胰肠吻合方式对胰十二指肠切除术后胰瘘的影响
黄佳飞 张倜 周洪渊 李慧锴 崔云龙 李强
·临床研究与应用·
胰肠吻合方式对胰十二指肠切除术后胰瘘的影响
黄佳飞 张倜 周洪渊 李慧锴 崔云龙 李强
目的:探讨胰肠吻合方式对胰十二指肠切除术后胰瘘的影响。方法:回顾性分析2008年10月至2013年8月天津医科大学肿瘤医院收治的145例术前诊断为壶腹周围肿瘤行胰十二指肠切除术患者的临床资料。对影响术后胰瘘发生的相关因素进行统计分析。结果:本组患者中27例术后发生胰瘘。在4种胰肠吻合方式中,胰管空肠黏膜吻合和Blumgart吻合的胰瘘发生率低,且皆无C级胰瘘。多因素分析应用Logistic回归,结果表明不同的胰肠吻合方式及性别为术后胰瘘发生的独立预后因素。结论:胰肠吻合方式是影响胰十二指肠切除术后胰瘘发生的危险因素。
胰十二指肠切除术 胰肠吻合 胰瘘
术后胰瘘(postoperative pancreatic fistula,POPF)是胰十二指肠切除术后最常见和严重的并发症[1-2]。由于手术方式的复杂性,术后POPF相关并发症发生率高达30%~50%,可导致患者住院时间延长和住院费用增加,严重者可导致患者再次手术或死亡。文献表明POPF不仅与胰腺组织的硬度、胰管直径和肿瘤部位密切相关[3-4],也受到胰肠吻合方式的影响[5]。在所有相关因素中,胰肠吻合方式是术中唯一可控的因素,因而选择合理的胰肠吻合方式尤为重要[6]。本文回顾性分析2008年10月至2013年8月天津医科大学肿瘤医院肝胆肿瘤科收治的145例术前诊断为壶腹周围肿瘤行胰十二指肠切除术患者的临床资料,对影响POPF发生的相关因素进行分析,探讨胰十二指肠切除术后POPF相关危险因素,特别是胰肠吻合方式对POPF的影响。
1 材料与方法
1.1病例材料
本组接受胰十二指肠切除术患者145例,男性91例,女性54例;年龄22~76岁,中位年龄60岁。胆管下段不典型增生1例,胆管下段癌30例,壶腹癌17例,结肠癌转移壶腹1例,十二指肠癌28例,胰岛细胞瘤4例,胰头癌57例,胰头淋巴瘤1例,胰腺类癌1例,胰腺良性瘤2例,胰腺炎3例。患者术前均无严重心肺功能不全,入院前未进行其他抗肿瘤治疗。全部手术主要实施者为同一名外科医师,常规术前准备后在全身麻醉下行胰十二指肠切除术。
