家庭远程监测系统下社区中老年人早晚时段心率差值及高水平静息心率的影响因素分析
刘孟颖,吴升平,茹小娟,孙冬玲
·论著·
·慢病管理·
家庭远程监测系统下社区中老年人早晚时段心率差值及高水平静息心率的影响因素分析
刘孟颖,吴升平,茹小娟,孙冬玲
目的分析家庭远程监测系统下社区中老年人早晚时段心率差值及高水平静息心率的影响因素。方法2013-09-25至2014-01-30,选取北京市石景山区某社区符合纳入标准且使用家庭远程监测系统〔监测06:00~10:00(早晨时段)、16:00~22:00(晚间时段)的心率及血压〕的中老年人78例进行研究,居民签署知情同意书后统一发放Lifesense电子血压仪LS802-4及数据基站LS902,嘱其在家定时测量血压、心率等,通过数据基站LS902自动传输到老年人健康服务支撑平台,共进行3个月的监测。其中早晚时段心率差值=晚间时段平均心率-早晨时段平均心率,并将平均心率≥83次/min定义为高水平静息心率。收集并记录所有配合并完成监测的居民的一般资料〔性别、年龄、体质指数(BMI)、散步时间、吸烟、饮酒〕、用药史〔是否服用钙通道阻滞剂(CCB)〕和疾病史(高血压、高脂血症、冠心病、糖尿病)。采用多元线性回归分析中老年人早晚时段心率差值的影响因素,采用多因素Logistic回归分析高水平静息心率的影响因素。结果服用CCB、患高血压的中老年人早晚时段心率差值高于未服用CCB、未患高血压的中老年人(P<0.05);不同性别、年龄、BMI及是否吸烟、是否饮酒、是否患高脂血症、冠心病、糖尿病的中老年人早晚时段心率差值比较,差异均无统计学意义(P>0.05)。早晚时段心率差值影响因素的多元线性回归分析结果显示,早晚时段心率差值与年龄、BMI、散步时间、服用CCB、早晨时段舒张压有线性回归关系(P<0.05)。单因素Logistic回归分析结果显示,吸烟〔OR=3.889,95%CI(1.133,13.354),P=0.031〕是中老年人早晨时段出现高水平静息心率的影响因素;BMI 24~ kg/m2〔OR=4.444,95%CI(1.427,13.839),P=0.010〕、高脂血症〔OR=3.018,95%CI(1.117,8.156),P=0.029〕是中老年人晚间时段出现高水平静息心率的影响因素。多因素Logistic回归分析结果显示,吸烟〔OR=3.889,95%CI(1.133,13.354),P=0.031〕是中老年人出现早晨时段高水平静息心率的危险因素(P<0.05);晚间时段舒张压〔OR=1.593,95%CI(1.023,2.481),P=0.039〕、高脂血症〔OR=2.953,95%CI(1.058,8.237),P=0.039〕是中老年人出现晚间时段高水平静息心率的危险因素。结论在社区50岁以上的人群中,早晚时段心率差值与BMI、散步时间、服用CCB、早晨时段舒张压呈正相关,与年龄呈负相关;吸烟是早晨时段高水平静息心率的独立影响因素,晚间时段舒张压、高脂血症是晚间时段高水平静息心率的独立影响因素。
中年人;老年人;社区网络;心率
刘孟颖,吴升平,茹小娟,等.家庭远程监测系统下社区中老年人早晚时段心率差值及高水平静息心率的影响因素分析[J].中国全科医学,2016,19(30):3729-3735.[www.chinagp.net]
LIU M Y,WU S P,RU X J,et al.Influencing factors of heart rate difference and high-level resting heart rate between morning and evening periods among the middle-aged and aged people in community under home telemonitoring system[J].Chinese General Practice,2016,19(30):3729-3735.
