statistically significant (P>0.05). No postoperative bleeding and perforation occurred in both groups. The incidence of postoperative acute pancreatitis in the old elderly group was 9.7%, which was higher than 5.4% in the young elderly group, the incidence of postoperative pulmonary infection and ventilator offline delay after LC in the old elderly group were 0, which were lower than 2.7% and 5.4% in the young elderly group, the differences were not statistically significant (P>0.05). Conclusion: Combination of ERCP and LC is safe and feasible for the elder patients with cholecystolithiasis complicated with choledocholithiasis in same hospitalization.
[Key words] EPCP Laparoscopic cholecystectomy Cholecystolithiasis Choledocholithiasis
First-author’s address: Bishan Hospital, Chongqing 402760, China
doi:10.3969/j.issn.1674-4985.2021.28.032
胆囊结石是我国常见的胆道疾病之一,且发病率随着年龄的增加逐渐增高。约30%大于70岁的老年人存在胆囊结石,其中10%~20%的胆囊结石又常常合并胆总管结石[1]。胆总管结石一旦确诊,均建议积极手术,避免因结石梗阻而出现重症胆管炎、感染性休克等情况[2]。由于老年人身体机能随着年龄的增加逐渐减退,且易合并基础疾病,在选择手术策略时,有效性、安全性和微创性就十分重要。本文回顾性分析了本院运用内镜逆行胰胆管造影术(endoscopic retrograde cholangiopancreatography,ERCP)联合腹腔镜胆囊切除术(laparoscopic cholecystectomy,LC)治疗老年胆总管和胆囊结石的安全性和有效性,现报道如下。
1 资料与方法
1.1 一般资料 回顾性分析2013年1月-2019年9月本院在同一次住院期間先后进行ERCP和LC的68例胆囊结石合并胆总管结石老年患者的临床资料。纳入标准:(1)在同一次住院期间先后进行ERCP和LC;(2)年龄≥65岁。排除标准:(1)ERCP取石失败;(2)既往有上腹部手术和消化道重建史;(3)肝内胆管结石;(4)严重心肺等功能障碍不能耐受手术。根据年龄将患者分为高龄组(≥75岁)和老年组(≥65岁且<75岁),高龄组31例,老年组37例。本研究经医院伦理委员会批准。
