NLR、TgAb与甲状腺乳头状癌颈部淋巴结转移的关系
许克 杨枋 谢应海 王培斌


[摘要] 目的 探究中性粒細胞/淋巴细胞比值(NLR)、甲状腺球蛋白抗体(TgAb)与甲状腺乳头状癌颈部淋巴结转移的关系。 方法 对2017年1月~2019年9月淮南市第一人民医院诊治的135例甲状腺乳头状癌患者进行临床研究,根据患者是否发生颈部淋巴结转移将其分为未转移组(72例)和转移组(63例)。记录两组患者的临床资料和病史资料,采用血细胞自动分析仪检测NLR值,采用全自动生化分析仪检测患者的生化指标,采用酶联免疫吸附法检测血清TgAb水平。采用logistic回归模型分析发生颈部淋巴结转移的影响因素,采用受试者工作特征曲线(ROC)分析NLR和血清TgAb对发生颈部淋巴结转移的预测价值。 结果 转移组的肿瘤直径、尿酸、尿素氮、肌酐、总胆红素、NLR和血清TgAb高于未转移组,差异有统计学意义(P < 0.05)。两组患者性别、年龄、高血压史、冠心病史、糖尿病史、合并甲状腺肿、肿瘤数量、胆固醇、三酰甘油、高密度脂蛋白和低密度脂蛋白比较,差异无统计学差异(P > 0.05)。logistic回归模型显示NLR和血清TgAb水平升高是甲状腺乳头状癌患者颈部淋巴结转移的独立危险因素(P < 0.05)。NLR联合血清TgAb[AUC = 0.874,95%CI(0.816~0.932),灵敏度=89.76%,特异度=90.58%]预测颈部淋巴结转移的临床价值明显优于NLR[AUC = 0.753,95%CI(0.673~0.833),灵敏度=76.53%,特异度=79.12%]和血清TgAb[AUC = 0.796,95%CI(0.724~0.869),灵敏度=80.47%,特异度=83.91%]单独检测。结论 NLR和血清TgAb水平异常升高均与甲状腺乳头状癌患者颈部淋巴结转移的发生密切相关,早期联合检测有助于预测甲状腺乳头状癌患者颈部淋巴结转移的发生风险,从而为临床制订针对性干预方案提供参考。
[关键词] 中性粒细胞/淋巴细胞比值;甲状腺球蛋白抗体;甲状腺乳头状癌;颈部淋巴结转移
[中图分类号] R736.1 [文献标识码] A [文章编号] 1673-7210(2020)04(b)-0093-05
Relationship between NLR, TgAb and cervical lymph node metastasis in papillary thyroid carcinoma
XU Ke YANG Fang XIE Yinghai WANG Peibin
Department of General Surgery, Huainan First People′s Hospital, Anhui Province, Huaian 232007, China
[Abstract] Objective To explore the relationship between neutrophil to lymphocyte ratio (NLR), thyroglobulin antibody (TgAb) and cervical lymph node metastasis of papillary thyroid carcinoma. Methods A clinical study was conducted on 135 patients with papillary thyroid carcinoma diagnosed and treated in Huainan First People′s Hospital from January 2017 to September 2019. The patients were divided into the non-metastatic group (72 cases) and the metastatic group (63 cases) according to whether they had cervical lymph node metastasis. Clinical data and medical history of patients in the two groups were recorded. NLR value was measured by automatic blood cell analyzer, biochemical indicators of the patients were measured by automatic biochemical analyzer, and serum TgAb level was measured by enzyme-linked immunosorbent assay. Logistic regression model was used to analyze the influencing factors of cervical lymph node metastasis, and receiver operating characteristic (ROC) curve was used to predict the value of NLR and serum TgAb for cervical lymph node metastasis. Results Tumor diameter, uric acid, urea nitrogen, creatinine, total bilirubin, NLR and serum TgAb were significantly higher in the metastatic group than in the non-metastatic group (P < 0.05). There was no statistically significant difference between the two groups in gender, age, history of hypertension, history of coronary heart disease, history of diabetes, combined goiter, number of tumors, cholesterol, triglyceride, high density lipoprotein and low density lipoprotein (P > 0.05). Logistic regression model showed that elevated NLR and serum TgAb levels were independent risk factors for cervical lymph node metastasis in patients with papillary thyroid carcinoma (P < 0.05). The clinical value of NLR combined with serum TgAb [AUC = 0.874, 95%CI (0.816 - 0.932), sensitivity = 89.76%, specificity = 90.58%] in predicting cervical lymph node metastasis was significantly better than that of NLR [AUC = 0.753, 95%CI (0.673 - 0.833), sensitivity = 76.53%, specificity = 79.12%] and serum TgAb [AUC = 0.796, 95%CI (0.724 - 0.869), sensitivity = 80.47%, specificity = 83.91%] alone. Conclusion Abnormally elevated levels of NLR and serum TgAb levels are closely related to the occurrence of cervical lymph node metastasis in patients with papillary thyroid carcinoma. Early combined detection is helpful to predict the risk of cervical lymph node metastasis in patients with papillary thyroid carcinoma, so as to provide reference for clinical development of targeted intervention programs.
