Vitreoretinal surgeons’ experience and time interval from pars-plana vitrectomy to cataract extraction
Yan-Xin Xu, Liang-Ping Liu, Jian-Bing Li, Huan-Huan Cheng, Min Hou, Lin Lu, Ming-Xing Wu
State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou 510060, Guangdong Province, China
Abstract
INTRODUCTION
With the continuous evolution of instrumentation and techniques, pars-plana vitrectomy (PPV) has been extensively applied in the treatment of vitreoretinal disorders. Cataract formation is a frequent late postoperative complication, with up to 80%[1-2]of cases developing cataracts within 2y and of these almost 100%[3-4]developing nuclear sclerotic cataract. Phacoemulsification with intraocular lens (IOL) implantation is the most common treatment for cataracts, but there are many surgical challenges in vitrectomized eyes[5]. Patients with vitreoretinal diseases are generally young, and the eye is unable to accommodate after cataract extraction (CE), which brings many inconveniences to life and work, and increases the health-care costs and financial burden to families and societies.The exact cause of cataract development after PPV remains unclear; some predisposing factors have been proposed, such as patients’ age[6-7], the use of silicone oil (SO) or intravitreal gas[7-8], lens injury during PPV[9], the complexity of vitreoretinal disease[5], diabetic retinopathy[5,10], and duration of surgery[11]. The time interval from PPV to CE is determined largely by the speed of progression of cataract after vitrectomy, with more rapid progression indicating shorter time intervals.
The cataract surgeon’s grade and annual case volume are related to better visual acuity outcomes and a lower complication rate[12]. However, any association between vitreoretinal surgeons’ experience and the time interval from PPV to CE has rarely been reported. A previous study found that post-vitrectomy cataract progression is not associated with surgeons’ experience[13], but the study was limited by its sample size, and no further studies have been conducted.
The primary aim of this study was therefore to identify the associations between vitreoretinal surgeons’ experience and the time interval from PPV to CE.
SUBJECTS AND METHODS
Ethical ApprovalThe study was performed in accordance with the Helsinki Declaration and approved by the Zhongshan Ophthalmic Center Ethical Committee.
Data Extraction and Patient SelectionAll patients who underwent CE at Zhongshan Ophthalmic Center, Guangzhou, China from January 1, 2012 to June 30, 2018 were enrolled in an electronic medical record system.
Patients aged 18y or older with prior PPV who underwent phacoemulsification and IOL implantation in the hospital were included. Eyes that underwent phacovitrectomy were excluded. Eyes with a history of ocular diseases that could cause cataract formation or progression, including corneal disease, glaucoma, uveitis, endophthalmitis, optic nerve disease, and blunt or penetrating trauma, and eyes that had multiple intraocular procedures other than SO removal were also excluded. Patients whose records showed incomplete data were excluded. For patients in whom surgery was bilateral, only one eye was randomly selected in the final analyses.
Data were extracted from patient records and included the patient’s age, gender, diabetics status, the gauge of PPV, duration of surgery, the intraocular tamponade, the complexity of vitreoretinal diseases, the surgeon’s number of years as a practicing surgeon (years in practice) and annual case volume, and the dates of the PPV and CE surgeries. The time interval from PPV to CE was defined as the date of CE minus the date of PPV and recorded accurately to the nearest month.
Surgeons’ ExperienceTo describe the experience of each surgeon, the number of years of practice in vitreoretinal surgery and the annual case volume were both considered. Years in practice were determined by subtracting the year of PPV from the year of residency completion of the PPV surgeon and recorded as the practice years of the surgeon which was updated annually as the study progressed. Surgeons were categorized according to the number of practice years into three subgroups: ≤10y (junior), 11-20y (mid-level), and >20y (senior). For each patient case, the surgeon’s annual case volume was defined as the number of cases performed by the surgeon during the same year as surgery performed in that case. Annual case volume was categorized into five subgroups: <400, 400-599, 600-799, 800-999 and ≥1000 cases/year.
Complexity of VitrectomyFor analysis, complexity of PPV surgery was categorized into 4 levels as described in a previous study[5]: Level 1, vitreous opacities: including vitreous opacity caused by various vitreoretinal diseases except for proliferative diabetic retinopathy (PDR). Level 2, vitreoretinal interface diseases: including macular membrane, macular hole, and vitreomacular traction. Level 3, rhegmatogenous retinal detachment (RRD): including RRD with proliferative vitreoretinopathy (PVR) grade C1 or less. Level 4, complex vitrectomy: including PDR with epiretinal membrane and retinal detachment with PVR over grade C1.
