X-CONE经脐单通道腹腔镜胆囊切除术治疗胆囊疾病的疗效
陈斯聪?缪丁丁
【摘要】目的 探讨X-CONE经脐单通道腹腔镜胆囊切除术治疗胆囊疾病的疗效。方法 回顾性分析402例接受腹腔镜胆囊切除术患者的临床资料,根据手术方式将其分为单孔组(X-CONE经脐单通道腹腔镜胆囊切除术)181例及传统组(三孔法腹腔镜胆囊切除术)221例,比较2组的手术时间、术中出血量、术后住院时间、并发症、疼痛评分及住院总费用等指标。结果 402例患者均順利完成腹腔镜胆囊切除术,无中转开腹者。单孔组181例中98.3%(178/181)成功完成X-CONE经脐单通道腹腔镜胆囊切除术,3例中转接受传统三孔法腹腔镜胆囊切除术。2组患者术中出血量比较差异无统计学意义(P > 0.05)。单孔组手术时间长于传统组(P < 0.05),但其术后住院时间、胆囊窝积液、住院总费用均优于传统组(P均 < 0.05)。单孔组的术后第1日疼痛程度弱于传统组(P < 0.05)。2组均无伤口感染、胆漏、腹腔出血、胆道损伤等并发症。术后随访12 ~ 24个月,无患者出现脐疝、胆道狭窄等并发症,所有患者对美容效果均满意。结论 X-CONE经脐单通道腹腔镜胆囊切除术治疗胆囊疾病安全可靠,患者恢复快,费用少。
【关键词】X-CONE;经脐单通道腹腔镜手术;胆囊切除术
Surgical efficacy of X-CONE trans-umbilical single-port laparoscopic cholecystectomy in treatment of gallbladder diseases Chen Sicong, Miao Dingding. Department of Hepatobiliary and Pancreatic Surgery, Shenzhen Nanshan Peoples Hospital, Shenzhen 518052, China
Corresponding author, Chen Sicong, E-mail: firelake@ foxmail. com
【Abstract】Objective To evaluate the surgical efficacy of X-CONE trans-umbilical single-port laparoscopic cholecystectomy in the treatment of gallbladder diseases. Methods Clinical data of 402 patients undergoing laparoscopic cholecystectomy were retrospectively analyzed. According to the surgical approaches, all patients were divided into the single-port group (n = 181, X-CONE trans-umbilical single-port laparoscopic cholecystectomy) and the traditional group (n = 221, three-port laparoscopic cholecystectomy). The operation time, intraoperative blood loss, length of postoperative hospital stay, postoperative complications, pain score and total hospitalization expenses were statistically compared between two groups. Results All 402 patients successfully completed the laparoscopic cholecystectomy with no switch to open surgery. Of the 181 cases in the single-port group, 178 patients (98.3%) successfully completed the X-CONE trans-umbilical single-port laparoscopic cholecystectomy, and 3 cases were switched to conventional three-port laparoscopic cholecystectomy. Intraoperative blood loss did not significantly differ between two groups (P > 0.05).The operation time in the single-port group was significantly longer than that in the traditional group (P < 0.05).However, the length of postoperative hospital stay, cystic fossa effusion and hospitalization expense in the single-port group were remarkably better compared with those in the traditional group (all P < 0.05). In the single-port group, the severity of pain at postoperative 1 d was considerably less than that in the traditional group (P < 0.05). No wound infection, bile leakage, abdominal hemorrhage, biliary tract injury or other complications were observed in two groups. During postoperative follow-up for 12-24 months, no umbilical hernia, biliary stricture or other complications were found. All patients were satisfied with the cosmetic effect. Conclusion X-CONE trans-umbilical single-port laparoscopic cholecystectomy is a safe and reliable treatment of gallbladder diseases, which yields fast recovery and low cost.
