ACEI/ARB类和CCB类降压药对高血压合并急性脑梗死患者血清炎性因子水平和预后的影响
闫云岗,张晓峰,郑小龙
ACEI/ARB类和CCB类降压药对高血压合并急性脑梗死患者血清炎性因子水平和预后的影响
闫云岗1,张晓峰1,郑小龙2
目的:探讨高血压合并急性脑梗死患者使用血管紧张素转换酶抑制剂(ACEI)/血管紧张素受体阻滞剂(ARB)类降压药和钙通道阻滞剂(CCB)类降压药对血清炎性因子水平和预后的影响。方法:急性脑梗死合并高血压患者186例按照急性脑梗死前服用降压药的种类分为A组(入院前已正规服用ACEI/ARB类降压药)67例,B组(入院前已正规服用CCB类降压药)55例,C组(入院前未正规服用降压药)64例;将C组按随机数法随机分为2组,C1组(入院后正规服用ARB类降压药)30例和C2组(入院后正规服用CCB类降压药)34例。分别于入院第3天和第14天检测所有患者血清白细胞介素(IL)-6、肿瘤坏死因子(TNF)-α和和超敏C反应蛋白(hs-CRP)的水平。所有患者入院时及发病90 d时,采用美国国立卫生院脑卒中量表(NIHSS)进行评分。结果:入院第3、14天,A、B组血清IL-6、TNF-α和hs-CRP水平均显著低于C组(P<0.05),A、B组之间各炎性因子差异无统计学意义;入院14天时,A组IL-6水平较B组明显降低,但C1、C2组间各指标差异无统计学意义。入院时,3组的NIHSS评分差异无统计学意义;治疗90 d后,A、B组NIHSS评分低于C组(P<0.05),C1、C2组的NIHSS评分差异无统计学意义。结论:急性脑梗死合并高血压患者,梗死前早期规范服用降压药可能会降低血清多种炎性因子水平,并可能改善患者预后情况。
降压药;高血压;急性脑梗死;炎性因子
急性脑梗死患者伴随局部和全身的炎性反应,炎性因子水平的变化是梗死后炎性反应的结果,同时炎性因子也进一步参与促进脑代谢异常,加速脑梗死的病理变化进程[1-3]。有效降低炎性因子水平对急性脑梗死患者的病情进展和预后均有重要意义[4,5]。长期高血压患者血清炎性因子水平也普遍存在异常,有研究发现血管紧张素转换酶抑制剂(angiotensin converting enzyme inhibitors,ACEI)/血管紧张素受体阻滞剂(angiotensin receptor blockers,ARB)类降压药和钙通道阻滞剂(calcium channel blockers,CCB)类降压药均具有调节高血压患者血清白细胞介素(interleukin,IL)-6、肿瘤坏死因子(tumor necrosis factor,TNF)-α和超敏C反应蛋白(high-sensitivity C-reactive protein,hs-CRP)等炎性因子的作用[6,7]。本研究探讨不同降压药对急性脑梗死合并高血压患者血清相关炎性因子水平及预后的影响。
1 资料与方法
1.1 一般资料
选择2013年9月至2015年2月在我院神经内科住院的符合纳入标准的急性脑梗死合并高血压患者186例。入组标准:年龄45~80岁;高血压病史≥1年;符合脑梗死的诊断标准,并经头颅CT和(或)MRI确诊;本次发作到入院时间≤48 h;意识清楚;高血压治疗方案为ACEI/ARB类或CCB类降压药单药治疗,或未接受正规治疗。排除标准:严重心、肝、肾功能障碍;使用ACEI/ARB类或CCB类以外的降压药;采用多种降压药联合治疗;严重意识障碍。按照入院前有无服用降压药及降压药种类,分为A组(入院前已正规服用ACEI/ARB类降压药)67例,B组(入院前已正规服用CCB类降压药)55例,C组(入院前未正规服用降压药)64例;将C组按随机数法随机分为2组,C1组(入院后正规服用ARB类降压药)30例和C2组(入院后正规服用CCB类降压药)34例。