Response of L V Prasad Eye Institute to COVID-19 outbreak in India: experience at its tertiary eye care centre and adoption to its Eye Health Pyramid
Rohit C Khanna, Prashant Garg, Pravin K Vaddavalli, Merle Fernandes, Suryasnata Rath, Sameera Nayak, Raja Narayanan, Rajeev Reddy Pappuru, Swathi Kaliki, Anthony Vipin Das,9, Savitri Sharma, Subhadra Jalali
1Allen Foster Community Eye Health Research Centre, Gullapalli Pratibha Rao International Centre for Advancement of Rural Eye Care, L V Prasad Eye Institute, Hyderabad 500030, India
2Brien Holden Eye Research Centre, L V Prasad Eye Institute, Hyderabad, Telangana 500034, India
3School of Optometry and Vision Science, University of New South Wales, Sydney 2033, Australia
4University of Rochester, School of Medicine and Dentistry, Rochester, NY 14642, USA
5Kallam Anji Reddy Campus, L V Prasad Eye Institute, Hyderabad 500034, India
6Grandhi Mallikarjun Rao Varalakshmi Campus, L V Prasad Eye Institute, Vishakhapatnam, Andhra Pradesh 530040, India
7Mithu Tulsi Chanrai Campus, L V Prasad Eye Institute, Bhubaneswara, Odisha 751024, India
8Kode Venkatadri Chowdary Campus, L V Prasad Eye Institute, Vijayawada 521134, India
9Department of eyeSmart EMR & AEye, L V Prasad Eye Institute 500034, India
Abstract
INTRODUCTION
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which originated from Wuhan, China has spread across 213 countries. It has infected nearly 6 million individuals and killed more than 350 000, as on 31stMay 2020[1]. It is now well known that SARS-CoV-2 causes coronavirus disease 2019 (COVID-19) and is transmitted by droplets, aerosol particles, fomites and transient air borne particles[2]. There are reports of feco-oral route of transmission too[2]. The most common symptoms reported are fever, cough, dyspnoea, myalgia, anosmia and fatigue[3-4]. Less frequently reported symptoms are phlegm, haemoptysis, headache and diarrhoea. Rarely, conjunctivitis can be the first symptom. Advisory measures include social distancing, working from home, and safe hygiene practices. Legal measures include travel restrictions, reduction or postponement of elective procedures, and lockdown and curfews[5].
Health care professionals are at an increased risk of infection. In one study it was found that more than 40% of the infection was hospital acquired, with health professionals being mostly affected[3,6]. Ophthalmology as a specialty is at an increased risk as most of the procedures bring the clinicians in close contact with patient’s eyes (less than 20 centimeters for most procedures). Various parts of the patient’s face touch most of the ophthalmic equipment, thus increasing the risk of spread of infection through aerosolized particles from respiratory droplet and contact[7]. There are also reports of SARS-CoV-2 identified in tears and conjunctival swabs, thus putting ophthalmologists at risk of acquiring the infection[8-12].
Guidelines have already been developed for ophthalmologists by the American Academy of Ophthalmology (AAO)[13], International Council of Ophthalmology (ICO)[14]as well as diあerent National Societies such as All India Ophthalmological Society (AIOS)[15]. However, there are limited reports on hospital response to COVID-19[16-17].
In India, the first case of COVID-19 was reported on January 30th, 2020 from the Southern state of Kerala through a traveler from Wuhan. COVID-19 was reported in Hyderabad a month later on March 2nd2020 through a traveler from Dubai. A sharp increase in numbers then followed. India went into a countrywide strict lockdown on March 23rdfor 3wk, which was further extended by another 3wk until May 3rd2020[18]. Subsequently, from May 4th, 2020, India was divided into three zones at the district level, Red, Orange and Green, based on the presence of active cases in the community. Red zones included areas with high numbers of new active cases, Orange zones with no new cases reported in last two weeks, and green zones with no active COVID-19 cases[18]. While, lockdown continued in red zones, there were some relaxations given in orange and green zones[18].