1.2 方法
1.2.1 术前准备 两组患者入院后积极完善各项术前常规检查,如血常规、肝功、肾功、电解质、凝血功能、血糖、心电图、胸片、心脏彩超、腹部彩超、MRCP或CT等。对高血压、糖尿病患者保持血压、血糖平稳;术前签署手术知情同意书。所有患者术前常规禁食水6~8 h,术前30 min静脉注射山莨菪碱20 mg,口服达克罗宁胶浆。采取哌替啶50 mg+地西泮10 mg镇静或者丙泊酚静脉麻醉。
1.2.2 操作方法 患者先行ERCP手术。患者均采取左侧俯卧位,十二指肠镜到达十二指肠降段,观察乳头形态,插管成功后注入泛影葡胺进行胆道造影,明确胆总管结石的大小、数量以及位置。根据结石大小选择十二指肠乳头切开大小以及是否进行球囊扩张及机械碎石。术中造影提示无结石残留后,放置鼻胆管引流或胆道支架引流。术后禁食禁水,常规进行补液支持治疗。对于存在胆道感染的患者使用抗生素。术后3 h检查血淀粉酶,第2天复查血常规、肝功血淀粉酶及电解质。术后根据患者有无胰腺炎、出血、穿孔以及患者一般情况,择期安排LC。LC均采取三孔法,分离出胆囊管和胆囊动脉,用可吸收生物夹结扎后切断,若胆囊三角无法解剖则中转开腹。
1.3 观察指标 (1)比较两组手术过程指标。ECRP手术包括手术时间、一次性结石取尽率。LC手术包括手术时间、中转开腹率、出血量、术后住院时间、ERCP和LC手术间隔时间。(2)比较两组术后并发症发生情况。ERCP术后并发症包括急性胰腺炎、出血、穿孔,LC手术包括肺部感染、呼吸机脱机延迟(气管插管拔除时间超过术后2 h)。
1.4 统计学处理 采用SPSS 20.0软件对所得数据进行统计分析,正态分布计量资料以(x±s)表示,比较采用t检验;非正态分布计量资料用M(P25,P75)表示,比较采用Mann-Whitney U检验;计数资料以率(%)表示,比较采用字2检验。以P<0.05为差异有统计学意义。
2 结果
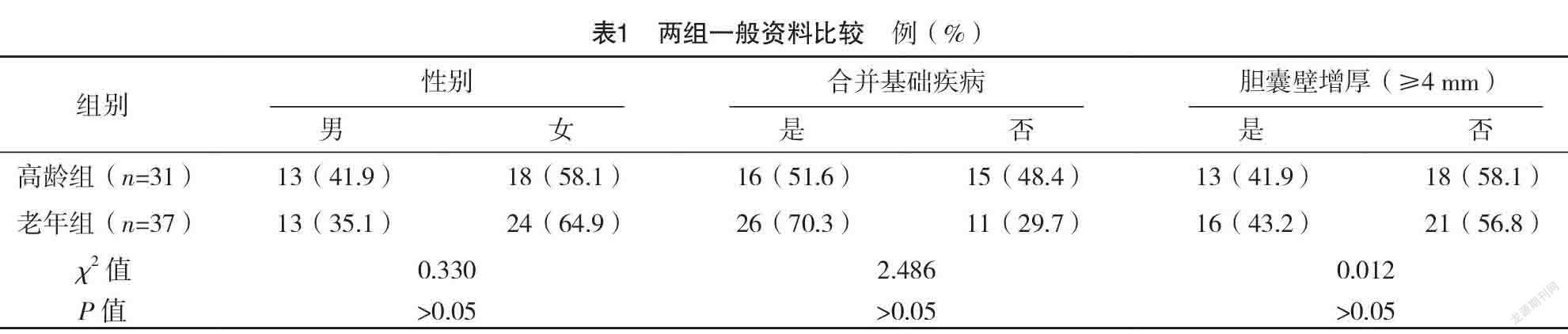
2.1 两组一般资料比较 高龄组16例患者存在基础疾病(高血压10例,糖尿病4例,心脏病4例,肺气肿4例,肾功能异常3例,脑梗死1例),老年组中有26例存在基础疾病(高血压12例,糖尿病6例,心脏病1例,慢性阻塞性肺病4例,肾功能异常2例,脑梗死1例)。两组一般资料比较,差异均无统计学意义(P>0.05),具有可比性。见表1。
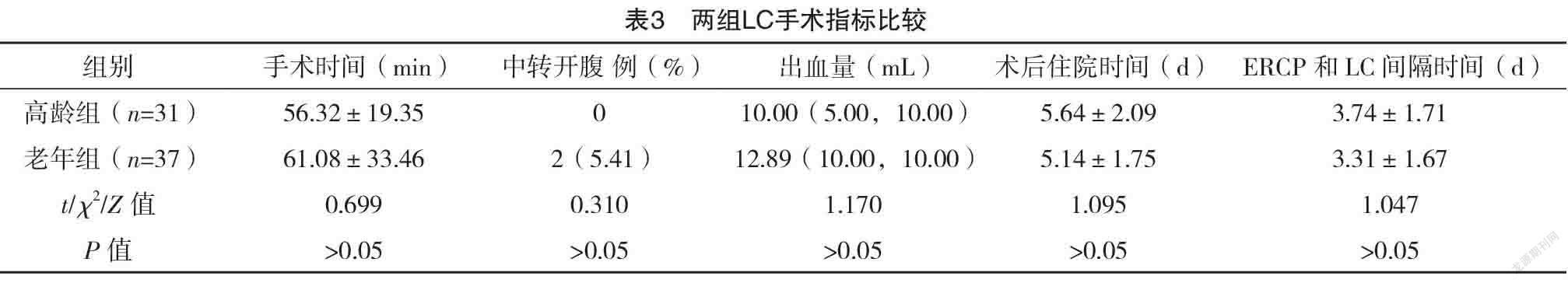
2.2 两组手术指标比较 两组ERCP手术时间、一次性结石取尽率比较,差异均无统计学意义(P>0.05),见表2。所有的残余结石均通过再次的ERCP手术取出。两组的LC手术时间、中转开腹率、出血量、术后住院时间、ERCP和LC间隔时间比较,差异均无统计学意义(P>0.05)。见表3。
2.3 两组术后并发症情况比较 两组均无术后出血和穿孔发生。两组ERCP术后急性胰腺炎、LC术后肺部感染、呼吸机脱机延迟发生率比较,差异均无统计学意义(P>0.05),见表4。
3 讨论