【Key words】X-CONE;Trans-umbilical single-port laparoscopic surgery;Cholecystectomy
微创化是未来外科手术的发展方向,而更小的切口,甚至无瘢痕手术,是外科医师追求的目标。经脐单孔腹腔镜手术由于脐部切口愈合后伤口隐蔽,可以达到近乎无瘢痕的效果,是現阶段较为理想的“无瘢痕”术式[1]。笔者自2015年1月至2017年12月采用STORZ公司X-CONE单孔器械对181例胆囊疾病患者施行经脐单通道腹腔镜胆囊切除术,取得良好效果,现总结手术经验报告如下。
对象与方法
一、研究对象
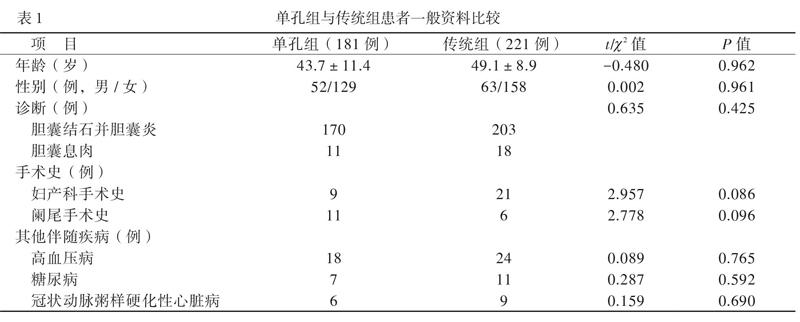
收集402例接受腹腔镜胆囊切除术的胆囊疾病患者的临床资料,其均符合腹腔镜胆囊切除术指征,术前均无上腹部手术史、Mirriz综合征、恶性肿瘤、不能耐受手术等情况。402例术前均签署知情同意书。根据手术方式将其分为单孔组(行X-CONE经脐单通道腹腔镜胆囊切除术)及传统组(行三孔法腹腔镜胆囊切除术)。单孔组181例,其中男52例、女129例,年龄(43.7±11.4)岁,胆囊结石并胆囊炎170例;传统组221例,2组一般资料具可比性,见表1。
二、手术方法
1. 单孔组手术方法
1.1 特殊设备及器械
STORZ腹腔镜成像系统,STORZ X-CONE 单通道入口系统(23020PA),STORZ预弯抓钳(23161OND)及加长分离钳,STORZ 30°内窥镜(26048BSA)。
1.2 单孔组手术步骤
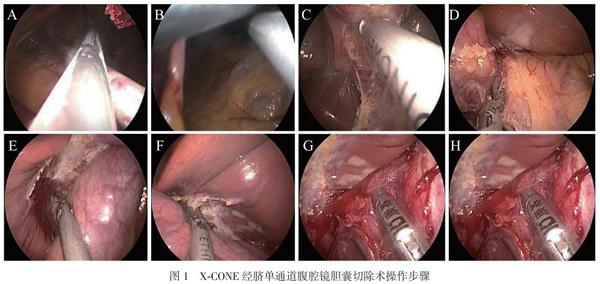
气管插管全身麻醉后,患者取分腿平卧位,脐下做一约2 cm切口,用气腹针穿刺证实其进入腹腔后,充入二氧化碳,维持压力12 mm Hg(1 mm Hg = 0.133 kPa)。采用开放法,经腹白线切开腹膜,置入X-CONE单通道系统。调整患者为头高脚低位。解剖胆囊三角,用弯钳朝头侧牵拉胆囊底部,辨认Rouviere沟及胆总管后解剖胆囊后三角及前三角,用分离钳解剖胆囊动脉及胆囊管,用超声刀直接离断胆囊动脉。剥离胆囊,弯钳朝左上方向牵拉胆囊底部,从胆囊床右侧开始剥离胆囊,弯钳钳夹肝圆韧带向头侧牵拉,从胆囊床左侧剥离,两侧会师后向肝门方向剥离。牵拉胆囊,再次确认胆囊管与胆总管关系无误后,夹闭胆囊管近端后超声刀直接离断。经X-CONE取出胆囊,检查胆囊床无渗血无胆瘘则不放置腹腔引流管,缝合切口腹直肌前鞘及腹膜,皮内缝合切口(图1)。
2.传统组手术步骤
气管插管全身麻醉成功后,分别于脐下、剑突下及右侧腋前线附近建立观察孔,主操作孔及辅助孔,解剖胆囊三角,分离胆囊管及胆囊动脉,分别夹闭,逆行剥离胆囊,再次确认胆囊管及胆囊动脉无误后切断,标本自剑突下取出,不放置腹腔引流管,缝合切口。
三、疗效评价
比较2组的手术时间、术中出血量、术后住院时间、并发症、 疼痛数字评分法(NRS)评分及住院总费用等指标。
四、统计学处理
采用SPSS 24.0进行统计分析。正态分布的计量资料用表示,2组间比较采用独立样本t检验;偏态分布的计量资料采用中位数(下四分位数,上四分位数)表示,2组间比较采用秩和检验。计数资料用例表示,其中无序分类资料组间比较采用χ2检验,等级资料组间比较采用秩和检验。α=0.05。