The lockdown, while saving lives and flattening the curve, by reducing the number of patients reporting together to hospitals, continues to have detrimental effect on the Indian economy. The health care industry was also badly hit and had to prepare guidelines at short notice to take care of patients and staff. Currently, the health care industry is trying to revive, as the country moves to a slow exit from the lockdown. Hospitals need to rapidly develop new operational guidelines and exit strategy, for implementation post lockdown. Based on the available evidence, we herein summarize our experience from a tertiary eye care institute in India, which also manages a network of secondary and primary eye health centres through its unique eye health pyramid[19]. Our response to COVID-19, pre-lockdown, during lockdown as well as the exit strategy post-lockdown are detailed. We hope that our experience will provide guidelines to the ophthalmic community, to develop protocols for care at various levels in the community, and to protect ophthalmologists and ophthalmic care personnel as well as their patients across the world.
We based our strategy plan on the level of threats as was done in Singapore[20]. The Hospital Infection Control Committee (HICC) held the first meeting on January 10th(first case reported to World Health Organization on Dec 31); gave this serious attention and initiated steps on February 20th; and more detailed action on March 2nd(after the first case was reported in Hyderabad, where our main campus is situated). Steps were taken to consolidate actions, and at each step, importance was given to: Clear evidence from literature and protocols; Clear instructions and communication; Monitoring and auditing of compliances; Getting feedback and improving; Daily meeting of nodal and strategy teams with updated data and actions.
OUR RESPONSE TO COVID-19 CAN BE DIVIDED INTO THE FOLLOWING STEPS
1) Administrative control; 2) Patient triaging and clinical protocols; 3) Staあ protection; 4) Environmental protection; 5) Social distancing measures; 6) Communication strategy; 7) Monitoring.
Response was based on the principles of social distancing, hand hygiene, following respiratory etiquettes, surface disinfection protocol, and rational use of appropriate personal protective equipment (PPE). The response was also aligned with the core values of the institute-patient first, excellence, equity, togetherness and integrity.
Administrative Control
On March 8th, a formal COVID-19 Task Force and
Situation Room was set up consisting of Nodal Person In
chargeNetwork Head of Quality along with Network Head of Infection control with overall responsibility of adopting and implementing the best Global and National practices. They were also responsible for coordination with members of the Task Force and communication to the entire network of 208 centres within our Eye Health Pyramid.
Strategy CommitteeThis consisted of Directors of diあerent campuses, Director of Operations, Director of Public health, key administrators and executives from diあerent departments.Their role includes ongoing monitoring of the situation on the ground, brainstorm various issues and propose action items. The Chairperson and three vice chairs guided the committee.
Action Plan Execution CommitteeAdministrators and executives from all areas of the Institute are included in this committee, with responsibility to implement, monitor compliance and report to nodal and strategy committee.
Patient Triaging and Clinical Protocols
Pre-lockdownAppointments of all international patients were rescheduled. They were advised to regularly follow Government of India notifications regarding travel advisories and quarantine rulings. Retinoblastoma patients were helped through personal interactions with the local Indian Embassy. All patients with appointments were sent a message (SMS) one day prior to appointment with the following advise: ‘If you have cold, cough, breathlessness, head-ache and fever, please consult a general physician before coming for your eye checkup.’Temperature screening (for patient and staあ), and patient triaging was started and at the same time, and the policy of one attendant with each patient was reinforced. Patients were instructed to avoid public mass transportation, rather take taxi or self-drive. All those with cough/cold/fever were referred to Government hospital. Any of the staあ having cold/cough/fever was granted leave and advised to consult a doctor. All those with personal or family history of international travel, or those who had contact with anyone who travelled internationally, were also monitored for COVID-19 symptoms. Isolation room was kept ready to handle any encountered with a COVID-19 case or suspect.
In out-patient area, all slit lamps were fitted with an acrylic sheet or an X-ray film to protect from direct aerosol of the patient (Figure 1). The innovation team designed an in-house 3D printed protective face mask for all the staff. The design was made open source freely available on our website (https://lvpmitra.com/osvisor). For those directly dealing with patients, triple layer surgical masks were provided. Others were provided cloth masks.
During examination, no talking policy was followed. Clinicians were instructed to avoid all non-essential non-critical examinations and explain to the patients about the truncated protocol. The deferment and the need for more elaborate testing in future was documented in the medical record. All staff were directed to greet patients strictly with “Namaste”, and to avoid shaking hands and any physical contact with the patients without gloves.
Aerosol generating procedures such as non-contact air puff tonometry was discouraged as was the use of direct ophthalmoscopic evaluation where the close contact situation poses higher risk of cross infection[21]. Fundus examination was done with indirect ophthalmoscopy rather than biomicroscope with +90/78 D lens. They were directed to minimize the number of staあ in examination room, ideally one ophthalmologist, one optometrist and one patient and his/her attendant. Guidelines for handling conjunctivitis patients were strictly followed by the clinicians. Full PPE was provided to all cadres of staあ who handle high aerosol situations including COVID-19 suspects.