[Key words] Neutrophil to lymphocyte ratio; Thyroglobulin antibody; Papillary thyroid carcinoma; Cervical lymph node metastasis
2018年甲状腺癌的新发病例数约为57万人,占恶性肿瘤新发病例数的3.1%,死亡人數约为4万人,占恶性肿瘤死亡病例数的0.4%[1]。甲状腺癌可分为乳头状癌、滤泡状癌、髓样癌和未分化癌,其中乳头状癌约占85%,并且预后最好[2]。但是甲状腺乳头状癌依然存在肿瘤转移的风险,导致患者病情恶化[3]。根据文献报道,甲状腺乳头状癌的颈部淋巴结转移率高达80%,如何对颈部淋巴结转移进行诊断并据此拟定后续术中淋巴结清扫手术方案是目前的研究重点之一[4]。炎性相关指标中性粒细胞/淋巴细胞比值(NLR)与乳腺癌和肺癌的发生发展密切相关,与肿瘤转移和复发存在一定相关性,并且NLR值增高与肿瘤患者的不良预后密切相关[5-6]。甲状腺球蛋白抗体(TgAb)常见于甲状腺疾病患者的血清中,与甲状腺病变的发生密切相关[7]。在甲状腺癌患者中血清TgAb水平明显升高,是甲状腺癌的潜在肿瘤标志物分子[8]。但是目前对于NLR和TgAb在甲状腺乳头状癌颈部淋巴结转移中的相关研究较少,本研究通过检测NLR值和血清TgAb水平,旨在探讨其在甲状腺乳头状癌患者中的水平及其与颈部淋巴结转移的关系,现报道如下:
1 资料与方法
1.1 一般资料
选择2017年1月~2019年9月淮南市第一人民医院诊治的甲状腺乳头状癌患者135例作为研究对象,纳入标准:①经病理学诊断确诊为甲状腺乳头状癌;②临床资料完整;③患者接受腺叶全切手术,辅之以淋巴结清扫术。排除标准:①合并其他类型肿瘤;②存在自身免疫性疾病;③存在肝肾功能损伤;④复发患者;⑤非首次接受手术治疗患者;⑥存在全身性感染性疾病。根据患者是否发生颈部淋巴结转移将其分为未转移组(72例)和转移组(63例)。患者入院后与院方签署知情同意书,临床研究开展经过医院医学伦理委员会同意。
1.2 生理生化指标检测
采集患者的空腹静脉血5 mL,8000 r/min(离心半径12.5 cm)离心20 min后将上清液转移至另一洁净离心管中,-80℃冻存,待所有入组患者的血清样本采集结束后统一进行检测。采用血细胞自动分析仪(美国贝克曼库尔特科技有限公司,型号:LH750)检测患者的NLR值。采用全自动生化分析仪(美国贝克曼库尔特科技有限公司,型号:AU5800)检测患者尿酸、尿素氮、肌酐、总胆红素、胆固醇、三酰甘油、高密度脂蛋白和低密度脂蛋白等指标,使用配套检测试剂盒进行生化指标检测,实验操作严格按照试剂盒说明书以及仪器操作规范进行。血清TgAb检测采用酶联免疫吸附法,使用TgAb检测试剂盒(上海晶抗生物工程有限公司,货号:JK-6130,规格:96T)进行检测,实验操作严格按照试剂盒说明书进行。