结果
一、腹腔镜胆囊切除术手术情况
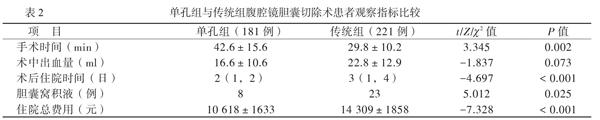
402例患者均顺利完成腹腔镜胆囊切除术,无中转开腹。单孔组患者98.3%(178/181)顺利完成经脐单通道腹腔镜胆囊切除术,3例中转常规三孔法腹腔镜胆囊切除术。2组患者术中出血量比较差异无统计学意义(P > 0.05)。单孔组手术时间长于传统组(P < 0.05),见表2。
二、腹腔镜胆囊切除术后情况
单孔组腹腔镜胆囊切除术后住院时间、胆囊窝积液、住院总费用均优于传统组(P均 < 0.05),见表2。2组均无伤口感染、胆漏、腹腔出血、胆道损伤等并发症。术后随访12 ~ 24个月,所有患者均无脐疝、胆道狭窄等并发症,均对美容效果满意。
三、术后疼痛情况
单孔组的腹腔镜胆囊切除术后第1日疼痛程度弱于传统组,见表3。
讨论
单通道腹腔镜胆囊切除术开展初期普遍采用单切口置入多个普通穿刺器来建立操作通道,使用常规腹腔镜器械完成手术,存在漏气、器械长度不够、左右手器械互相干扰,不能建立有效三角操作等问题,导致操作异常困难[2-3]。此外,由于内窥镜与操作器械同轴平行,视野受限,增加了医源性胆管损伤的风险,这使得大部分术者对该技术持否定态度[4-5]。随着国内外研究者对手术器械的研发改良,近年来一些单通道手术专用器械被推出。简志祥等[6]在国内首先应用X-CONE及其单通道专用器械实施单通道腹腔镜胆囊切除术,初步验证了该手术的可行性及安全性。
STORZ公司X-CONE单通道入口系统由2片金属鞘及橡胶套组成。切口仅需约2 cm,2片金属鞘勾住腹壁且合并后,套上橡胶套即完成单通道手术入口系统的建立,操作便捷。橡胶套由4个5 mm操作孔及1个12 mm操作孔组成,其中12 mm操作孔可插入配套转换器转换成5 mm操作孔,同时配有放气部件,可减轻烟雾干扰。橡胶套有比较大的活动度,配合预弯曲的抓钳和长度50 mm、直径5.5 mm的内窥镜,可有效减少器械的互相干扰,提高了手术成功率。同时X-CONE单孔入口系统经消毒后可重复多次使用,不增加医疗费用。本研究组自2014年起采用STORZ公司X-CONE单通道入口系统及预弯曲抓钳,施行了181例单孔腹腔镜胆囊切除术,98.3%(178/181)顺利完成手术。
减少器械的体内干扰是顺利完成手术的关键。我们的经验是:①把术野分为2个操作视野,即暴露视野与解剖视野。以左手抓钳平面为界,镜头在抓钳平面以上为暴露视野,以下为解剖视野。在暴露视野左手可以随意调整钳夹部位,暴露满意后,镜头退至金属鞘内连同右手器械从左手抓钳平面以下进入解剖视野,此时右手可以解剖胆囊三角而不会与其他器械碰撞;当暴露不满意需调整左手钳夹部位时,镜头应后退至金属鞘内重新进入暴露视野,调整好镜头再次进入解剖视野进行下一步操作。②左手预弯曲抓钳与右手器械上下错开,能较易找到角度进行操作。③使用超声刀解剖胆囊三角腹膜及剥离胆囊。④超声刀慢烧直接离断胆囊动脉,为夹闭胆囊管留出空间。
预防医源性胆道损伤在单通道腹腔镜胆囊切除术中格外重要。我们的经验是:①采用以Rouviere沟为导向的胆囊三角解剖技术;②于胆囊后三角入路;③采用顺逆结合,解剖胆囊三角显露胆囊管后,逆行剥离胆囊,再次确认胆囊管与胆总管关系后再夹闭切断胆囊管[7-9]。