研究发现,心率与全因死亡和心血管疾病的发生关系密切,全因死亡率与心血管疾病病死率均随心率的升高而递增,且心率升高对一般人群病死率或猝死的影响独立于其他危险因素[1-3]。麦劲壮等[4]队列研究结果发现,心率随着年龄的增加而明显升高,且心率≥90次/min的人群全因死亡风险明显增加。但对不同心率水平及早晚心率差异影响因素的研究较少,本研究观察了北京某社区50岁以上中老年人早晚时段心率变化,并分析早晚时段心率差值和高水平静息心率的影响因素,旨在为有针对性地控制高水平静息心率提供帮助。
1 对象与方法
1.1纳入与排除标准纳入标准:(1)社区常住居民(在该社区至少居住6个月以上);(2)年龄>50岁。排除标准:(1)存在心率异常史者;(2)监测期间,服用β-受体阻滞剂类药物明显影响心率者;(3)存在甲状腺相关疾病病史者;(4)不能坚持测量者;(5)不具备网络使用条件者。
1.2研究对象2013-09-25至2014-01-30,选取北京市石景山区某社区符合纳入标准且使用家庭远程监测系统〔监测06:00~10:00(早晨时段)、16:00~22:00(晚间时
段)的心率及血压〕的中老年人78例进行研究,居民均自愿参与本研究并签署知情同意书。
1.3家庭远程监测系统监测方法居民签署知情同意书后统一发放Lifesense电子血压仪LS802-4及数据基站LS902,嘱其在家定时测量血压、心率等,通过数据基站LS902自动传输到老年人健康服务支撑平台(www.sechealth.cn),共进行3个月的监测。早晚时段心率差值=晚间时段平均心率-早晨时段平均心率。根据心血管疾病中静息心率的相关研究[5-6],本研究将平均心率≥83次/min定义为高水平静息心率。
1.4监测期间观察指标收集并记录所有配合并完成监测的居民的一般资料、用药史和疾病史,其中一般资料包括性别、年龄、体质指数(BMI)、散步时间、吸烟、饮酒;用药史即是否服用钙通道阻滞剂(CCB);疾病史包括高血压、高脂血症、冠心病、糖尿病。其中吸烟定义为≥1支烟/d,持续12个月以上;饮酒定义为饮酒≥1次/周。

2 结果
2.1一般资料、用药史、疾病史、早晚时段心率及血压一般资料:男36例(46.2%),女42例(53.8%);平均年龄(59.9±7.1)岁;平均BMI(25.4±3.0)kg/m2;平均散步时间(1.7±1.3)h/d;吸烟22例(28.2%);饮酒32例(41.0%)。用药史:服用CCB34例(43.6%)。疾病史:高血压45例(57.6%),高脂血症25例(32.0%),冠心病20例(25.6%),糖尿病17例(21.7%)。早晨时段心率及血压:平均心率(76±9)次/min,平均收缩压(127±12)mmHg(1mmHg=0.133kPa),平均舒张压(76±7)mmHg;晚间时段心率及血压:平均心率(79±9)次/min,平均收缩压(126±12)mmHg,平均舒张压(76±6)mmHg。