Figure 1 Slit-lamps with an X-ray film for aerosol protection.
In operating room, full PPE was provided to those performing general anaesthesia, and procedures with potential for blood/body fluid spills. The PPE included disposable gowns, gloves, caps, N95 respirator mask, shoe covers and eye protection.
Being a standalone eye care facility, it was decided that COVID-19 positive patients, even if they need emergency eye care, would be directed to the COVID-19 facilities on priority (currently exclusively held by the Government).
During lockdownThe routine patient care in pre-lockdown period was changed to exclusively emergency services during lockdown. The appointments of all non-emergency patients were rescheduled and communicatedviaphone call by each consultant, text messages and/or e-mail. Optical services were closed. The consultants personally categorized their patients into red (need to come in urgently), yellow (can defer examination by 2-4wk) and green (can reschedule once situation is good after few months) groups, and conveyed to staあ for implementation. Patients were also provided direct accessviaphone should they wished to speak to their treating doctor.
List of emergencies was prepared by each specialty (Table 1), and only emergency surgeries were performed. Donning full PPE was mandatory for staあ handling emergencies.
There was significant drop in patients visit to the institute. In response to it, our standardized and robust Electronic Medical Record (EMR) system, integrated across the multi-tier ophthalmology network in our Eye Health Pyramid, helped to immediately start tele-ophthalmology and remote clinical examination with real time video[22-24]. In area of rehabilitation, tele rehabilitation services was started as well as online training videos were developed[25].

Table 1 List of ocular emergencies to be handled during lockdown
In order to address rural distress, phone calls were made to all our patients of our primary and secondary centres in the EMR database, irrespective of social and economic status. Additionally, we connected with the vulnerable blind clients of our rehabilitation services, both in cities and rural areas. Eighty thousand phone calls were made over 4wk to check on their health, any family issues, and support required and this is ongoing. Support was extended to those identified with needs, such as small monetary help, groceries, education, and rehabilitation needs, in addition to medical advice. At the same time, we also started exploring the opportunity of providing home-based consultation, especially to those elderly (60y and above).
Post lockdown and exit strategyA robust triaging system (six stations instead of one earlier) has been introduced and will continue. The patients will continue to be screened for temperature, any history of acute respiratory illness, and incidence of any contact with a COVID-19 case or suspect. Past visit to any other hospital or any social gathering in last 14d as well as history of quarantine has been added to the check-list, as it was noted that patients were deliberately suppressing this information. Patients from red zone or containment zone are handled separately. “Arogya Setu” app introduced by government of India to track contact with COVID-19 is also considered[26].All patients areinstructed to use face masks and COVID-19 consent form has to be filled prior to performing any out-patient or surgical procedures.Appointments have been reduced by 30 percent with slots spaced at 20min and will be gradually increased. Optical and contact lens services are resumed and patients with appointment will continue to be screened for COVID-19 risk as before. Patients, both with and without appointment will be examined irrespective of problem. Guidelines and protocols for home base consultation are also developed. As most of the patients would seek care closer to their home, our network of primary and secondary care in rural areas would be of additional benefit as care would be oあered closer to their homes.
Social distancing will be maintained at all levels (clinical and non-clinical areas) and examination protocols will remain same as in pre-lockdown period, with addition of refraction and glass prescriptions. All clinical staあ will continue to use full PPE (similar to lockdown period) and the names of all medical staff who examined or interacted with a patient are documented in EMR for any future tracking for exposure to COVID-19.
Based on government guidelines, as asymptomatic surgical patients do not undergo testing, universal precautions are followed. Pulse oximetry in Out-patient Department and Preoperative Room, to detect low oxygen saturation is already part of our standard of care. Patients operated under general anesthesia (GA) get an additional chest X-ray, to report for any signs of COVID-19 infection by the radiologist. Day care surgeries will be performed under local and preferably topical anesthesia. In GA cases, a full PPE is required (including water repellent gowns). A separate operating room (OR) is already allocated for GA cases. A gap of 20min is also recommended between two surgeries to allow aerosols to settle down. For retinal and oculoplastic procedures, full PPE is recommended due to fluid/blood seepage and aerosol generation with radio frequency cautery. High-eきcient particulate air filter (HEPA) units are used in operating rooms (already in place in tertiary centers). It is recommended not to open OR door during the surgery to avoid air turbulence.