综上所述,遵循一定的解剖原则,掌握特定的手术技巧,单孔腹腔镜胆囊切除手术安全可靠,患者恢复更快,住院费用更低,具有广阔的应用前景。该术式远期疗效的探讨,尚需进行长期随访总结更多经验。
参 考 文 献
[1] Haueter R, Schutz T, Raptis Da, Clavien Pa, Zuber M. Meta-analysis of single-port versus conventional laparoscopic cholecy-stectomy comparing body image and cosmesis. Br J Surg, 2017, 104(9): 1141-1159.
[2] 黃晓斌, 柳晓春, 郑玉华. 经脐单孔腹腔镜手术治疗卵巢良性肿瘤的研究. 新医学, 2015, 46(7): 482-485.
[3] Raakow J, Klein D, Barutcu A G, Biebl M, Pratschke J, Raakow R. Safety and efficiency of single-incision laparoscopic cholecystectomy in obese patients: a case-matched comparative analysis. J Laparoendosc Adv Surg Tech A, 2019, 29(8): 1005-1010.
[4] Casaccia M, Palombo D, Razzore A, Firpo E, Gallo F, Fornaro R. Laparoscopic single-port versus traditional multi-port laparo-scopic cholecystectomy. Jsls, 2019, 23(3). pii: e2018.00102. doi: 10.4293/JSLS.2018.00102.
[5] Arezzo A, Passera R, Forcignano E, Rapetti L, Cirocchi R, Morino M. Single-incision laparoscopic cholecystectomy is responsible for increased adverse events: results of a meta-analysis of randomized controlled trials. Surg Endosc, 2018, 32(9): 3739-3753.
[6] 简志祥, 金浩生. 经脐单孔腹腔镜胆囊切除术——胆囊良性疾病的主流选择. 岭南现代临床外科, 2012, 12(3): 161-162.
[7] 董家鸿, 曾建平. 胆道外科的永恒议题——胆囊切除术胆管损伤的预防. 中国实用外科杂志, 2015, 35(9): 920-922.
[8] 宫路路, 王赈霄, 杨永生, 姜伟栋. Rouviere沟在腹腔镜胆囊切除术中意义的再评估. 腹腔镜外科杂志, 2019, 24(6): 478-480.
[9] 王鹏飞, 孙海军, 李之拓, 于朋涛. 腹腔镜胆囊切除术中有效避免副损伤的手术解剖技巧. 腹腔镜外科杂志, 2018, 23(8): 633-636.
(收稿日期:2019-05-25)
(本文编辑:洪悦民)