随着社会人口结构的变化,老年人群体的比重逐渐增加。老年人身体机能随着年龄的增加而逐渐减退,且易合并一种或者多种疾病,如心脏病、糖尿病、高血压、慢性阻塞性肺病等,导致对手术耐受能力降低,尤其是创伤大,时间长的手术。因此,对于老年人来说,选择创伤小、术后恢复快、麻醉时间短的手术方式尤为重要。ERCP结合内镜下oddi括约肌切开(endoscopic sphincterotomy,EST)、内镜下十二指肠乳头气囊扩张(endoscopic papillary balloon dilation,EPBD)/内镜下乳头括约肌大球囊扩张术(endoscopic papillary large balloon dilation,EPLBD)等技术已经广泛运用于胆总管结石的治疗,具有安全性高、创伤小、术后恢复快等优点,尤其适用于老年人。尽管ERCP技术已十分成熟,但仍会出现一些并发症,如胰腺炎、出血、穿孔、胆管炎等[3]。此外,EST和球囊扩张对Oddi括约肌功能的破坏会引起术后反流性胆管炎的发生,甚至结石复发等远期并发症[4]。开腹胆囊切除+胆总管切开探查取石已广泛运用于临床治疗胆总管结石合并胆囊结石,但存在手术切口大、术后恢复慢等缺点,且术后需行T管引流[5]。腹腔镜胆囊切除+胆道探查较开腹手术创伤小,但需要熟练的腹腔镜技术,且面临术后T管引流的问题[6-7]。胆道探查术后留置T管的目的在于降低胆道内压力,促进胆总管下段或Oddi括约肌水肿消退和对胆道起支撑作用,避免胆道狭窄。此外,术后还可以通过T管窦道行胆道镜检查,避免结石残留[8]。但是长时间的T管引流不但可导致胆汁大量丢失,还为患者带来生活和行动上的不便,降低生活质量。杨彦等[9]进行的一项腹腔镜胆总管探查术后一期缝合的多中心研究表明,在严格掌握手术适应证的条件下行一期缝合是安全有效的,但该研究也指出,胆总管探查后术后一期缝合不但要求术者具有娴熟的腹腔镜下胆总管缝合技巧以避免术后胆瘘,还有严格的手术指征,如胆总管结石数目≤5枚、胆总管结石直径≤1.5 cm、无缩窄性乳头炎、无急性胆源性胰腺炎等。
LC具有創伤小、术后恢复快、术后并发症低等特点,已成为手术治疗胆囊结石的金标准。ERCP结合十二指肠乳头切开、球囊扩张等方式,已成为治疗胆总管结石的主要方式之一。ERCP取石联合LC与腹腔镜下胆囊切除+胆道探查取石手术在结石清除率、并发症发生率、病死率等方面没有显著差异,已逐渐成为治疗胆总管结石合并胆囊结石的主要方法之一,并且被日本胃肠病学会2016版指南所推荐[10-11]。但是,ERCP术后何时进行LC,目前国内外尚无明确的定义。有研究表明ERCP术后择期LC的患者发生胆绞痛、急性胆囊炎、胆源性胰腺炎、继发性胆总管结石的概率明显升高[12]。因此,ERCP术后应早期进行LC[13-15]。但是对年龄大,存在基础疾病的患者来说,既要考虑同一次住院期间完成ERCP和LC两次手术,又要考虑患者能否耐受短期内进行两次手术。本研究中,70.3%的老年人和51.6%高龄患者存在至少一种基础疾病,但两组术后均无死亡病例和30 d再住院患者。术后并发症方面,老年组中有2例患者LC术后出现呼吸机脱机延迟以及1例患者发生肺部感染。因此,对于老年人来说,术前详细评估患者病情,控制好血压、血糖、肺部感染等基础疾病,ERCP术后及时进行LC是安全的。