本研究通过我院伦理委员会审核批准,并经患者知情同意。A组男46例,女21例,平均年龄(58.69±11.19)岁;糖尿病10例(14.93%);高血 压 1~5年 36例(53.73%),6~10年 17例(25.37%),≥10年14例(20.90%)。B组男37例,女18例,平均年龄(59.93±12.21)岁;糖尿病7例(12.73%);高血压 1~5年 33例(60.00%),6~10年 12例(21.82%),≥10年10例(18.18%)。C组男41例,女23例,平均年龄(59.23±12.38)岁;糖尿病8例(21.95%);高血压1~5年38例(59.38%),6~10年20例(31.25%),≥10年6例(9.37%)。3组患者年龄、性别、糖尿病患病情况及高血压患病时间等相关基线资料的差异均无统计学意义,具有可比性。
1.2 方法
所有患者根据病情给予抗血小板聚集,调脂,舒张脑血管,去除自由基,维持血糖和电解质平衡及液体支持等基础治疗。A组和B组患者继续住院前降压方案;C1组患者给予缬沙坦80 mg,1次/日,血压控制不佳时最高加量至160 mg;C2组患者给予硝苯地平控释片30 mg,1次/日,血压控制不佳时最高加量至60 mg。分别于入院第3天和第14天检测所有患者血清IL-6、TNF-α和hs-CRP的水平。所有患者入院时及发病90 d时,采用美国国立卫生院脑卒中量表(National Institutes of Health Stroke Scale,NIHSS)进行评分。
1.3 统计学处理
采用SPSS 19.0软件处理数据,计量资料以(χ±s)表示,检验数据正态性及方差齐性,组间比较采用单因素方差分析,组间两两比较采用SNK-q检验;计数资料以率表示,组间比较采用χ2检验,3个样本率两两比较的检验水准,以P<0.025为差异有统计学意义,其余P<0.05为差异有统计学意义。
2 结果
入院第3、14天,A、B组血清IL-6、TNF-α和hs-CRP水平均显著低于C组(P<0.05),A、B组之间各炎性因子差异无统计学意义,见表1。入院14天时,A组IL-6水平较B组明显降低,见表1;但C1、C2组间各指标差异无统计学意义,见表2。
入院时,A、B、C组的NIHSS评分分别为(16.12± 8.27)分、(16.87±7.49)分及(18.55±6.76)分,差异无统计学意义。治疗90 d后,A、B、C组的NIHSS评分分别为(6.83±3.15)分、(7.24±3.48)分及(11.84±4.82)分,A、B组低于C组(P<0.05);A、B、C组治疗前、后NIHSS评分的差值分别为(9.29±4.70)分、(9.63±5.23)分及(6.71±3.48)分,A、B组大于C组(P<0.05)。治疗90 d后C1、C2组的NIHSS评分分别为(11.17±4.32)分及(12.43±5.11)分,差异无统计学意义。
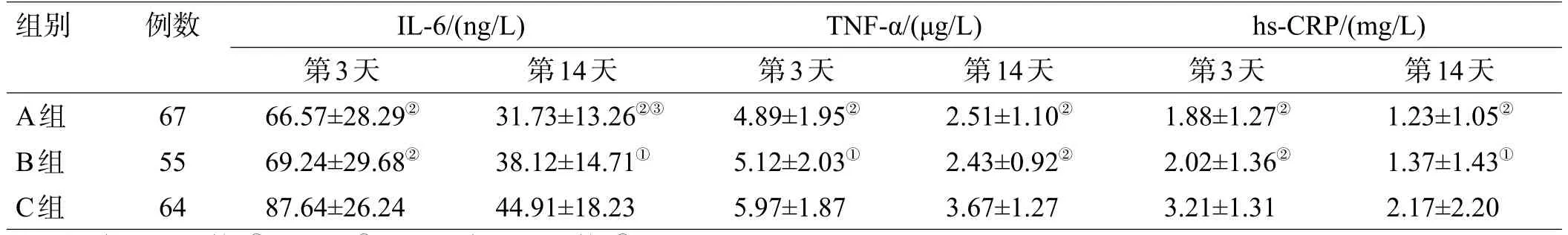
表1 入院第3、14天各组IL-6、TNF-α及hs-CRP水平比较(χ±s)
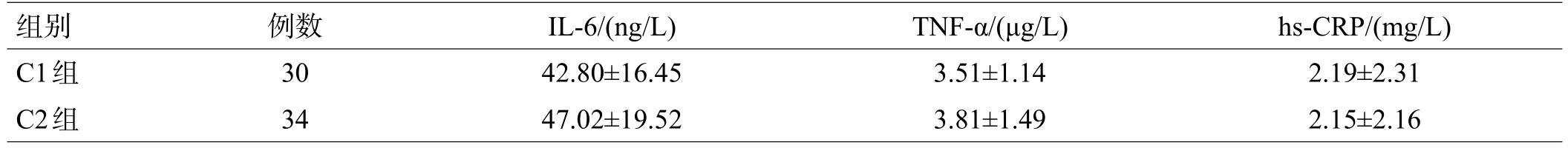
表2 入院第14天C1、C2组IL-6、TNF-α及hs-CRP水平比较(χ±s)
3 讨论
脑梗死后局部炎性反应产生的炎性介质是脑梗死缺血中心区和周围神经元损伤的重要因素[1-5]。除梗死局部产生炎性反应外,脑梗死患者多还伴有全身炎性反应,引起血清中多种炎性因子水平改变,因此,临床中多以血清中主要炎性因子的水平预测评估脑梗死患者的病情进展和预后,指导治疗。