There will be only one patient in each room in the wards. Wherever it is not possible, social distancing has to be maintained in wards and temperature of patient and attendant has to be measured every 12h. As far as possible, in-patients, should be examined in the ward itself. Once discharged, digital follow-ups with photos are recommended to the extent feasible, with minimal physical visits. The infection control nurse regularly communicates with and monitors the discharged patients for any symptoms related to COVID-19 during next 2wk.
Apart from this, faculty from the institute were also involved with the AIOS to develop clinical guidelines for various specialties. Apart from this, guidelines for secondary and primary eye care are also developed and implemented[27].
Staあ Protection
Pre-lockdownStaあ at all levels attended awareness sessions, and were properly educated. Several mock drills were held for employee awareness and self-protection. Surveillance systems were set up to understand the impact of awareness and training. Staあ also received guidelines for safety measures at their home. Importance of social distancing and hand hygiene practice were stressed. They were advised to avoid touching eyes, nose and mouth without washing hands, discouraged use of cell phones in patient care areas, and instructed to avoid wearing ornaments, watchesetc. Female staあ were specifically instructed to keep their hair tied and covered all the time.Staあ were also advised to postpone all social gatherings/parties/ceremonies/visits to temples and family holidays. All physical meetings at the institute involving external participants were cancelled from March 8thand online platform was used. Education classes were also suspended and moved to online platforms.
The staff who were given leave from workplace were instructed to remain isolated at home and not venture outside in the city or town for their own and their family’s safety. All employees returning from vacation were required to report to human resource (HR) department about their travel history and any history of contact with actual or potential patient (s).
Employees with high risk factors were encouraged to work from home. These include those 60y and above; those with systemic comorbidities and chronic diseases, involving respiratory, heart, kidney, liver, and neurologic conditions; uncontrolled diabetes, uncontrolled hypertension; cancer and those on immunosuppressive therapy[28]. Pregnant ladies were also asked to work from home until further notice.
To have an inclusive approach to our own staあ with disability, each such staあ member was approached at an individual level to facilitate their work and personal needs.
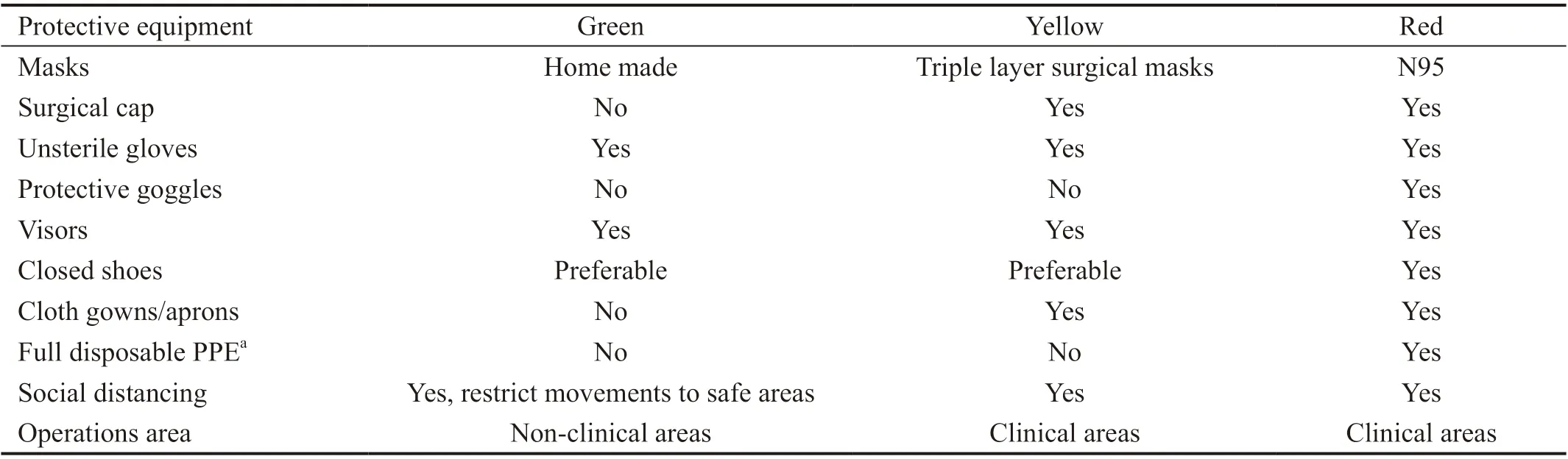
Table 2 Guidelines for using personal protective equipment
During lockdownStaff in every department was divided into three teams with adequate backup. Every team came twice in a week exclusively. Socializing among the teams was prohibited. Smaller departments would cover only some days of the week. If a replacement for a sick member could not be found, the work was managed by other staあ within the team itself. Daily staあ attendance was reduced to 15%. There were occasional difficulties related to non-availability of public transport, discovery of a positive case in their locality and sudden declaration as containment zoneetc. Shortage of staあ in certain areas was managed by organizing transport for select individuals and multi-tasking in the absence of certain other members.