1.2术后胰瘘判断标准
采用国际胰瘘研究组(ISGPF)标准,术后3天或以后腹腔引流液淀粉酶含量为正常血清值上限3倍以上定义为POPF[2]。
1.3统计学分析
应用SPSS 19.0统计软件进行分析,相关性分析采用Pearson χ2检验和Logistic回归。P<0.05为差异具有统计学意义。
2 结果
本组145例患者中27例术后发生POPF,其中A级5例、B级17例、C级5例。本组共采用4种胰肠吻合方式,即端端吻合(end to end,ETE),端侧吻合(end to side,ETS),胰管空肠黏膜吻合(duct to muco⁃sa,DTM)及Blumgart吻合(blumgart anastomosis,BA)。术后胰瘘相关因素包括:性别、胰腺癌、胰肠吻合方式、门静脉受累、胰腺硬度,MPD>3 mm与POPF的发生密切相关(P<0.05)。而年龄、CBD直径、术前胆道感染、胰管支架、胰液外引流、T管引流、术中失血量及术中输血等因素与POPF的发生无关(P>0.05,表1)。应用Logistic回归进行多因素分析结果表明:不同的吻合方式及性别与POPF相关,而胰腺癌、胰腺质地、主胰管直径等客观因素未显示出相关性(表2)。对4种胰肠吻合方式相关的术后并发症情况进行分析,结果显示DTM吻合方式POPF发生率仅为5.9%最低,其次为Blumgart吻合11.6%,端侧吻合方式所致POPF发生率最高为44.4%,而与POPF密切相关的一些并发症,如肺感染、腹腔感染、腹腔出血等,各组间并不存在显著性差异(表3)。
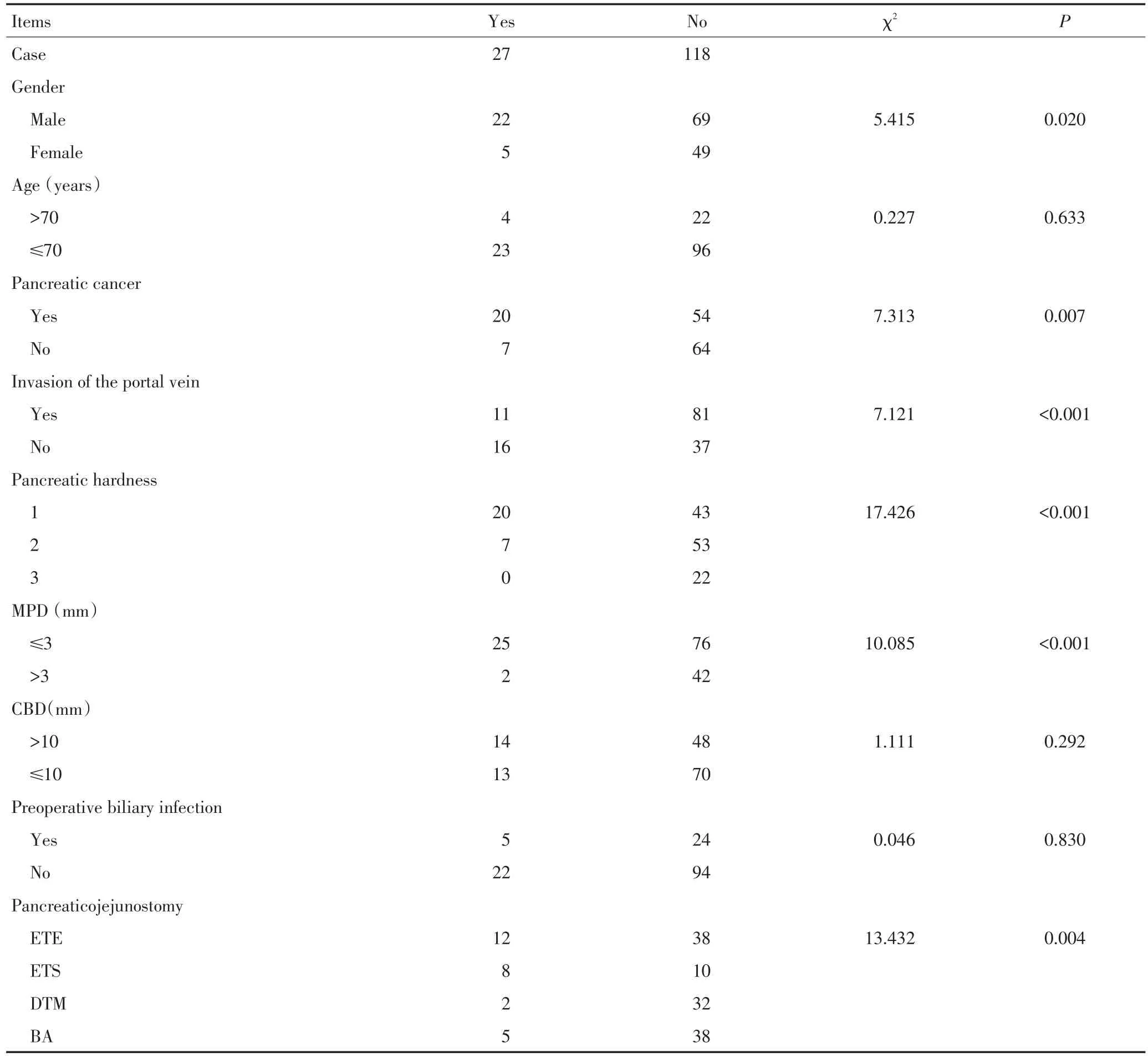
表1 患者一般临床特征及胰瘘发生情况Table 1Clinical characteristics of the patients

表1 患者一般临床特征及胰瘘发生情况(续表1)Table 1Clinical characteristics of the patients