2.2早晚时段心率差值影响因素的单因素分析服用CCB、患高血压的中老年人早晚时段心率差值高于未服用CCB、未患高血压的中老年人,差异有统计学意义(P<0.05);不同性别、年龄、BMI及是否吸烟、饮酒、患高脂血症、患冠心病、患糖尿病中老年人早晚时段心率差值比较,差异无统计学意义(P>0.05,见表1)。
2.3早晚时段心率差值影响因素的多元线性回归分析将高血压因素转变为早晨时段的血压值进行多元线性回归分析。以早晚时段心率差值为因变量,以性别、年龄、BMI、散步时间、吸烟、饮酒、服用CCB情况、早晨时段收缩压及早晨时段舒张压、冠心病为自变量(赋值见表2),进行多元线性回归分析,结果显示,早晚时段心率差值与年龄、BMI、散步时间、服用CCB、早晨时段舒张压有线性回归关系(P<0.05,见表3)。

Table1Univariateanalysisofheartratedifferencebetweenmorningandeveningperiodsin78middle-agedandagedpeopleincommunity
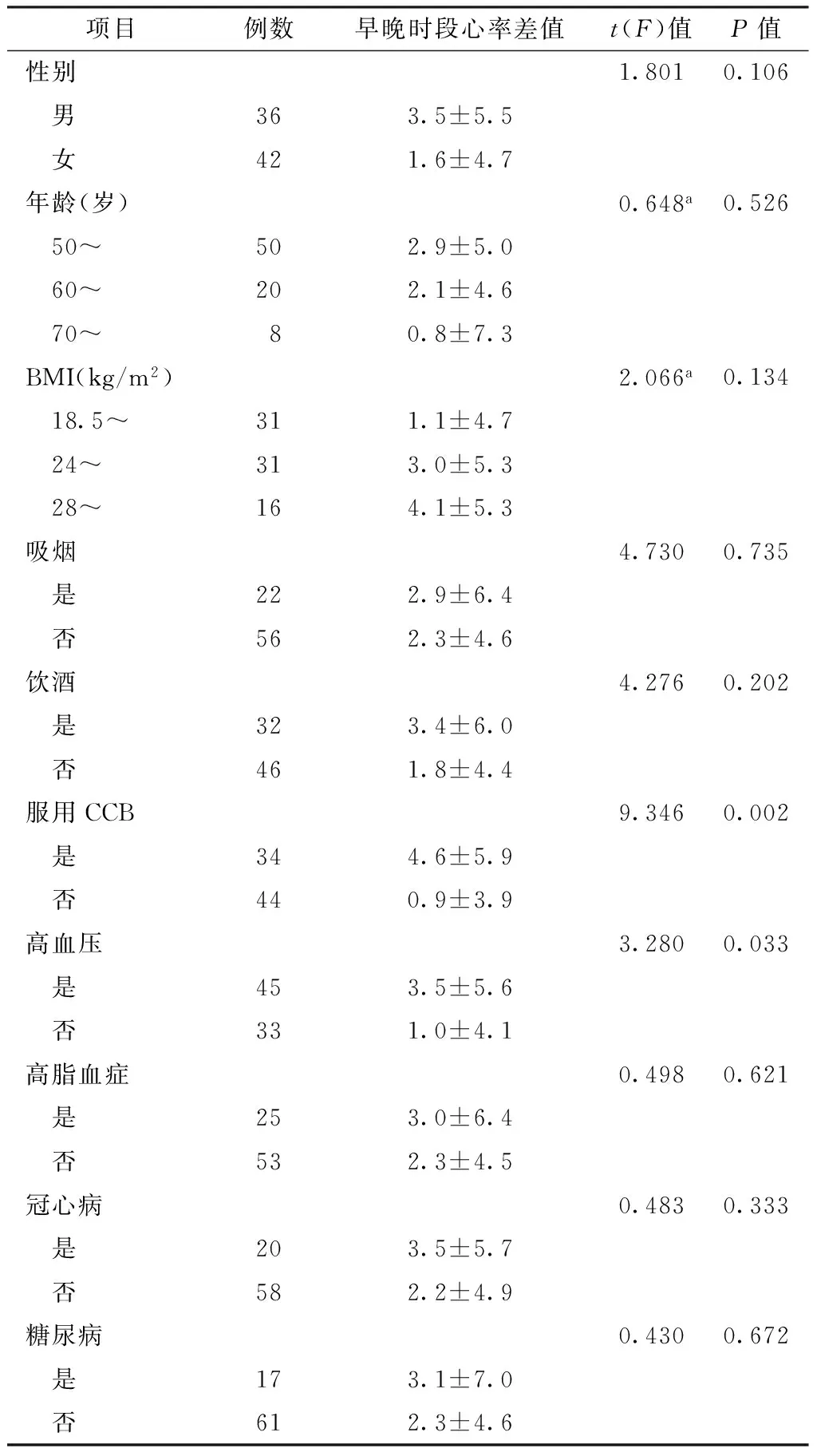
项目例数早晚时段心率差值t(F)值P值性别1.8010.106 男363.5±5.5 女421.6±4.7年龄(岁)0.648a0.526 50~502.9±5.0 60~202.1±4.6 70~80.8±7.3BMI(kg/m2)2.066a0.134 18.5~311.1±4.7 24~313.0±5.3 28~164.1±5.3吸烟4.7300.735 是222.9±6.4 否562.3±4.6饮酒4.2760.202 是323.4±6.0 否461.8±4.4服用CCB9.3460.002 是344.6±5.9 否440.9±3.9高血压3.2800.033 是453.5±5.6 否331.0±4.1高脂血症0.4980.621 是253.0±6.4 否532.3±4.5冠心病0.4830.333 是203.5±5.7 否582.2±4.9糖尿病0.4300.672 是173.1±7.0 否612.3±4.6
注:a为F值;BMI=体质指数,CCB=钙通道阻滞剂
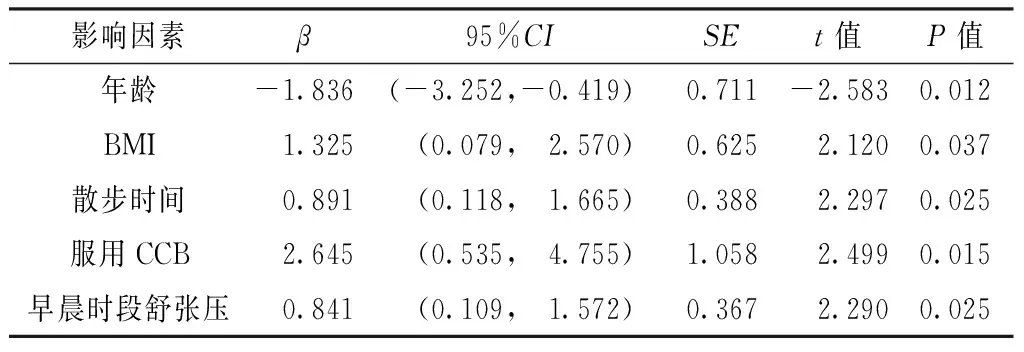
2.4高水平静息心率影响因素的单因素Logistic回归分析以早晨时段、晚间时段高水平静息心率分别为因变量,以性别、年龄、BMI、吸烟、饮酒、服用CCB、高血压、高脂血症、冠心病、糖尿病为自变量(赋值见表4),进行单因素Logistic回归分析,结果显示,吸烟是中老年人早晨时段出现高水平静息心率的影响因素(P<0.05);BMI 24~ kg/m2、高脂血症是中老年人晚间时段出现高水平静息心率的影响因素(P<0.05,见表5)。
表2早晚时段心率差值影响因素的多元线性回归赋值表
Table 2Assignment of multivariate linear regression analysis on influencing factors for heart rate difference between morning and evening periods