Duration of SurgeryThe duration of surgery was defined as the time from the opening to the closing of the scleral incision, and it was recorded by the operating room staff using an electronic timer.
Statistical AnalysisAll statistical analyses were performed using SPSS software version 19.0 (Stata CorpLP, College Station, TX, USA). Variables are described by type as proportions or medians with interquartile ranges (IQR) or mean±standard deviations (SDs) as appropriate. Because the time interval data were non-normal, Mann-WhitneyUor Kruskal-WallisHWilcoxon tests were used to determine significance. After mean square root transformation, time interval data were approximately normally distributed. Univariate linear regression analysis was used to assess the effects of various variables on the time interval from PPV to CE. All covariates reaching significance with no multicollinearity between them were included in the multivariate linear regression analysis. A Chi-square test was used to compare cases complexity between annual case volume subgroups. AP-value <0.05 was considered statistically significant. For multiple tests, theP-value was corrected using the Bonferroni method.
RESULTS
A total of 132 430 cataract surgeries were performed during the study period, and of these 2.4% (3285) cases had simultaneous or prior vitreoretinal surgeries. Among them, 78.2% (2571) cases had phacoemulsification with prior PPV, and data from 1445 eyes met the inclusion criteria and were analyzed (Figure 1). Among the 1445 eyes, there were vitreous opacities in 119 eyes (8.3%), vitreoretinal interface diseases in 393 eyes (27.2%), retinal detachment in 732 eyes (50.6%), and PDR in 201 eyes (13.9%). The patients with intraocular gas tamponade were positioned face down after operation for 1 to 3wk. And the patients with SO tamponade were positioned face down for 3d to 3mo. At the time of CE, the type of cataract was recorded as nuclear sclerosis (86%), posterior subcapsular (7.8%), or cortical (6.2%).
Patients’ CharacteristicsThe median time interval was 13mo (IQR 8-19). The baseline characteristics and time intervals of all variables are shown in Table 1. The average age of the patients was 55.25±10.51y (mean±SD), and slightly more than half of the patients were men (54.7%). The median time intervals for men and women were 12mo (8-19) and 13mo (8-20), respectively (P>0.05). Most of the patients (85.9%) were without diabetes, and the median time interval for patients without and with diabetes was similar, at 12mo (P>0.05).
Gauge of PPVTwo thirds (65.5%) of patients underwent 23-gauge (G) PPV, and only 1.2% of patients underwent 27-G PPV. The number of patients who received 20-G and 25-G PPV was similar. From 20-G to 23-G PPV, the time interval increased with reduced gauge size, while the interval for patients with 27-G PPV was similar to that of patients with 23-G PPV (P>0.05).

Figure 1 Flowchart showing the filtering process of the study population.
Intraocular TamponadeEyes with C3F8 tamponade had the longest time interval [median: 14mo (IQR 9-23)], and eyes with balanced salt solution (BSS), air and SO tamponade had a similar time interval (13mo). For patients with SO tamponade, 23.5% underwent SO extraction with simultaneous CE (SO+CE), and these patients had the shortest time interval [7mo (6-10)] (P<0.05).
Duration of SurgeryThe median surgery duration was 50min, and the time interval for patients requiring less than or more than 50min to perform the PPV was similar (12mo,P>0.05).
Complexity of VitrectomyThe complexity of surgery is classified into four levels from low to high. Cases with complexity at level 4 had the shortest time interval [12mo (8-17)], while the remaining complexity subgroups had similar intervals (P<0.05).
Surgeons’ ExperienceThe median practice years of surgeons was 20y (IQR 14-26). Among all the included cases, those performed by senior surgeons had the longest time interval [13mo (9-20)], followed by mid-level surgeons [12mo (7-18)], and junior surgeons [11mo (5-18)] (P<0.05).