1.3 观察指标
比较两组患者的临床资料,包括性别、年龄、高血压史、冠心病史、糖尿病史、合并甲状腺肿情况、肿瘤直径和肿瘤数量,以及两组患者的生理生化指标,包括尿酸、尿素氮、肌酐、总胆红素、胆固醇、三酰甘油、高密度脂蛋白、低密度脂蛋白、NLR和TgAb。以甲状腺乳头状瘤患者的NLR和TgAb均值作为logistic回归分析的临界值,分别为NLR=2.99和TgAb=10.75 ng/L。
1.4 统计学方法
采用SPSS 20.0对所得数据进行统计学分析,计量资料以均数±标准差(x±s)表示,采用独立样本t检验,计数资料以百分率表示,采用χ2检验。应用logistic回归模型分析发生颈部淋巴结转移的影响因素,受试者工作特征曲线(ROC)评估NLR和血清TgAb对发生颈部淋巴结转移的预测价值。以P < 0.05为差异有统计学意义。
2 结果
2.1 甲状腺乳头状癌患者的临床资料及生理生化指标与颈部淋巴结转移的关系
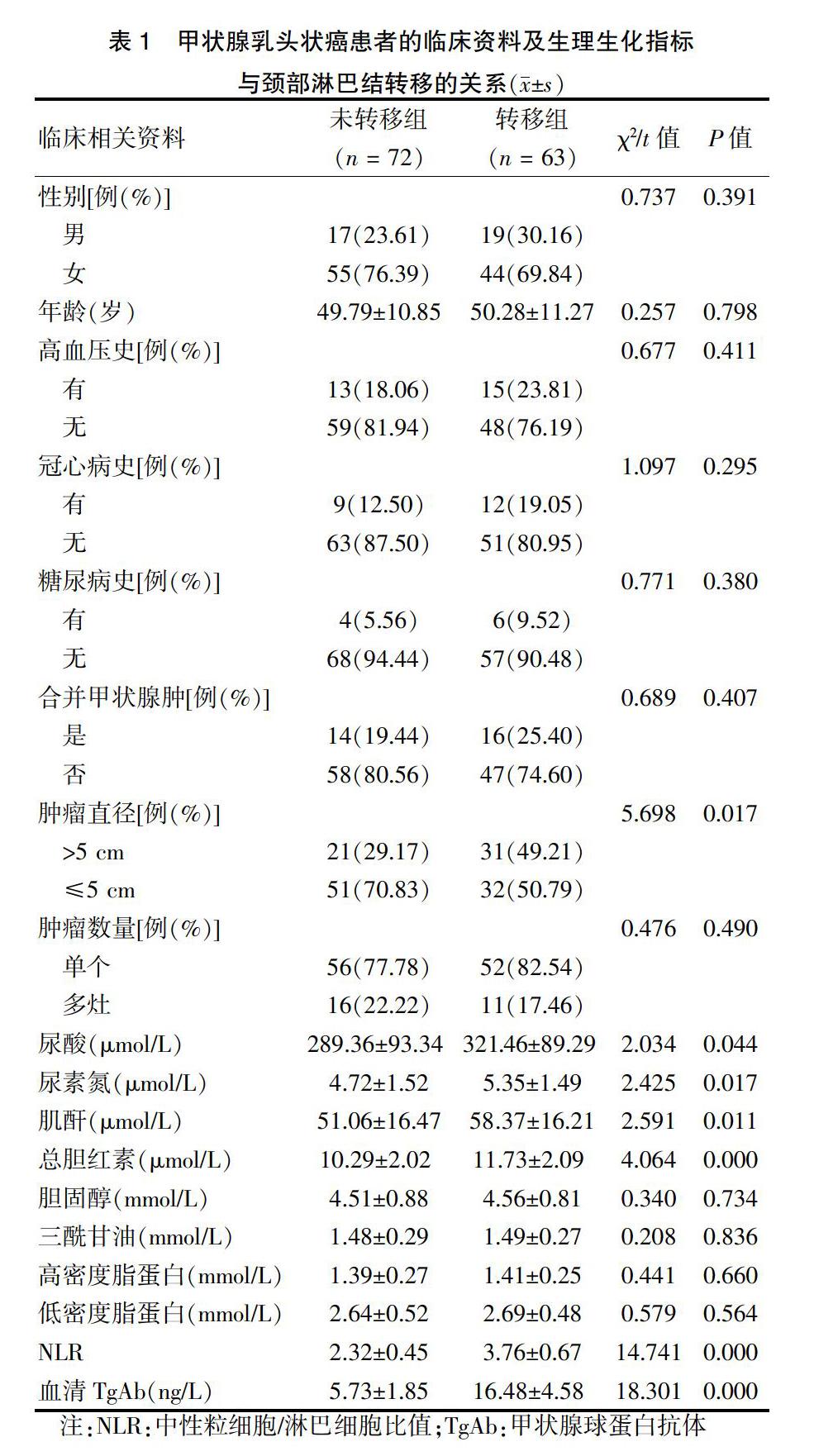
转移组的肿瘤直径、尿酸、尿素氮、肌酐、总胆红素、NLR和血清TgAb高于未转移组,差异有统计学意义(P < 0.05)。两组患者性别、年龄、高血压史、冠心病史、糖尿病史、合并甲状腺肿、肿瘤数量、胆固醇、三酰甘油、高密度脂蛋白和低密度脂蛋白比较,差异无统计学意义(P > 0.05)。见表1。
表1 甲状腺乳头状癌患者的临床资料及生理生化指标
与颈部淋巴结转移的关系(x±s)
注:NLR:中性粒细胞/淋巴细胞比值;TgAb:甲状腺球蛋白抗体
2.2 甲状腺乳头状癌患者颈部淋巴结转移影响因素的logistic回归分析
建立非条件logistic回归模型,以颈部淋巴结转移为因变量,赋值有颈部淋巴结转移=1,无颈部淋巴结转移=0。初步选择肿瘤直径、尿酸水平、尿素氮水平、肌酐水平、总胆红素水平、NLR值和血清TgAb水平作为自变量,经logistic回归分析可知:NLR和血清TgAb水平升高是甲状腺乳头状癌患者颈部淋巴结转移的独立危险因素(P < 0.05)。见表2。
2.3 NLR比值和血清TgAb水平对颈部淋巴结转移的预测价值
采用ROC曲线下面积评估NLR比值和血清TgAb水平对颈部淋巴结转移的预测价值,结果显示NLR的AUC为0.753,95%CI(0.673~0.833),最佳截断值为2.91,灵敏度、特异度分别为76.53%、79.12%;血清TgAb的AUC为0.796,95%CI(0.724~0.869),最佳截断值为10.48 ng/L,灵敏度、特异度分别为80.47%、83.91%;NLR联合血清TgAb预测颈部淋巴结转移的AUC为0.874,95%CI(0.816~0.932),灵敏度、特异度分别为89.76%、90.58%。见图1。