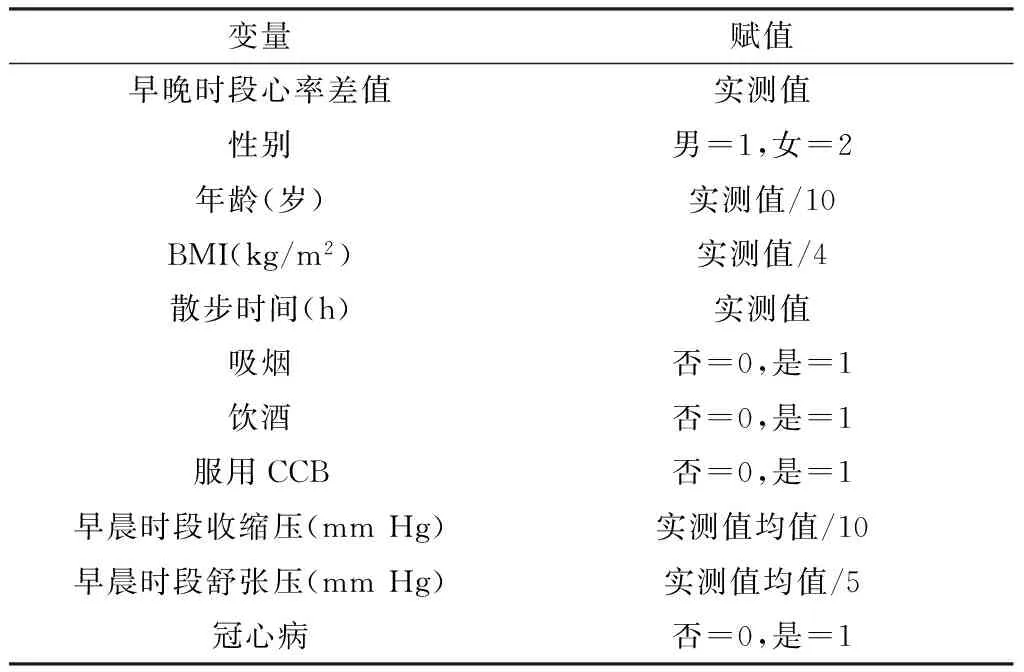
变量赋值早晚时段心率差值实测值性别男=1,女=2年龄(岁)实测值/10BMI(kg/m2)实测值/4散步时间(h)实测值吸烟否=0,是=1饮酒否=0,是=1服用CCB否=0,是=1早晨时段收缩压(mmHg)实测值均值/10早晨时段舒张压(mmHg)实测值均值/5冠心病否=0,是=1
表3早晚时段心率差值影响因素的多元线性回归分析
Table 3Multivariate linear regression analysis on influencing factors for heart rate difference between morning and evening periods
影响因素β95%CISEt值P值年龄-1.836(-3.252,-0.419)0.711-2.5830.012BMI1.325(0.079, 2.570)0.6252.1200.037散步时间0.891(0.118, 1.665)0.3882.2970.025服用CCB2.645(0.535, 4.755)1.0582.4990.015早晨时段舒张压0.841(0.109, 1.572)0.3672.2900.025
表4高水平静息心率影响因素的单因素Logistic回归分析赋值表
Table 4Assignment of univariate Logistic regression analysis on influencing factors for high-level resting heart rate
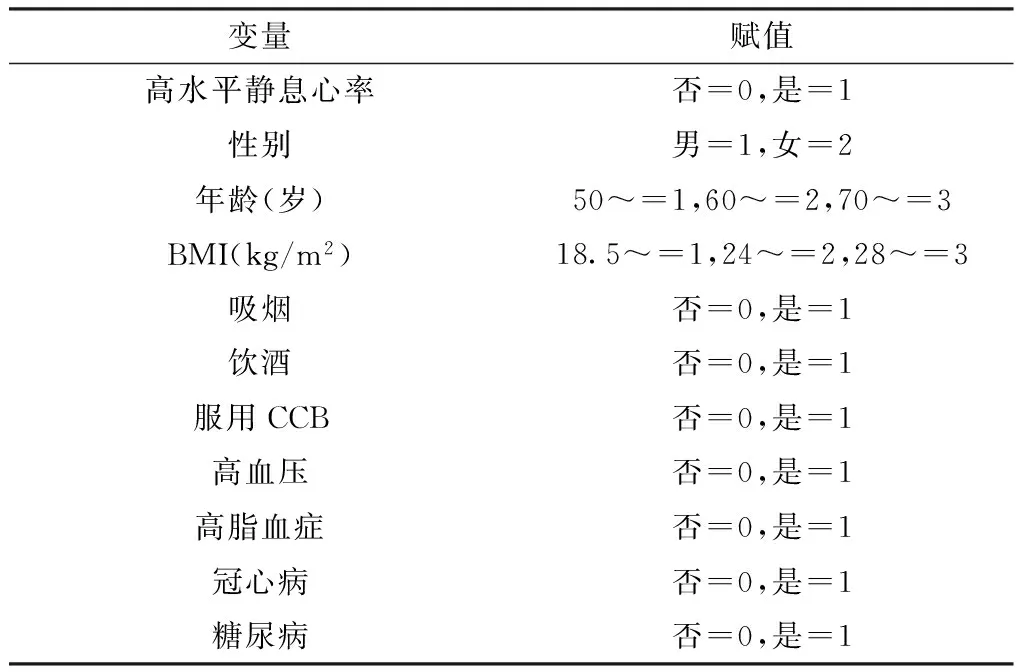
变量赋值高水平静息心率否=0,是=1性别男=1,女=2年龄(岁)50~=1,60~=2,70~=3BMI(kg/m2)18.5~=1,24~=2,28~=3吸烟否=0,是=1饮酒否=0,是=1服用CCB否=0,是=1高血压否=0,是=1高脂血症否=0,是=1冠心病否=0,是=1糖尿病否=0,是=1
2.5高水平静息心率影响因素的多因素Logistic回归分析以早晨时段、晚间时段高水平静息心率分别为因变量,以性别、年龄、BMI、吸烟、饮酒、服用CCB、高血压、高脂血症、冠心病、糖尿病为自变量〔赋值同表4,仅将高血压因素转变为早晚时段血压实测值(赋值:收缩压实测值/10、舒张压实测值/5)进行分析〕,进行多因素Logistic回归分析,结果显示,吸烟是中老年人出现早晨时段高水平静息心率的危险因素(P<0.05);晚间时段舒张压、高脂血症是中老年人出现晚间时段高水平静息心率的危险因素(P<0.05,见表6)。
表5高水平静息心率影响因素的单因素Logistic回归分析
Table 5Univariate Logistic regression analysis on influencing factors for high-level resting heart rate