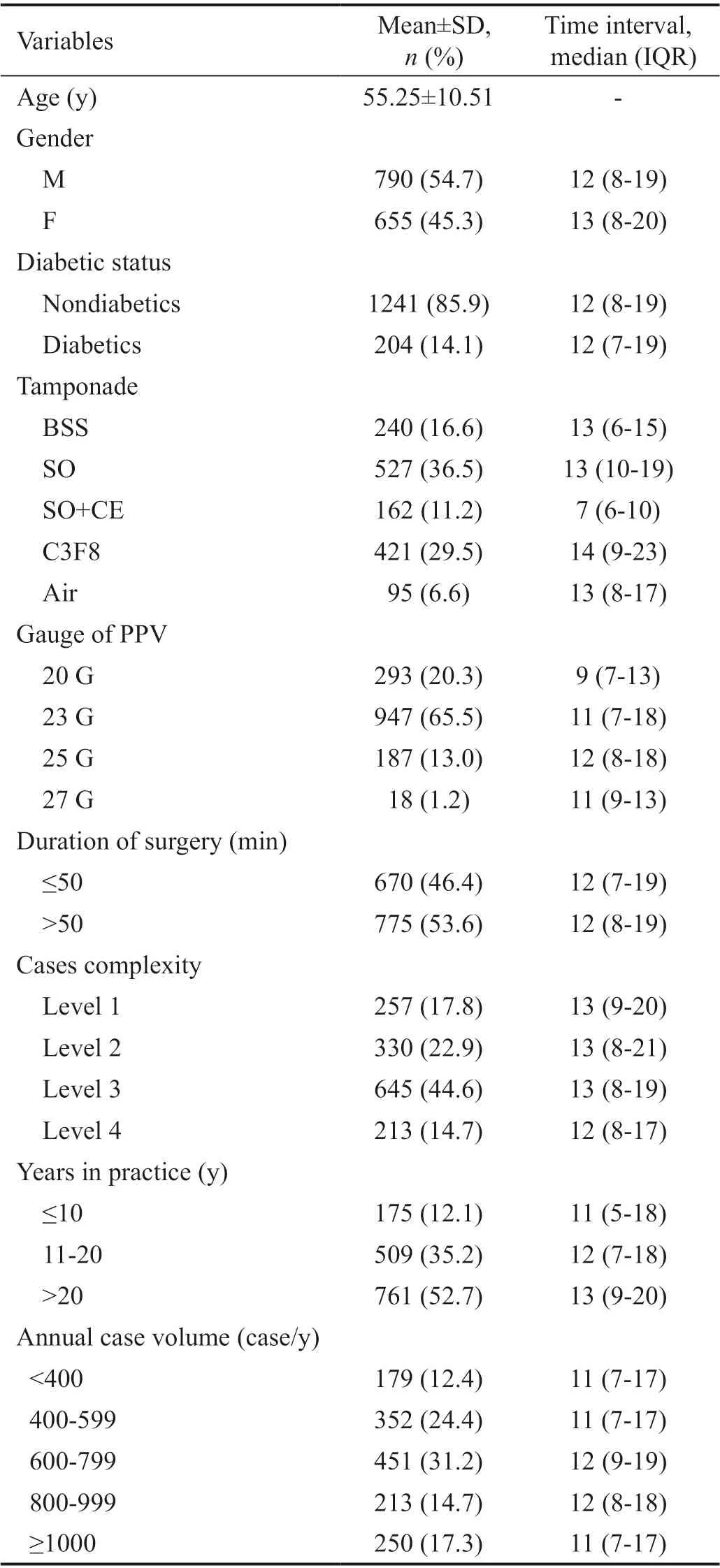
Table 1 Baseline characteristics and the time interval
The median annual case volume was 667 cases/year (IQR 520-859). Cases performed by surgeons with annual case volumes of 600-799 and 800-999 cases/year had the longest time interval (12mo). The rest of the annual case volume subgroups had the same intervals (P>0.05).
Linear Regression AnalysisThe linear regression analysis for the time interval is shown in Table 2.
Patients’ age was negatively correlated with time interval aftercontrolling for other variables (β=-0.017, 95%CI: -0.024 to -0.010,P<0.001) but no significant association was found between time interval and gender (P=0.691).

Table 2 Linear regression analysis for the time interval
Time interval was similar in patients with and without diabetes (β=0.855;P=0.314) and did not diあer significantly with PPV gauge (P>0.05) or duration of surgery (P=0.256).
Compared with patients with BSS tamponade, patients with SO+CE had a shorter time interval (β=-0.449, 95%CI: -0.723 to -0.174,P<0.001), and patients with C3F8 tamponade had a longer time interval (β=0.486, 95%CI: 0.259 to 0.713,P<0.001), as determined using multivariate regression analysis controlling for other variables.

Table 3 Years in practice and classification of cases complexity according to surgeons’ annual case volume
In univariate linear regression analysis, cases performed by mid-level and senior surgeons had longer time intervals compared with that performed by junior surgeons (allP<0.05). In multivariate regression analysis, time interval was significantly longer following surgery by senior versus junior surgeons after controlling for other variables (β=0.329, 95%CI: 0.113 to 0.549,P=0.003) but did not diあer between mid-level and junior surgeons (P=0.512).
In univariate linear regression analysis, time interval did not diあer significantly with annual case volume (allP>0.05, Table 2).