3 讨论
甲状腺乳头状癌的手术治疗主要包括淋巴结清扫和甲状腺切除两个部分,对于颈部淋巴结存在转移的患者可行治疗性淋巴结清扫,在淋巴结转移灶存在残留的情况下可以进一步进行预防性淋巴结清扫,防止甲状腺乳头状癌复发[9-10]。目前临床上虽然能够以颈部彩超的结果作为是否行预防性淋巴结清扫的标准,但是颈部彩超存在诊断敏感性和特异性差等局限性,使得该标准存在较大的不合理性[11]。因此寻求与颈部淋巴结转移密切相关的生物标志物分子对预防性淋巴结清扫具有一定的临床指导价值。
甲状腺乳头状癌容易发生颈部淋巴结转移,其中肿瘤细胞的上皮-间质转化以及肿瘤血管生成是引起肿瘤转移的主要因素[12]。NLR是反映机体免疫功能和炎性反应的重要指标,在卵巢癌和直肠癌患者中均能够检测到NLR值的提高,与肿瘤患者的肿瘤转移和不良预后密切相关[13-14]。NLR值升高与中性粒细胞数增加密切相关,而肿瘤相关中性粒细胞在肿瘤转移中发挥重要作用,如Wang等[15]的研究发现中性粒细胞能够产生并分泌明胶酶,明胶酶作用于胰腺癌细胞的胞外基质蛋白并催化其降解,导致细胞的黏附能力下降,促进肿瘤细胞转移。同时,Stojkov等[16]的研究结果表明来源于中性粒细胞的氧自由基能够抑制淋巴细胞的细胞毒性,同时抑制肿瘤细胞外基质的黏附促进功能,导致肿瘤细胞转移和復发。本研究结果发现在发生颈部淋巴结转移的患者当中NLR值明显升高,提示患者体内存在一定程度的免疫机能紊乱的炎性反应,并且提示肿瘤相关中性粒细胞存在异常增殖的现象。进一步通过logistic回归分析发现NLR是颈部淋巴结转移的独立危险因素,NLR值每上升1,颈部淋巴结转移发生风险增加2.333倍,推测其原因,可能是因为随着甲状腺乳头状癌的病情发展,患者体内的肿瘤相关中性粒细胞异常增殖,导致患者NLR升高。肿瘤相关中性粒细胞产生大量的明胶酶和氧自由基并作用于肿瘤细胞的胞外基质,导致胞外基质降解和胞外基质的细胞间黏附功能下降,进而促进甲状腺乳头状癌细胞的颈部淋巴结转移[17-18]。
TgAb是自身免疫性甲状腺疾病的标志物,在甲状腺癌患者当中血清TgAb水平普遍升高,并且与甲状腺癌患者的不良预后密切相关[19]。同时,TgAb在甲状腺癌细胞的增殖、迁移和干细胞特性调控过程中均发挥重要作用。如Shen等[20]的研究表明TgAb能够上调甲状腺癌细胞中基质金属蛋白酶9(MMP9)和MMP13蛋白的表达,MMP9和MMP13属于金属蛋白酶家族,能够促进胞外基质的降解,二者表达量上调会促进肿瘤细胞外基质的降解,从而促进甲状腺癌细胞转移。本研究发现在发生颈部淋巴结转移的患者当中血清TgAb水平明显升高,提示在甲状腺乳头状癌发病过程中存在自身免疫性反应,肿瘤发病过程中产生的大量Tg蛋白被自身产生的TgAb抗体中和。