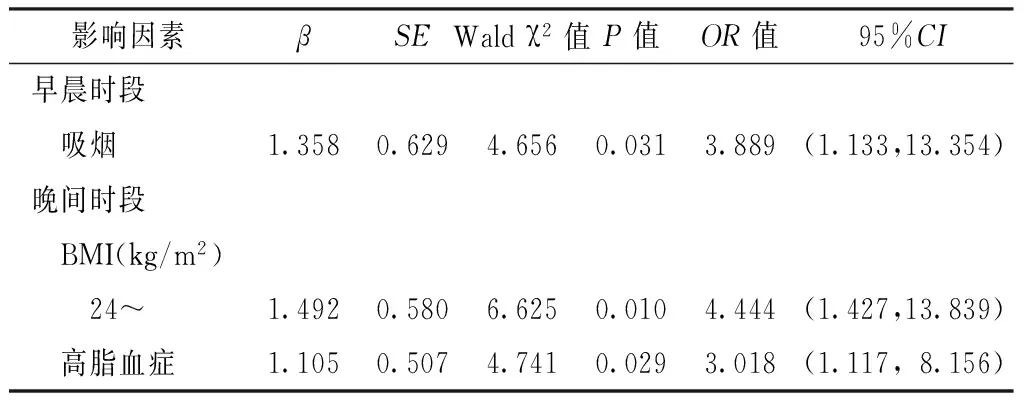
影响因素βSEWaldχ2值P值OR值95%CI早晨时段 吸烟1.3580.6294.6560.0313.889(1.133,13.354)晚间时段 BMI(kg/m2) 24~1.4920.5806.6250.0104.444(1.427,13.839) 高脂血症1.1050.5074.7410.0293.018(1.117,8.156)
表6高水平静息心率影响因素的多因素Logistic回归分析
Table 6Multivariate Logistic regression analysis on influencing factors for high-level resting heart rate
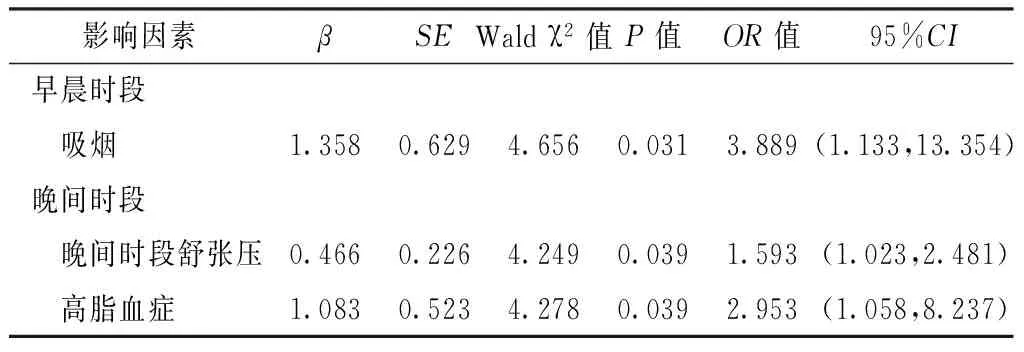
影响因素βSEWaldχ2值P值OR值95%CI早晨时段 吸烟1.3580.6294.6560.0313.889(1.133,13.354)晚间时段 晚间时段舒张压0.4660.2264.2490.0391.593(1.023,2.481) 高脂血症1.0830.5234.2780.0392.953(1.058,8.237)
3 讨论
随着高水平静息心率与人群全因死亡风险增高相关的证据越来越多[1-6],了解静息心率变化的相关因素及全面了解高水平静息心率的影响因素十分必要。在静息心率的相关研究中,PIWOSKA等[7]研究提到肥胖、低密度脂蛋白(LDL)、血压、血糖与心率的升高有关;另一项以企业职工体检数据为基础的横断面研究表明,健康生活方式(不吸烟、低盐饮食、经常体育锻炼、BMI<24 kg/m2)有降低静息心率的作用[8];以上研究提示静息心率与一些传统危险因素存在相关性,应引起各界的关注。
本研究结果显示,早晚时段心率差值与年龄、BMI、散步时间、服用CCB、早晨时段舒张压有线性回归关系。关于年龄与早晚时段心率差值的关系,一项对83例25~85岁健康志愿者的心率变异性频谱分析结果显示,随着志愿者年龄的增加,交感、迷走功能均减弱,生理节律波动下降,从而影响心率[9]。有研究显示,肥胖人群的迷走神经张力降低,交感神经活性增加[10],而超重人群也存在交感神经兴奋性增高,分析原因与过多的内脏脂肪有关[11]。本研究结果显示,BMI与早晚时段心率差值呈正相关,与上述研究结果相似。本研究结果显示,早晚时段心率差值与散步时间存在相关性,原因可能为人体在活动中,心率通过心脏自主神经调节而逐渐升高,活动后的恢复期心率逐渐接近静息期[12],白天活动后晚间时段静息心率略高于早晨时段,而经过夜间睡眠后时恢复常态水平。CCB有反射性增加心率的作用,在高水平静息心率影响因素分析中,服用CCB对高水平静息心率无影响;但从早晚时段心率差值影响因素的结果来看,服用CCB与早晚时段心率差值呈正相关,其机制可能与CCB能反射性升高心率,但不会影响心率患者上升到高水平(高水平静息心率患者的心血管事件和死亡风险较高[5-6])有关。在有关24 h血压、心率的研究中,心率在晚间时段处于低水平,早晨时段逐渐升高,中午时段、晚间部分时段的心率高于早晨时段上升初期的心率,心率24 h变化大致类似于血压的杓型状态,血压与心率密切相关[13-14]。