腹腔镜胆囊切除已成为治疗胆囊结石的首选方式。但是,腹腔镜胆囊切除术的中转开腹率在3.6%~8%[16]。腹腔镜中转开腹与多种因素有关,如:男性、年龄大于60岁、糖尿病、心血管疾病、上腹部手术史、急性胆囊炎、胆囊壁增厚、胆囊颈部结石嵌顿等,其中急性胆囊炎和胆囊壁增厚是导致腹腔镜胆囊切除术中转开腹的重要独立因素[17]。与单纯的LC相比,ERCP术后进行腹腔镜胆囊切除术的风险和难度会有所增加,这与胆囊炎所致的胆囊三角区组织水肿、解剖结构不清有关,随着时间的延长,组织水肿继续加重甚至纤维化形成。此外,ERCP的相关操作,如插管、乳头切口、球囊扩张、反复取石、造影剂、肠道细菌移位均可能会导致胆管周围炎,进一步增加手术难度[18-19]。对于合并胆总管结石的患者,入院后通常需完善CT、MRCP等相关检查,若合并急性胰腺炎、胆管炎,还需抗感染、控制胰腺炎等治疗,导致发病到LC手术的间隔时间明显延长,进一步增加了手术风险和难度。本研究中,41.9%的高龄组患者和43.2%的老年组患者存在胆囊壁增厚(≥4 mm),但是两组手术时间、出血量比较,差异均无统计学意义(P>0.05),仅有两例老年组患者发生中转开腹。因此,对于合并胆囊壁增厚的老年人,在同一次住院期间完成ERCP和LC,是可行、安全的。
ERCP术后急性胰腺炎(post-ERCP pancreatitis, PEP)是常见的并发症之一,发生率约9.7%,但是在高危人群中可达14.7%[3]。在本研究中,共5例患者发生了PEP,发生率为7.3%,所有患者均通过保守治疗后好转,无患者进展为重症胰腺炎。ERCP术后胰腺炎的发病机制尚不清楚,但是oddi括约肌功能障碍、女性、反复插管、预切开、胰管造影等都是诱发胰腺炎的高危因素,目前推荐预防PEP的方式主要有:术前肛门予以非甾体类药物(吲哚美辛或双氯芬酸)和术中胰管支架置入两种方式[20-21]。对于存在非甾体类药物禁忌证或预防性置入胰管失败的高危患者,可考虑舌下含化硝酸甘油或静脉使用生长抑素的方式预防PEP[22]。
本研究结果表明,对于存在胆囊结石和胆总管结石的老年患者,经过详细的术前评估和准备,在同一次住院期间完成ERCP和LC手术是安全可行的。
参考文献
[1] Kuan L L,Oyebola T,Mavilakandy A,et al.Retrospective Analysis of Outcomes Following Percutaneous Cholecystostomy for Acute Cholecystitis[J].World J Surg,2020,44(8):2557-2561.
[2] Sarli L,Costi R,Gobbi S,et al.Asymptomatic bile duct stones:selection criteria for intravenous cholangiography and/or endoscopic retrograde cholangiography prior to laparoscopic cholecystectomy[J].Eur J Gastroenterol Hepatol,2000,12(11):1175-1180.
[3]李鹏,王拥军,王文海.中国ERCP指南(2018版)[J].中华内科杂志,2018,57(11):772-801.