脑梗死后大量脑组织细胞坏死,释放的多种产物刺激患者免疫系统,进而激活单核巨噬细胞和淋巴细胞等免疫细胞,联合脑组织中损伤的胶质细胞和内皮细胞,释放大量IL-6和TNF-α,相互促进,引发多种炎性因子呈“爆发式”增长[3,5]。临床研究证实脑梗死患者急性期血清中IL-6和TNF-α水平显著增高,一般在发病3 d时达到高峰,发病14 d时逐渐趋于正常[8]。hs-CRP不仅是炎性反应的敏感指标,还可通过激活补体,促进活性因子释放等方式参与对脑组织的损伤[4,9]。血清中hs-CRP水平与脑梗死病灶大小及神经功能损害程度均呈正相关,是评价脑梗死损伤程度的重要指标[9]。
近年来研究发现炎性反应与高血压的发生发展密切相关[6]。多种炎性因子在高血压患者体内表达升高,部分炎性因子是高血压发作的独立危险因素[7,10]。其可能的作用机制为:炎性因子可调控一氧化氮的表达,促进血管收缩,加重血压升高;炎性因子可通过参与血管壁重构,维持和加剧高血压病理进程;炎性因子还可通过激活机体的氧化应激反应,降低血管对一氧化氮等舒张血管因子的反应,升高血压[11]。另外,炎性因子不仅作用于血管,还可直接作用于体内多个器官,包括心、脑、肾等,进一步反馈式的加重高血压的病理损害。
研究发现ACEI和ARB类降压药可降低血清中多种炎性因子水平,目前相关机制尚不清楚,可能在于两者可通过抑制血管紧张素Ⅱ表达,从而抑制血管紧张素Ⅱ介导的过氧化物酶体增殖因子活化受体γ(peroxisome proliferator-activated receptor γ,PPARγ)的表达,PPARγ参与多种炎性因子的基因调控,最终影响患者血清炎性因子的水平[12]。CCB类降压药也具有调节炎性因子水平的作用,可能机制在于CCB类降压药可通过抑制烟酰胺腺嘌呤二核苷酸磷酸氧化酶相关调节亚基磷酸化来抑制其活化,抑制活性氧(reactive oxygen species,ROS)产生,从而降低炎性反应[13]。
急性脑梗死合并高血压患者具备慢性炎症和急性炎性反应的双重特点,本研究首次探索不同类型降压药对此类人群血清相关炎性因子的影响,及可能对患者预后情况的影响。结果提示,对于高血压合并急性脑梗死患者,脑梗死发作前规范服用ACEI/ARB类和CCB类降压药均可有效降低脑梗死发作后急性期血清炎性因子水平,能显著提高患者90天基本康复率。本研究还发现长期服用ACEI/ARB类降压药较服用CCB类降压药的患者,除血清IL-6水平更低外,未发现其余指标有显著差异。
总而言之,高血压患者积极规范应用ACEI/ARB类和CCB类降压药,可能通过调节炎性因子的方式改善患者脑梗死发作后的预后情况。
[1]Jafarinaveh HR,Allahtavakoli M,Rezazadeh H,et al.Proinflammatory Cytokines in the Embolic Model of Cerebral Ischemia in Rat[J].Iran J AllergyAsthma Immunol,2014,13:125-130.
[2]张凤莉.脑梗死后炎性因子的动态变化分析[J].中国实用神经疾病杂志,2014,15:57-57.
[3]Kim Y,So HS,Kim JK,et al.Anti-inflammatory effect of oyaksungisan in peripheral blood mononuclear cells from cerebral infarction patients[J].Biol Pharm Bull,2007,30:1037-1041.
[4]Shi SS,Yang WZ,Chen Y,et al.Propofol reduces inflammatory reaction and ischemic brain damage in cerebral ischemia in rats[J].Neurochem Res,2014,39:793-799.