Despite huge impact on revenues, there were no layoffs and no salary cuts. Fair dealing and support were not just limited to employees but also extended to our vendors and no payments were delayed. Some vendors were considerate owing to the extraordinary circumstances, and oあered to wait if LVPEI deferred their payments until the situation improved. Such offers were appreciated but respectfully declined. All pending payments were cleared so that the institute could start operations after normalcy is restored without any burden and obligation. Opportunities in other areas like engineering product, innovation products educational products and consulting were explored. Very stringent measures for expenditure reduction were put in place (reduction in rentals, consumables costs, utilities, traveletc.) as well as new hiring was stopped across the network.
In areas of training, numerous webinars for internal and external audiences were conducted and online resource materials for training were developed. During lockdown, faculty and fellows also utilized their time in writing as well as submitting numerous manuscripts and grant applications and these were monitored on a weekly basis creating a healthy competition while working from home.
Leave policy was modified for the rest of the year so that staあ were discouraged from taking unnecessary personal leaves.
Staあ were allowed to work from home wherever possible and monitored by weekly reporting. This included digital education and training, manuscripts preparation, designing protective wear, pending and new administrative protocols, digital rehabilitation, providing psychological support by phone callsetc.
All employees were placed under 3 categories (red, yellow and green) based on their risk of exposure. Guidelines for use of PPE were prepared (Table 2). All those in non-clinical areas were placed in green category, those in clinical area but not directly in contact with patients would be in yellow category, and those who come within 6 feet (1.83 m) of the patients or dealing with infected material would be in the red category. During lockdown, there was scarcity of temperature guns, triple layer and N95 masks in the market. In addition, vendors hiked the rates of all these items. With meticulous search, networking, and negotiations we managed to purchase these, however had to pay 50% more than the normal rates.
Post lockdownThe plan is to continue with the same teams for 4wk after which the situation would be reassessed. Those living in containment zones are advised not to come to the center at this time.Staff education is ongoing digitally for proper donning and doきng of PPE and steps in patient flow[29]. To enhance staff protection, updating influenza vaccine to the prevailing seasonal strain can be considered. A system has been set up for providing psychological support to staff. One member of HICC is always available to address staff apprehensions. A circular is sent to all staあ clearing their myths about COVID-19 as well as bringing more awareness among them. Session by external physicians dealing with COVID-19 is organized to present facts and clear myths. Positive messages to alleviate fear is also circulated. Daily calls and meetings are arranged across all cadres of staあ to assess their wellbeing. Meditation sessions for certain cadre of staff is also organized. All the staあ members are trained for increased efficiency and reducing expenditure and administrators are developing future plans in each area. Employee check list for reporting to work is developed, this includes details on staff retuning from travel, protocols to be followed at workplace, protocols if any staff is found to be symptomatic, guidelines home quarantine for staff, guidelines to be followed if any family member is suspected or turned out to be positive and guidelines for use of hydroxychloroquine (HCQ) prophylaxis. Some of the staあ took up the contact tracing courses online to help with the contact tracing, thus helping in mitigating the risk of COVID-19 spread in the hospital[30]. For staあ who develops symptoms, we tied up with a local laboratory for carrying out investigations. At the same time, facility for performing ‘rapid antigen’ testing is initiated in different campuses. All staff and their family were already covered under regular health insurance facilitated annually by the institute and information for possible enhanced insurance for COVID-19 was provided. For students’ special negotiations resulted in very reasonable packages of insurance cover. In addition to this, we tied up with various hospitals locally for any staあ needing emergency COVID-19 related admission.