Surgeons’ Practice Years and Annual Case VolumeFor all case complexity classification subgroups, the time interval was prolonged as the surgeons’ practice years increased (P<0.05 for level 2 and 3 subgroups) except in the level 1 subgroup(Figure 2).Surgeons with fewer than 400 cases/year were the least experienced, with a median of 9y in practice, and those with 600-799 cases/year were the most experienced, with a median of 26y in practice (Table 3). Surgeons performing the highest volume had 24 practice years. Differences in the surgeons’ practice years between the annual case volume subgroups were significant (P=0.017). However, case complexity was similar between diあerent case volume subgroups (P=0.069).
Case volume of junior surgeons did not exceed 800 cases per year, and the time interval showed an upward but not significant tendency as this volume increased within this subgroup (P>0.05). The upward tendency was found among senior surgeons (P<0.01), but for mid-level surgeons, time interval showed the opposite trend, decreasing with case volume (P<0.01; Figure 3).
DISCUSSION
In this retrospective clinical study, the relationship between surgeons’ experience and the time interval from PPV to CE was analyzed, controlling for the patients’ age, gender, diabetics status, the gauge of PPV, duration of surgery, intraocular tamponade, and case complexity. Number of years in practice was a protective factor for the time interval, but the surgeons’ annual case volume had no significant relationship with time interval. In addition, patients’ age, SO tamponade, and complicated vitreoretinal surgery were predisposing factors for a shorter time interval. The median time interval between CE and the initial PPV was 13mo (mean±SD, 16±14.6mo), similar to previous reports[5,14-16].
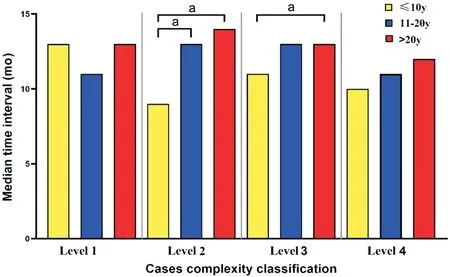
Figure 2 The median time interval of all years in practice subgroups among diあerent case complexity classification aP<0.05, Kruskal-Wallis H test.

Figure 3 The trends of the time interval of all practice years subgroups as the annual case volume increased.
The surgeons’ grade was associated with a shorter duration of surgery and lower complication rate in CE[17]. A previous study suggested that vitreoretinal surgeons’ experience was associated with the progression of nuclear sclerosis[13]but largely accounted for the differences in the proportions of preoperative nuclear sclerosis and the duration of follow-up. In the present study, surgeons with a higher number of practice years were associated with a longer time interval to CE after PPV compared with surgeons with fewer practice years, after controlling for the patient’s age, gender, diabetics status, the gauge of PPV, duration of surgery, intraocular tamponade, case complexity, and the surgeons’ annual case volume. The association may indicate that more experienced surgeons possess particularly fine-tuned surgical skills that further reduce the likelihood of lens damage and other complications.Volume-outcome studies have shown that surgeons who perform more operations have better patient outcomes than those performing fewer operations[18]. Previous studies have also shown that cataract operations performed by surgeons with high surgery volume have better postoperative visual acuity outcomes and fewer complications[17,12]. However, the present study found no correlation between the surgeons’ annual case volumes and the time intervals, and surgeons’ practice years were not associated with their annual case volumes. In addition, the proportions of cases complexity in annual case volume subgroups were similar. As the annual case volume increased, the number of complicated surgeries also increased, but the practice years of surgeons did not increase correspondingly. Consequently, the time intervals were shortened when the lower-practice-year surgeons performed complicated surgeries.
A correlation between patient age and cataract progression after PPV has been reported in previous studies[6-7,19-20]. Melberg and Thomas[6]found that the incidence of nuclear sclerosis within two years after vitrectomy was 7% in people under 50 years of age and 79% in those older than 50. In broad agreement with this, the present study found that patient age was negatively correlated to the time interval.
Previous findings indicate a lower rate of CE after vitrectomy in diabetic patients than that in nondiabetic patients, because vitreous oxygen tension was significantly lower in diabetic patients with ischemic retinopathy[10,21]. However, the present study found no diあerence in the time interval between patients with and without diabetes. The shorter time interval found previously in diabetics may relate to a higher frequency of examinations in those patients and a possible misattribution of poor vision to lens opacity without clinical significance[22]. In addition, patients with diabetes in the present study did not all have ischemic retinopathy.
Small gauge PPV in vitreoretinal surgery has been associated with less postoperative inflammation, lower complication rates, and time savings[23]. In the present study and in one former study[24]the gauge of PPV was not significantly associated with the time interval to CE. Further research is needed to understand why time interval was not aあected by the advantages of smaller gauge PPV.