进一步通过logistic回归分析发现血清TgAb是颈部淋巴结转移的独立危险因素,血清TgAb水平每上升1 ng/L,颈部淋巴结转移发生风险增加2.995倍,推测其原因,可能是因为TgAb能够上调MMP9和MMP13等金属蛋白酶的表达,导致细胞外基质被大量分解,造成肿瘤细胞的黏附能力下降,导致甲状腺乳头状癌细胞的转移。同时TgAb能够促进细胞外信号调节激酶2(ERK2)和丝裂原激活的蛋白激酶(MAPK)等肿瘤血管新生相关信号通路的活化,使得肿瘤血管大量生成,甲状腺乳头状癌细胞通过新生血管进行转移[21]。
结果还显示,NLR联合血清TgAb预测甲状腺乳头状癌患者发生颈部淋巴结转移的临床价值较高,ROC曲线下面积为0.874,灵敏度、特异度分别为89.76%、90.58%,明显优于NLR、血清TgAb单独预测的价值。提示早期检测甲状腺乳头状癌患者NLR、血清TgAb水平,可作为临床预测颈部淋巴结转移发生风险的重要生化标志物。
综上所述,NLR和血清TgAb水平异常升高均与甲状腺乳头状癌患者颈部淋巴结转移的发生密切相关,早期联合检测有助于预测甲状腺乳头状癌患者颈部淋巴结转移的发生风险,从而为临床制订针对性干预方案提供参考。
[参考文献]
[1] Bray F,Ferlay J,Soerjomataram I,et al. Global cancer statistics 2018:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries [J]. CA Cancer J Clin,2018,68(6):394-424.
[2] Seib CD,Sosa JA. Evolving Understanding of the Epidemiology of Thyroid Cancer [J]. Endocrinol Metab Clin North Am,2019,48(1):23-35.
[3] Roman BR,Morris LG,Davies L. The thyroid cancer epidemic,2017 perspective [J]. Curr Opin Endocrinol Diabetes Obes,2017,24(5):332-336.
[4] Agrawal N,Evasovich MR,Kandil E,et al. Indications and extent of central neck dissection for papillary thyroid cancer: An American Head and Neck Society Consensus Statement [J]. Head Neck,2017,39(7):1269-1279.