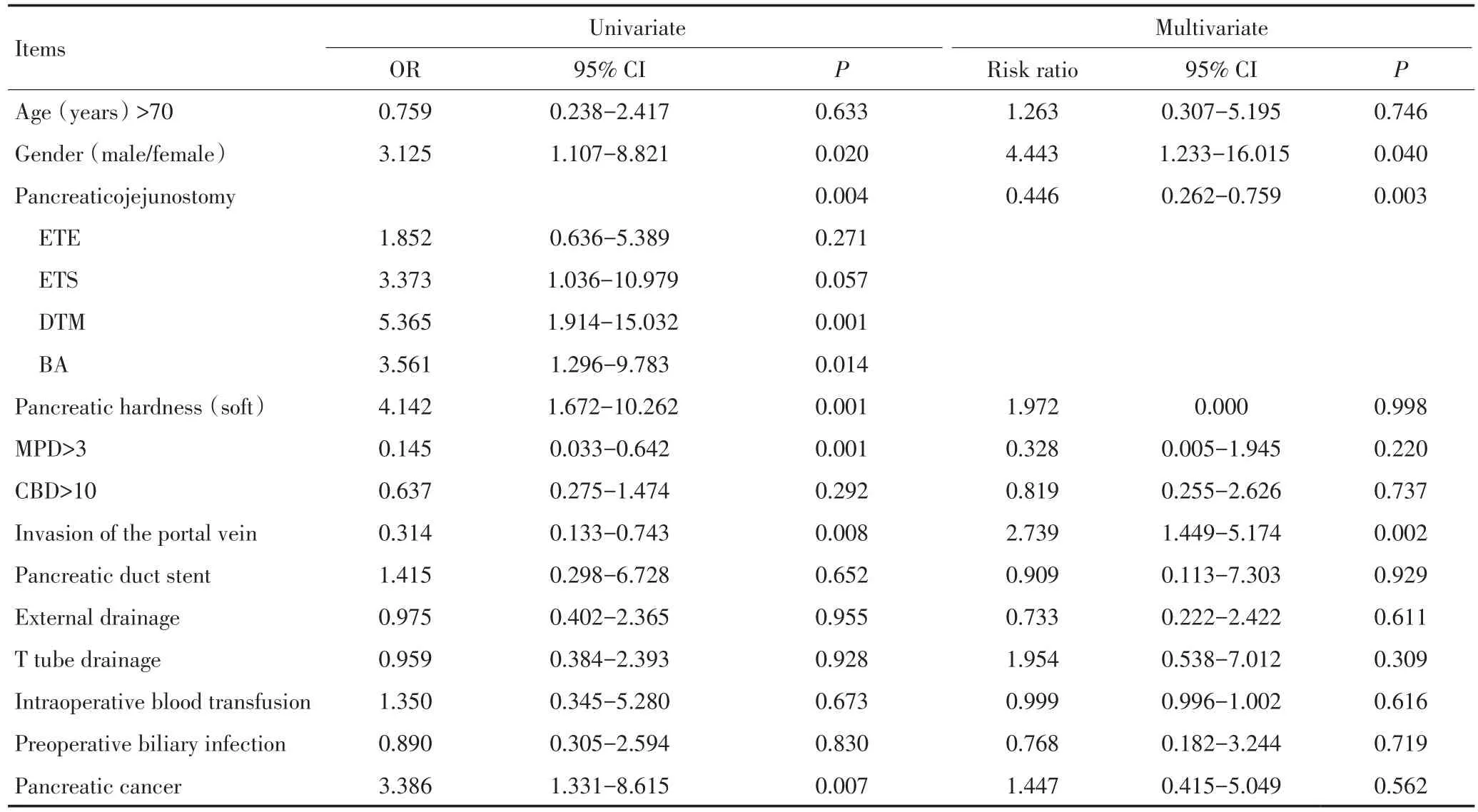
表2 胰十二指肠切除术后胰瘘发生的单因素与多因素分析Table 2Univariate and multivariate analysis
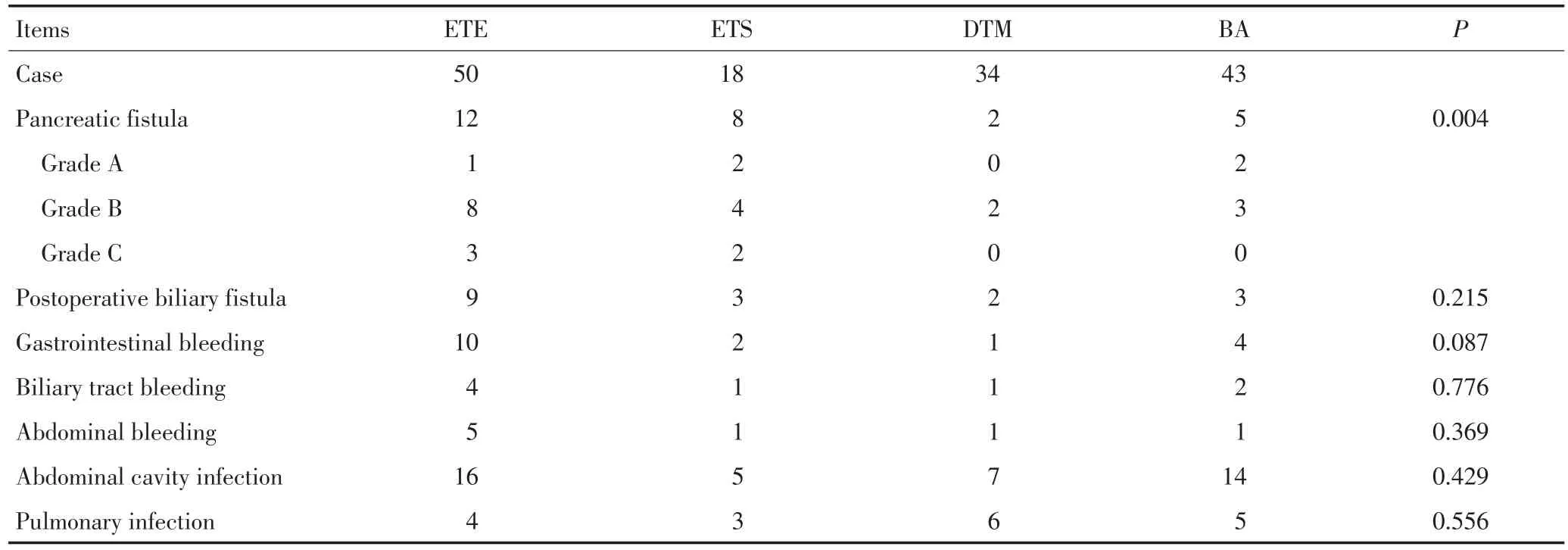
表34 种胰肠吻合方式的术后并发症情况比较Table 3Effects of the four types of pancreaticojejunostomy following pancreaticoduodenectomy on postoperative complications
3 讨论
POPF是胰十二指肠切除术后最严重的并发症,也是近年研究的热点[7]。POPF发生的机制尚不十分明确,但主要有两种表现形式。1)缝针穿过毛细胰管引起单纯性胰液外漏;2)肠腔内消化液突破吻合口薄弱环节和(或)肠管压力增高进入腹腔引起的胰肠吻合口漏[8],这两者均可能与吻合方式有关。传统的胰肠套入式吻合术是目前报道中POPF发生率较高的吻合方式[9],其原因除与胰腺自身的腺体分泌特征有关外,还与其本身的某些缺陷相关。如手术时可因残端过大,第二层吻合时缝合张力过大,吻合口血运较差,受挤压的胰腺引流不畅而导致胰瘘;或者双层缝合时前壁套埋而后壁相对缝合不足,增加了胰腺前壁应力,缝针过浅,特别在质软胰腺中易致胰腺切割,过深则易缝穿分胰管致针眼胰漏增多;此外,双层吻合还可能使胰液、肠黏膜分泌物渗入层间无法排除,导致吻合口局部感染、腐蚀[6]。胰管空肠黏膜吻合方式是目前主要的重建方式之一,POPF发生率在各大中心存在较大差异。近年来,不断有学者对此经典吻合方式进行改进,取得了一些可喜的结果。Lee等[10]报道,针对外层加固缝合,采用连续吻合的方式显著优于间断吻合的方式,可降低POPF发生,更加简便易行。Berger等[11]通过前瞻性随机对照临床试验研究发现,改进的胰腺导管黏膜连续套入吻合在降低POPF发生上优于传统的间断吻合方式。