[5]Rong Z,Zailiang Y,Xurong T,et al.Propofol Protects Against Focal Cerebral Ischemia via Inhibition of Microglia-Mediated Proinflammatory Cytokines in a Rat Model of Experimental Stroke[J].PloS One,2013,8: e82729-e82729.
[6]Krishnan SM,Sobey CG,Latz E,et al.IL-1β and IL-18:inflammatory markers or mediators of hypertension[J]?Br J Pharmacol,2014,171: 5589-5602.
[7]Mirhafez SR,Mohebati M,Feiz Disfani M,et al.An Imbalance in Serum Concentrations of Inflammatory and Anti-inflammatory Cytokines in Hypertension[J].JAm Soc Hypertens,2014,8:614-623.
[8]Boeckh-Behrens T,Schubert M,Förschler A,et al.The Impact of Histological Clot Composition in Embolic Stroke[J].Clin Neuroradiol,2016, 26:189-197.
[9]孙卫亚.急性脑梗死患者血清C-反应蛋白及TNF-α浓度变化的临床研究[J].神经损伤与功能重建,2006,1:93-95.
[10]Karaman E,Urhan Kucuk M,Bayramoglu A,et al.Investigation of relationship between IL-6 gene variants and hypertension in Turkish population[J].Cytotechnology,2014,67:947-954..
[11]Wang Q,Zuo XR,Wang YY,et al.Monocrotaline-induced pulmonary arterial hypertension is attenuated by TNF-α antagonists via the suppression of TNF-α expression and NF-κB pathway in rats[J].Vascul Pharmacol,2013,58:71-77.
[12]Qi Y,Zhang J,Cole-Jeffrey CT,et al.Diminazene aceturate enhances ACE2 activity and attenuates ischemia-induced cardiac pathophysiology [J].Hypertension,2013,62:746-752.
[13]Vasigar P,Batmanabane M.Anti-inflammatoryactivity of calciumchannel blocker lercanidipine hydrochloride[J].J Pharmacol Pharmacother, 2013,4:238-242.
(本文编辑:唐颖馨)
Effect of ACEI/ARB and CCB Antihypertensive Drugs on Serum Inflammatory Cytokines and Prognosis in Patients with Acute Cerebral Infarction Combined with Hypertension
YAN Yun-gang1,ZHANGXiao-feng1,ZHENGXiao-long2.1.Department ofNeurology,Xi’anChanganHospital,Xi’an,710008China2.Department of Neurology,LuochuanCountyHospital,Luochuan,727400China
Objective:To observe the effect of ACEI/ARB and CCB antihypertensive drugs on serum inflammatory cytokines and prognosis in hypertensive patients with acute cerebral infarction.Methods:One hundred and eighty-six hypertensive patients with acute cerebral infarction were divided into A group(took ACEI/ARB drugs regularly before the onset of cerebral infarction,n=67),B group(took CCB drugs regularly before the onset of cerebral infarction,n=55)and C group(didn’t take any antihypertensive before the onset of cerebral infarction,n=64).Then patients of C group were randomly divided into C1 group(took ARB drugs regularly after the onset of cerebral infarction,n=30)and C2 group(took CCB drugs regularly after the onset of cerebral infarction, n=34)by random number table.On the 3rd and the 14th day after the onset of cerebral infarction,the serum levels of interleukin(IL)-6,tumor necrosis factor(TNF)-α and high-sensitivity C-reactive protein(hs-CRP)were detected.On the 1st and 90th day,all the patients were evaluated using National Institutes of Health Stroke Scale (NIHSS).Results:The levels of serum IL-6,TNF-α and hs-CRP in group A and B were significantly lower than that in group C on both 3rd and 14th day after onset of cerebral infarction(P<0.05).On the 14th day,the serum level of IL-6 of group A was significantly lower than those in group B(P<0.05).But there was no statistical differences between group C1 and C2.There was no statistical differences among 3 groups about NIHSS scores on the 1st day of onset of cerebral infarction(P>0.05).On the 90th day after therapy the NIHSS scores of group A and B were significantly lower than that of group C while there was no difference between group C1 and C2(P>0.05).Conclusions:Before the onset of cerebral infarction,taking ACEI/ARB or CCB antihypertensive drugs regularly may down-regulate the levels of serum inflammatory cytokines and improve the prognosis of patients with acute cerebral infarction combined with hypertension.
antihypertensive drug;hypertension;acute cerebral infarction;inflammatory cytokines
R741;R743
A DOI 10.16780/j.cnki.sjssgncj.2016.06.005
1.西安市长安医院神经内科西安710008
2.洛川县医院神经内科洛川 727400
2016-04-05
闫云岗yanyungang1972@ 126.com