[4]孔雷,吴庆华,陆一凡,等.内镜下十二指肠乳头气囊扩张治疗胆总管结石对Oddi括约肌功能的影响[J].肝胆胰外科杂志,2019,31(5):301-305.
[5] Girard R M,Morin M.Open cholecystectomy:its morbidity and mortality as a reference standard[J].Can J Surg,1993,36(1):75-80.
[6] Petelin J B.Surgical management of common bile duct stone[J].Gastrointest Endosc,2002,56(6 Suppl):S183-S189.
[7] Muhammedoglu B,Kale I T.Comparison of the safety and efficacy of single-stage endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy versus two-stage ERCP followed by laparoscopic cholecystectomy six-to-eight weeks later:A randomized controlled trial[J].Int J Surg,2020,76:37-44.
[8]蔡军,龔仁华,孙登群,等.三镜联合胆总管探查一期缝合临床分析[J].中国内镜杂志,2015,21(3):308-310.
[9]杨彦,张剑,楼健颖,等.腹腔镜胆总管探查取石免留置鼻胆管引流一期缝合术临床疗效的多中心回顾性研究(附312例报告)[J].中华消化外科杂志,2018,17(1):68-75.
[10] Yang J J,Liu X C,Chen X Q,et al.Clinical value of DPOC for detecting and removing residual common bile duct stones (video)[J].Bmc Gastroenterol,2019,19(1):135.
[11] Ansaloni L,Pisano M, Coccolini F,et al.2016 WSES guidelines on acute calculous cholecystitis[J].World J Emerg Surg,2016,11:25.
[12] Lau J Y,Leow C K,Fung T M,et al.Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in Chinese patients[J].Gastroenterology,2006,130(1):96-103.
[13] Aziret M,Karaman K,Ercan M,et al.Early laparoscopic cholecystectomy is associated with less risk of complications after the removal of common bile duct stones by endoscopic retrograde cholangiopancreatography[J].Turk J Gastroenterol,2019,30(4):336-344.
[14] Trejo-Avila M,Solorzano-Vicuna D,Garcia-Corral R,et al.
Laparoscopic cholecystectomy after endoscopic treatment of choledocholithiasis:a retrospective comparative study[J].Updates Surg,2019,71(4):669-675.
[15] Passi M,Inamdar S,Hersch D,et al.Inpatient Choledocholithiasis Requiring ERCP and Cholecystectomy:Outcomes of a Combined Single Inpatient Procedure Versus Separate-Session Procedures[J].J Gastrointest Surg,2018,22(3):451-459.
[16] Sarli L,Iusco D R,Roncoroni L.Preoperative endoscopic sphincterotomy and laparoscopic cholecystectomy for the management of cholecystocholedocholithiasis:10-year experience[J].World J Surg,2003,27:180-186.
[17] Tazuma S,Unno M,Igarashi Y,et al.Evidence-based clinical practice guidelines for cholelithiasis 2016[J].J Gastroenterol,2017,52:276-300.
[18] Boerma D,Rauws E A,Keulemans Y C,et al.Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones:a randomised trial[J].Lancet,2002,360(9335):761-765.
[19] Srinivas G N.Conversion rate for laparoscopic cholecystectomy after endoscopic retrograde cholangiography in the treatment of choledocholithiasis:oes the time interval matter?[J].Surg Endosc,2006,20(12):1932.
[20] Boskoski I,Costamagna G.How to Prevent Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis[J].Gastroenterology,2020,158(8):2037-2040.
[21] Fogel E L,Lehman G A,Tarnasky P,et al.Rectal indometacin dose escalation for prevention of pancreatitis after endoscopic retrograde cholangiopancreatography in high-risk patients:a double-blind,randomised controlled trial[J].Lancet Gastroenterol Hepatol,2020,5(2):132-141.
[22] Dumonceau J M,Andriulli A,Elmunzer B J,et al.Prophylaxis of post-ERCP pancreatitis:European Society of Gastrointestinal Endoscopy (ESGE) Guideline-updated June 2014[J].Endoscopy,2014,46(9):799-815.
(收稿日期:2020-12-30) (本文编辑:张明澜)