Blumgart吻合术是由纽约纪念斯隆-凯特琳癌症中心的Blumgart教授发明的一种新型的胰肠吻合技术,其主要是应用了贯穿胰腺实质的U型缝线来完成胰腺前后壁与空肠肠壁的加固吻合,取得了非常理想的临床疗效[12]。通过来自德国和印度的研究证实,Blumgart吻合技术在手术操作过程中更为简洁确切,显著优于传统胰肠吻合[13-14]。Fujii等[15]进一步改进了这种吻合方式,使得POPF发生率降低至2.5%,显著优于其他常用的胰肠吻合方式(36%)。本文探讨4种吻合方式与POPF的关系,即端端吻合、端侧吻合、胰管空肠黏膜吻合及Blumgart吻合,多因素Logis⁃tic回归分析显示,性别和吻合方式为POPF的独立预测因素,而胰腺硬度、胰管直径等客观因素未显示相关性。门脉受累者不易发生POPF,本研究数据显示,ETE组中门脉受累的比例最高,但POPF发生率仍高达24%,显著高于DTM,从一个侧面证实吻合方式的确可降低POPF发生。Poon等[16]随机对照试验研究显示胰管外引流可降低高危患者POPF发生率,本研究数据显示胰管外引流在4种吻合方式组间存在差异,但在多因素分析中与术后POPF并未显示出相关性。在4种吻合方式中,胰管空肠黏膜吻合与Blumgart吻合均取得了良好疗效,不仅POPF发生率显著下降,而且不存在严重的C级POPF。Blumgart吻合操作更为简洁,技术更易掌握,吻合更加牢固。
综上所述,胰肠吻合方式的改进对降低POPF的发生可能起到关键作用,但由于回顾性研究的局限性,仍需严格设计的随机对照临床试验的证实。
[1]Lai EC,Lau SH,Lau WY.Measures to prevent pancreatic fistula after pancreatoduodenectomy:a comprehensive review[J].Arch Surg,2009,144(11):1074-1080.
[2]Bassi C,Dervenis C,Butturini G,et al.Postoperative pancreatic fistula:an international study group(ISGPF)definition[J].Sur⁃gery,2005,138(1):8-13.
[3]Sato N,Mori Y,Minagawa N,et al.Rapid postoperative reduc⁃tion in prognostic nutrition index is associated with the develop⁃ment of pancreatic fistula following distal pancreatectomy[J].Pan⁃creatology,2014,14(3):216-220.
[4]Sugimoto M,Gotohda N,Kato Y,et al.Risk factor analysis and prevention of postoperative pancreatic fistula after distal pancre⁃
atectomy with stapler use[J].J Hepatobiliary Pancreat Sci,2013,20(5):538-544.
[5]Kim WS,Choi DW,Choi SH,et al.Clinical validation of the IS⁃GPF classification and the risk factors of pancreatic fistula forma⁃tion following duct-to-mucosa pancreaticojejunostomy by one surgeon at a single center[J].J Gastrointest Surg,2011,15(12):2187-2192.
[6]Ding HM,Qin XH,Zhu F,et al.Analysis of postoperative com⁃plications of pancreationcoduodenectomy[J].Chinese Journal of General Surgery,2008(3):256-260.[丁会民,秦锡虎,朱峰,等.胰十二指肠切除术后并发症分析[J].中国普通外科杂志,2008(3):256-260.]