在高水平静息心率的影响因素分析中,吸烟者是非吸烟者早晨时段出现高水平静息心率的3.889倍。吸烟是一个经典的影响心脑血管疾病的危险因素,其能导致心率升高[15]。吸烟会导致机体产生急性心血管毒性作用,表现为血压和心率骤升,分析原因为烟草中烟碱和微量元素镉含量较高,机体吸入后可刺激交感神经兴奋分泌儿茶酚胺[16]。但也有研究显示,大量吸烟对交感神经有抑制作用,血清儿茶酚胺活性显著低于正常人[17]。有研究显示,被动吸烟者24 h平均心率及舒张压均会升高[18],本研究对象部分是夫妻同时入组,被动吸烟者(妻子)的烟草暴露无法控制,而其产生的危害也应引起重视。本研究结果显示,高脂血症患者是非高脂血症患者晚间时段出现高水平静息心率的2.953倍,与相关研究结果[19]类似,但其研究对象为青少年,与本研究对象(中老年人)年龄类似的研究有待进一步检索。本研究结果显示,晚间时段舒张压每升高5 mm Hg,其高水平静息心率的发生风险增加1.593倍,提示中老年人应关注舒张压的水平变化。
本研究未发现样本人群的高水平静息心率与年龄、性别有关,可能与本研究样本人群的平均年龄为59.9岁,65岁以下的研究对象占83.3%,年龄间距窄有关。本研究结果显示,冠心病、糖尿病对高水平静息心率无影响,与相关研究结果存在一定差异[7-8],原因可能是样本人群只限于中老年人,且慢性病患者均在积极用药管理。本研究没有检测具体的血脂、血糖水平,分析时仅纳入疾病状态,未纳入实验室检查资料,因此结果可能存在一定的偏倚。但本研究对象均在一个社区,一定程度上能降低气候环境因素带来的偏倚。
综上所述,在社区进行50岁以上居民的家庭血压远程监测发现,早晚时段心率差值与BMI、散步时间、服用CCB、早晨时段舒张压呈正相关,与年龄呈负相关,且吸烟是早晨时段出现高水平静息心率的独立危险因素,高脂血症、晚间时段舒张压是晚间时段出现高水平静息心率的独立危险因素。吸烟是可干预因素,因此在心脑血管病的预防中,可以通过严格的戒烟及避免二手烟来控制较高的心率水平,同时再次证实了降脂、控制体质量、降压对控制静息心率的重要性。
作者贡献:孙冬玲进行试验设计与实施、质量控制及校审,刘孟颖负责资料收集整理、撰写论文、成文并对文章负责;吴升平、茹小娟进行试验实施、评估。
本文无利益冲突。
[1]GILLMAN M W,KANNEL W B,BELANGER A,et al.Influence of heart rate on mortality among persons with hypertension:the Framingham Study[J].Am Heart J,1993,125(4):1148-1154.