Environmental Protection
Pre-lockdown periodCoronavirus can survive on different surfaces for a long time, plastic (72h), stainless steel (48h), cardboard (24h), and copper (4h)[7,31]. While other coronaviruses have been found to survive on surfaces for 6d, there are no reports related to this on SARS-CoV-2[32]. SARSCoV-2 can be killed with 70%-90% ethanol or 1% sodium hypochlorite[33]. Washing hands with soap and water for 40-60s before and after examination was also recommended. Povidone-Iodine or a combination of chlorhexidine with ethanol and cetrimide was also used for infection control[34-35]. Cleaning and disinfectant guidelines were prepared and both clinical and housekeeping staff were trained to follow these. Non-clinical areas were cleaned twice a day and clinical areas were cleaned 4 times a day. All surfaces were cleaned including floors, doors, door handles, knobs, hand railing of staircase, lift, waiting area chairsetc. Sanitizers were placed at diあerent locations in all floors for use of staあ and patients. Education of staあ, improved hygiene surveillance and information sharing became regular practices.
A separate room was allocated near the entrance for isolation of any COVID-suspect. In addition to the existing safety alert codes, a new ‘Code Gray’ was introduced. This is not for announcement on public address system. It is to alert the internist about a COVID-suspect, and is conveyed on intercom phone to attend to the patient in full PPE.
The staあ optometrists were trained to clean the slit lamp, chin rest, head band, acrylic sheet as well as patient seat with 70% isopropyl alcohol after each patient. The computer, mouse, keyboard, tablets,etc. were also cleaned in between patients. Similar method of cleaning all diagnostic equipment was followed after every use. Guidelines for cleaning was prepared and circulated. The occludes (used for testing binocular vision and those used in trial frame), trial frames, and lenses were wiped with alcohol swabs after checking vision or doing refraction for each case. Hands with or without gloves, were cleaned with 70% isopropyl alcohol before touching any equipment.Air conditioning restriction/stoppage and opendoor policy was followed at all locations (except operating room and some diagnostic equipment that do not work in high temperatures). Bedsheets/towels in the wards were to be washed with soap and water after single use. All blankets were removed. In the optical outlets, patients were asked to clean their hands with 70% isopropyl alcohol before touching any frames. Sample frames tried by patients, mirror and furniture were cleaned with alcohol swabs immediately after every use.The hospital ambulance, including handles, window panes, and the seats, was cleaned twice a day and after every use, with quality disinfectant cleaner (Lemonizer-Granadier brand, 1% dimethyl benzyl ammonium chloride). All material received in the stores was kept separate from main stock and sanitized. Hands were washed after touching any material. The canteen staff were instructed to maintain personal hygiene and were monitored closely. They were asked to use personal protection while handling/serving food. The master cook was provided hospital accommodation. Similar protocols were followed in other non-clinical areas like human resource department, accounts, information technologyetc.
During lockdownAll the above guidelines were followed. Additionally, the entry and exit routes were separated for staあ and patients. Out-patient and operating room areas were re-allocated for efficiency. Several areas in the building not required for patient care were shut down to reduce costs.
Post lockdownAll the above guidelines would be followed and depending on the need, more areas will be opened up in a phased manner. It is envisaged that most of the building will become functional over 2wk. Guidelines for staあ quarantine/isolation was developed based on the risk post-exposure[36].
Social DistancingAll areas were decongested (including dining area) with staggered timing. Out-patient area was decongested and the patients were seated maintaining distance of 6 feet (1.83 m). The cafeteria seating was reduced to half. Chairs were placed at diagonal ends of tables at 6.5 feet (1.98 m) Extra eating areas were opened in other locations of the institute. Staあ were instructed to enter eating area only when a chair fell vacant and to leave as soon as they finished eating. They were advised to spread out lunch timing, and to avoid crowding in the cafeteria. All repair/construction projects were postponed until further notice. Staあ were discouraged use of elevators. When elevators were used however, gloves/elbows/cloth were used to touch elevators knobs and door handles, or sterilium/hand wash was used after touching these. Elevators were avoided for some minutes after other people had used them and only four passengers were allowed at one time, facing one wall each.