随着新媒体迅速发展,出版宣传方式更加多元。互联网凭借技术优势,不断推进议程融合和关联网络议程设置。传统的传播模式正在改变,议程设置的重点由“媒体”转向“社群”。主题出版要顺应互联网时代的发展潮流,利用好网络媒体和移动社交新媒体,全面启动微信、微博等网络宣传渠道对既定目标群体进行精准投递,通过用户口碑传播推广,实现品牌的病毒式传播,以此节约人力成本和推广费用,增加盈利能力。
Previous studies have shown that eyes with intraocular gas filling do not show increased cataract progression after vitrectomy[19-20], while other studies have the opposite outcome[1,7]. Eyes with air tamponade were not related to cataract development[5]. In the present study, intraocular tamponade with air was not related to the time interval, but longer time intervals were found in eyes with C3F8 tamponade. A transient posterior subcapsular cataract has been reported after PPV when gas was injected into the vitreous cavity[1], but the long-term eあect of gas on the lens is not well understood. Intraocular SO tamponade has been found to increase cataract progression after vitrectomy[25-26]. In the present study, the time interval was shorter in eyes that underwent SO+CE, while eyes with SO tamponade in which SO was removed with delayed CE had similar time intervals to those with other types of tamponade. This finding is in line with those reported in a recent study[5].
It has been reported that light phototoxicity, intraoperative oxidation of lens proteins, and exposure to irrigating solutions are associated with the development of cataracts after PPV[5]but the duration of PPV surgery was not correlated with changes in nuclear sclerosis progression[11,19-20]. Consistent with these findings, no significant difference in time interval was found between patients undergoing PPV within 50min and over 50min in this study.
Time interval was shorter in high complexity cases in this study, in agreement with previous research[5]. In RRD and PDR surgeries, more action was taken to remove peripheral vitreous, which may increase the risks of lens injury and accelerate the development of cataracts.
It is important to consider the clinical significance of the present findings. Although many factors affected lens opacification after vitrectomy, 83% of patients needed CE within 24mo after PPV in this study. Combined phacoemulsification with vitrectomy should be considered.
Study LimitationsThis study has some limitations. First, this was a retrospective single-center study. However, the Zhongshan Ophthalmic Center has the largest CE volume in China, and the results of this study can therefore be extended to most hospitals. Second, the time interval from PPV to CE was used as an indicator of cataract progression after PPV, and this indicator is aあected by subjective factors such as the patient’s preference and the individual surgeon’s threshold for CE surgery. Third, no detailed information is available about the duration of surgery with patients in prone (face down) position, so its impact on cataract progression cannot be analyzed, and further prospective study is needed to understand this potential factor.
In conclusion, this study found that surgeons with more years in practice were associated with a longer time interval to CE after PPV and more experienced surgeons were associated with longer intervals in complicated cases. The annual case volume of surgeons had no clear relationshipwith the time interval in non-low-complexity cases. In addition, aging,
SO tamponade, and complicated vitreoretinal surgery were predisposing factors for a shorter time interval. These findings may indicate the necessity of surgery allocation according to the classification of cases complexity in ophthalmic hospitals, particularly in regions with high patient-to-surgeon ratios.
ACKNOWLEDGEMENTS
Authors’ contributions:Conception and design: Wu MX, Xu YX; Provision of study materials or patients: Xu YX, Liu LP; Collection and assembly of data: Xu YX, Liu LP; Data analysis and interpretation: Xu YX, Liu LP, Li JB, Cheng HH; Manuscript writing: All authors; Final approval of manuscript: All authors.
Foundations:Supported by the National Key Research and Development Program of China (No.2017YFC1104603); the National Natural Science Foundation of China (No.81770909; No.81970783).
Conflicts of Interest: Xu YX,None;Liu LP,None;Li JB,None;Cheng HH,None;Hou M,None;Lu L,None;Wu MX,None.
 International Journal of Ophthalmology2021年1期
International Journal of Ophthalmology2021年1期
- International Journal of Ophthalmology的其它文章
- Response of L V Prasad Eye Institute to COVID-19 outbreak in India: experience at its tertiary eye care centre and adoption to its Eye Health Pyramid
- Preliminary studies of constructing a tissue-engineered lamellar corneal graft by culturing mesenchymal stem cells onto decellularized corneal matrix
- Therapeutic potential of Rho-associated kinase inhibitor Y27632 in corneal endothelial dysfunction: an in vitro and in vivo study
- Changes of matrix metalloproteinases in the stroma after corneal cross-linking in rabbits
- A multi-omics study on cutaneous and uveal melanoma
- Eあects of quercetin on diabetic retinopathy and its association with NLRP3 inflammasome and autophagy