[2]GREENLAND P,DAVIGLUS M L,DYER A R,et al.Resting heart rate is a risk factor for cardiovascular and noncardiovascular mortality:the Chicago Heart Association Detection Project in Industry[J].Am J Epidemiol,1999,149(9):853-862.
[3]SECCARECCIA F,PANNOZZO F,DIMA F,et al.Heart rate as a predictor of mortality:the MATISS project [J].Am J Public,2001,91(8):1258-1263.
[4]麦劲壮,赵连成,刘小清,等.心率与全因死亡及冠心病事件关系的队列人群研究[J].中华心血管病杂志,2009,37(8):750-753.
MAI J Z,ZHAO L C,LIU X Q,et al.Association between heart rate and all-cause death and coronary event in the Chinese cohort:16 years follow up results[J].Chinese Journal of Cardiology,2009,37(8):750-753.
[5]FOX K,BORER J S,CAMM A J,et al.Resting heart rate in cardiovascular disease[J].J Am Coll Cardiol,2007,50(9):823-830.
[6]DIAZ A,BOURASSA M G,GUERTIN M C,et al.Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease[J].Eur Heart J,2005,26(10):967-974.
[8]高竞生,梁欣,施继红,等.理想心血管健康行为和因素对静息心率的影响[J].中华心血管病杂志,2014,42(9):778-783.
GAO J S,LIANG X,SHI J H,et al.Impact of ideal cardiovascular health behaviors and factors on resting heart rate in individuals without cardiovascular diseases[J].Chinese Journal of Cardiology,2014,42( 9 ):778-783.
[9]PICCIRILLO G,FIMOGNARI F L,VIOLA E,et al.Age-adjusted normal confidence intervals for heart rate variability in healthy subjects during head-up tilt[J].Int J Cardiol,1995,50(2):117-124.
[10]KARASON K,MØLGAARD H,WIKSTRAND J,et al.Heart rate variability in obesity and the effect of weight loss[J].Am J Cardiol,1999,83(8):1242-1247.
[11]CHINTALA K K,KRISHNA B H,N M R.Heart rate variability in overweight health care students:correlation with visceral fat[J].J Clin Diagn Res,2015,9(1):CC06-08.
[12]ARAI Y,SAUL J P,ALBRECHT P,et al.Modulation of cardiac autonomic activity during and immediately after exercise[J].Am J Physiol,1989,256(1):H132-141.
[13]DEGAUTE J P,VAN DE BORNE P,LINKOWSKI P,et al.Quantitative analysis of the 24-hour blood pressure and heart rate patterns in young men[J].Hypertension,1991,18(2):199-210.
[14]KOROBOKI E,MANIOS E,PSALTOPOULOU T,et al.Circadian variation of blood pressure and heart rate in normotensives,white-coat,masked,treated and untreated hypertensives[J].Hellenic Journal of Cardiology,2012,53(6):432-438.
[15]AL-SAFI S A.Does smoking affect blood pressure and heart rate?[J].Eur J Cardiovasc Nurs,2005,4(4):286-289.
[16]杨春.吸烟对血压心率心电图即刻效应的研究[J].环境与健康杂志,2003,20(6):347-348.
YANG C.Study on the Immediate effects of smoking on blood pressure,heart rate and electrocardiogram in smokers[J].Journal of Environment and Health,2003,20(6):347-348.
[17]叶康平.吸烟对人血清多巴胺-β-羟化酶活性双相影响[J].国外医学卫生学分册,1993(2):27.
[18]赵菁,何飞,胡大一,等.被动吸烟人群特征及对心率变异性、心率和血压的影响[J].中华心血管病杂志,2013,41(5):422-426.
ZHAO J,HE F,HU D Y,et al.Population characteristics and impact on heart rate variability,heart rate and blood pressure of passive smoking[J].Chinese Journal of Cardiology,2013,41(5):422-426.
[19]FREITAS JúNIOR I F,MONTEIRO P A,SILVEIRA L S,et al.Resting heart rate as a predictor of metabolic dysfunctions in obese children and adolescents[J].BMC Pediatrics,2012,12(1):5.