[5] Kang KH,Efird JT,Sharma N,et al. Prognostic potential of neutrophil-to-lymphocyte ratio and lymphocyte nadir in stage Ⅲ non-small-cell lung cancer [J]. Future Oncol,2017,13(16):1405-1414.
[6] Lee J,Kim DM,Lee A. Prognostic Role and Clinical Association of Tumor-Infiltrating Lymphocyte,Programmed Death Ligand-1 Expression with Neutrophil-Lymphocyte Ratio in Locally Advanced Triple-Negative Breast Cancer [J]. Cancer Res Treat,2019,51(2):649-663.
[7] Esfandiari NH,Papaleontiou M. Biochemical Testing in Thyroid Disorders [J]. Endocrinol Metab Clin North Am,2017,46(3):631-648.
[8] Jo K,Lim DJ. Clinical implications of anti-thyroglobulin antibody measurement before surgery in thyroid cancer [J]. Korean J Intern Med,2018,33(6):1050-1057.
[9] Miccoli P,Bakkar S. Surgical management of papillary thyroid carcinoma:an overview [J]. Updates Surg,2017,69(2):145-150.
[10] Roman BR,Randolph GW,Kamani D. Prognostic Role and Clinical Association of Tumor-Infiltrating Lymphocyte,Programmed Death LiganConventional Thyroidectomy in the Treatment of Primary Thyroid Cancer [J]. Endocrinol Metab Clin North Am,2019,48(1):125-141.
[11] Chua WY,Langer JE,Jones LP. Surveillance Neck Sonography After Thyroidectomy for Papillary Thyroid Carcinoma:Pitfalls in the Diagnosis of Locally Recurrent and Metastatic Disease [J]. J Ultrasound Med,2017,36(7):1511-1530.
[12] Wang T,Xu H,Qi M,et al. miRNA dysregulation and the risk of metastasis and invasion in papillary thyroid cancer: a systematic review and meta-analysis [J]. Oncotarget,2017,9(4):5473-5479.
[13] Zhou M,Li L,Wang X,et al. Neutrophil-to-Lymphocyte Ratio and Platelet Count Predict Long-Term Outcome of Stage ⅢC Epithelial Ovarian Cancer [J]. Cell Physiol Biochem,2018,46(1):178-186.
[14] 陈梅,宋春兰,成怡冰.外周血Treg、Th17、血乳酸、NLR值的变化与脓毒症患儿预后的关系[J].中华医院感染学杂志,2020,30(2):250-253.
[15] Wang Y,Jia M,Yan X,et al. Increased neutrophil gelatinase-associated lipocalin (NGAL) promotes airway remodelling in chronic obstructive pulmonary disease [J]. Clin Sci(Lond),2017,131(11):1147-1159.
[16] Stojkov D,Amini P,Oberson K,et al. ROS and glutathionylation balance cytoskeletal dynamics in neutrophil extracellular trap formation [J]. J Cell Biol,2017,216(12):4073-4090.
[17] Lavender N,Yang J,Chen SC,et al. The Yin/Yan of CCL2:a minor role in neutrophil anti-tumor activity in vitro but a major role on the outgrowth of metastatic breast cancer lesions in the lung in vivo [J]. BMC Cancer,2017,17(1):88.
[18] Kumar S,Gupta E,Kaushik S,et al. Neutrophil Extracellular Traps:Formation and Involvement in Disease Progression [J]. Iran J Allergy Asthma Immunol,2018,17(3):208-220.
[19] 黄上林,付利军,邱新光.血清抗甲状腺球蛋白抗体水平与罹患甲状腺癌风险大小的相关性分析[J].中华内分泌外科杂志,2019,13(1):9-12.
[20] Shen CT,Zhang XY,Qiu ZL,et al. Thyroid autoimmune antibodies in patients with papillary thyroid carcinoma: a double-edged sword [J]. Endocrine,2017,58(1):176-183.
[21] Liang Z,Xie WJ,Zhao M,et al. DDR2 facilitates papillary thyroid carcinoma epithelial mesenchymal transition by activating ERK2/Snail1 pathway [J]. Oncol Lett,2017, 14(6):8114-8121.
(收稿日期:2019-12-26 本文編辑:顾家毓)