Communication StrategyCommunication strategy was also developed. Awareness posters in common local languages were displayed at prominent locations in the building and at the main gate. Robust and authentic communication was actively maintained with all cadres of staff daily lead by the head of Hospital Quality Control. The director or each campus discussed and reviewed operational plans with the clinical and administrative staff daily. Awareness videos on COVID-19, conjunctivitis and red eye were shown in the waiting lounges. A special section on ‘COVID-19’ was created on the institute’s intranet portal and updated daily with awareness messages. Videos for various protocols were developed and circulatedviadifferent communication channels. A major challenge was encountered in communicating with the staあ during this period, as the lower cadres did not have access to emails and social messaging platforms. Channels of communication that employees could access were mapped with the help of human resource (HR) department and were used appropriately. Multiple ways of communication with staff were designed, which included email, intranet, website, social media, digital classroom, land line and mobile telephones.
Monitoring
Pre-lockdownA monitoring checklist was developed by the quality team and was implemented by the execution team. The checklist included monitoring of one attendant policy, awareness of health messages, compliance with protocols, and cafeteria hygiene. The members of execution committee and quality team attempted to have one-to-one meetings with each employee, including contract employees, in all departments as an ongoing activity. The aim was to reduce anxieties, obtain feedback, and provide guidance for implementation, monitoring, and compliance. Employees were also trained to submit Incident Reports on any serious breach of protocol. Directors of other campuses and heads of centres at diあerent levels of the Eye Health Pyramid provided similar leadership in this situation
During lockdownThe team lead for that day made random checks to monitor all compliances. One person from the quality team was on the ground each day for handling incident reports, breached protocols, and monitoring sanitization of the isolation facility after each use.
Post lockdownMonitoring similar to pre-lockdown period will continue with more vigour.Twenty-five new standard operating protocols (SOP) were developed, one for each area of activity and for each clinical and non-clinical point of care (example vision check, refraction, tonometry, optical shop, contact lens trial, prosthetic eyeetc.). Implementation of these is ongoing.
DISCUSSION
These guidelines are based on best possible practices and upto-date evidence; and likely to be revised as new evidence is generated. Most of these guidelines were prepared through our experience in our centre of excellence for tertiary care. However, these are largely applicable and have been implemented (with a few exceptions like high end HEPA filters in operating rooms) across our network of secondary and primary eye care centres that constitute the Eye Health Pyramid. The key principles of behavioural changes, such as social distancing, hand hygiene, respiratory etiquettes, surface disinfectant protocol, clinical protocols, point-of-care checks, patient flow, and use of PPE could be implemented uniformly at all places irrespective of level of the care provided.
A good triaging system at multiple levels and following the best preferred practices would significantly mitigate the risk of COVID-19. COVID-19 is likely to stay with us and persist for a long time. The quicker we get used to the new system of functioning, and assimilate changed behaviors into our day to day work in eye care centers, the better it would be for everyone’s safety, and also for the overall economy and eye health of the country. We are quite confident that the protocols and processes adopted by our institute have prepared us for the post lockdown conditions. We also have confidence that we can exit the lockdown with very low risk to staff and patients from cross infection, in-spite of asymptomatic carriers of COVID-19 infection in the community. In two weeks, we expect to start routine eye care (except community screening) in a phased manner and get back to our mission of working towards blindness prevention and treatment to all those who need care. As we write this manuscript, many procedures including elective cataract and refractive surgeries have already started. Vision is critical for quality of life including economic independence of an individual, more so in these anxious and uncertain times.
ACKNOWLEDGEMENTS
Conflicts of Interest: Khanna RC,None;Garg P,None;Vaddavalli PK,None;Fernandes M,None;Rath S,None;Nayak S,None;Narayanan R,None;Pappuru RR,None;Kaliki S,None;Das AV,None;Sharma S,None;Jalali S,None.
 International Journal of Ophthalmology2021年1期
International Journal of Ophthalmology2021年1期
- International Journal of Ophthalmology的其它文章
- Preliminary studies of constructing a tissue-engineered lamellar corneal graft by culturing mesenchymal stem cells onto decellularized corneal matrix
- Therapeutic potential of Rho-associated kinase inhibitor Y27632 in corneal endothelial dysfunction: an in vitro and in vivo study
- Changes of matrix metalloproteinases in the stroma after corneal cross-linking in rabbits
- A multi-omics study on cutaneous and uveal melanoma
- Eあects of quercetin on diabetic retinopathy and its association with NLRP3 inflammasome and autophagy
- RNA interference targeting NOX4 protects visual function in an experimental model of retinal detachment by alleviating blood-retinal barrier damage