(本文编辑:毛亚敏)
Influencing Factors of Heart Rate Difference and High-level Resting Heart Rate between Morning and Evening Periods among the Middle-aged and Aged People in Community under Home Telemonitoring System
LIUMeng-ying,WUSheng-ping,RUXiao-juan,SUNDong-ling.
BeijingNeurosurgicalInstitute;BeijingTianTanHospital,CapitalMedicalUniversity;BeijingMunicipalKeyLaboratoryofClinicalEpidemiology,Beijing100050,China
Correspondingauthor:SUNDong-ling,BeijingNeurosurgicalInstitute;BeijingTianTanHosipital,CapitalMedicalUniversity;BeijingMunicipalKeyLaboratoryofClinicalEpidemiology,Beijing100050,China;E-mail:sdongling@sina.com
ObjectiveTo analyze influencing factors of heart rate difference and high-level resting heart rate between morning and evening periods among the middle-aged and aged people in community under home telemonitoring system.MethodsAccording to inclusion criteria,78 middle-aged and aged people from a community in Shijingshan district of Beijing,who were using home telemonitoring system 〔including heart rate and blood pressure from 06:00-10:00 at a.m.(morning periods) and 16:00-22:00 p.m.(evening periods)〕,were selected from September 25th in 2013 to January 30th in 2014.After the residents signing informed consent form,Lifesense electronic blood pressure meter LS802-4 and data base station LS902 were unified distributed.They were warned to measure their blood pressure and heart rate when at home.The data would automatically transmit to health service support platform of the elderly through the data base station LS902.Three-month monitoring was conducted totally.Heart rate difference between morning and evening periods= average heart rate during evening periods-average heart rate during morning periods,and the average heart rate greater than or equal to 83 times/min was defined as resting heart rate of high level.The general data 〔gender,age,body mass index (BMI),strolling time,smoking,drinking〕,medication history 〔whether taking calcium channel blockers (CCB) or not〕 and diseases history (hypertension,hyperlipidemia,coronary heart disease,diabetes) of residents who cooperated in the investigation and completed the monitoring were collected and recorded.The influencing factors of heart rate difference between morning and evening periods were analyzed by multivariate linear regression analysis and the influencing factors of resting heart rate of high level were analyzed by multiple Logistic regression analysis.ResultsHeart rate difference between morning and evening periods of middle-aged and aged people who had hypertension and took CCB was higher than that of middle-aged and aged people who did not have hypertension and take CCB (P<0.05);there was no significant difference in heart rate difference between morning and evening periods among middle-aged and aged people of different genders,ages,BMI,and whether smoking,drinking,whether developing hyperlipemia,coronary heart disease and diabetes (P>0.05).The results of multiple linear regression analysis of the influencing factors of heart rate difference between morning and evening periods showed that there was a linear regression relationship between heart rate difference between morning and evening periods and age,BMI,strolling time,taking CCB as well as diastolic blood pressure during morning periods (P<0.05).The results of univariate Logistic regression analysis showed that smoking 〔OR=3.889,95%CI(1.133,13.354),P=0.031〕 was the influencing factor of high-level resting heart rate occurring in middle-aged and aged people during morning periods;BMI 24~ kg/m2〔OR=4.444,95%CI(1.427,13.839),P=0.010〕,and hyperlipidemia 〔OR=3.018,95% CI (1.117,8.156),P=0.029〕 were the influencing factors of high-level resting heart rate occurring in middle-aged and aged people during evening periods.The results of multivariate regression analysis showed that smoking 〔OR=3.889,95%CI(1.133,13.354),P=0.031〕 was the influencing factor of high-level resting heart rate occurring in middle-aged and aged people during morning periods;diastolic blood pressure 〔OR=1.593,95%CI(1.023,2.481),P=0.039〕 and hyperlipidemia 〔OR=2.953,95%CI(1.058,8.237),P=0.039〕 were the influencing factors of high-level resting heart rate occurring in middle-aged and aged people during evening periods.ConclusionAmong the elderly aged over 50,heart rate difference between morning and evening periods is positively associated with BMI,strolling time,took CCB and diastolic blood pressure during morning periods,and was negatively related with age;smoking is the independent influencing factors of high-level resting heart rate in morning periods.Diastolic blood pressure and hyperlipidemia are the independent influencing factors of high-level resting heart rate in evening periods.
Middle-aged people;Aged people;Community networks;Heart rate
国家科技支撑计划课题(2012BAH06F06);十二五科技支撑计划项目(2011BAI08B01);北京市神经外科研究所2014年度青年创新基金(计划)(所青年-2014006)
100050北京市,北京市神经外科研究所,首都医科大学附属北京天坛医院,临床流行病学北京市重点实验室
孙冬玲,100050北京市,北京市神经外科研究所,首都医科大学附属北京天坛医院,临床流行病学北京市重点实验室;E-mail:sdongling@sina.com
R 331.31
A
10.3969/j.issn.1007-9572.2016.30.019
2016-03-13;
2016-08-06)