[7]Xu ZK,Guo F,Miao Y,et al.Clinical analysis of major postopera⁃tive complications of pancreatoduodenectomy in 502 cases[J]. Chinese Journal of Hepatobiliary Surgery,2009,15(11):809-812.[徐泽宽,郭峰,苗毅,等.502例胰十二指肠切除术后主要并发症的临床分析[J].中华肝胆外科杂志,2009,15(11):809-812.]
[8]Wang JW,Xu B,Cai XJ,et al.The mechanism of pancreatic fistu⁃la after pancreatoduodenectomy[J].World Chinese Journal of Di⁃gestology,2003(5):589-590.[王建伟,许斌,蔡秀军,等.胰十二指肠切除术后胰漏的发生机制[J].世界华人消化杂志,2003(5):589-590.]
[9]Watanabe M,Usui S,Kajiwara H,et al.Current pancreatogastro⁃intestinal anastomotic methods:results of a Japanese survey of 3109 patients[J].J Hepatobiliary Pancreat Surg,2004,11(1):25-33.
[10]Lee SE,Yang SH,Jang JY,et al.Pancreatic fistula after pancreati⁃coduodenectomy:a comparison between the two pancreaticojeju⁃nostomy methods for approximating the pancreatic parenchyma to the jejunal seromuscular layer:interrupted vs continuous stitches[J].World J Gastroenterol,2007,13(40):5351-5356.
[11]Berger AC,Howard TJ,Kennedy EP,et al.Does type of pancre⁃aticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula?A randomized,prospective,dual-institution trial[J].J Am Coll Surg,2009,208(5):738-749.
[12]Grobmyer SR,Kooby D,Blumgart LH,et al.Novel pancreatico⁃jejunostomy with a low rate of anastomotic failure-related com⁃plications[J].J Am Coll Surg,2010,210(1):54-59.
[13]Kleespies A,Rentsch M,Seeliger H,et al.Blumgart anastomosis for pancreaticojejunostomy minimizes severe complications after pancreatic head resection[J].Br J Surg,2009,96(7):741-750.
[14]Mishra PK,Saluja SS,Gupta M,et al.Blumgart's technique of pancreaticojejunostomy:an appraisal[J].Dig Surg,2011,28(4):281-287.
[15]Fujii T,Sugimoto H,Yamada S,et al.Modified Blumgart anasto⁃mosis for pancreaticojejunostomy:technical improvement in matched historical control study[J].J Gastrointest Surg,2014,18(6):1108-1115.
[16]Poon RT,Fan ST,Lo CM,et al.External drainage of pancreatic duct with a stent to reduce leakage rate of pancreaticojejunosto⁃my after pancreaticoduodenectomy:a prospective randomized tri⁃al[J].Ann Surg,2007,246(3):425-435.(2015-01-23收稿)(2015-03-03修回)
(编辑:周晓颖)
Effect of different pancreaticojejunal anastomoses on the occurrence of pancreatic fistula after pancreaticoduodenectomy
Jiafei HUANG,Ti ZHANG,Hongyuan ZHOU,Huikai LI,Yunlong CUI,Qiang LI
Ti ZHANG;E-mail:zhangti@tjmuch.com
Objective:To investigate the effect of pancreaticojejunostomy on the occurrence of postoperative pancreatic fistula(POPF)after pancreaticoduodenectomy.Methods:Data from 145 patients with periampullary tumor who underwent pancreaticoduodenectomy in Tianjin Medical University Cancer Institute and Hospital between October 2008 and August 2013 were reviewed.Factors potentially associated with POPF were analyzed by Pearson chi-square test and Logistic regression analysis.Results:Among the 145 patients,27 were diagnosed with POPF,including 5 grade A,17 grade B and 5 grade C.Neither duct to mucosa nor Blumgart pancreaticojejunostomy was correlated with POPF in grade C.The univariate analysis showed that gender,pancreatic cancer,portal vein involvement,type of pancreaticojejunostomy,texture of pancreas,and diameter of the main pancreatic duct were closely correlated with POPF. The multivariate analysis using Logistic regression showed that different pancreaticojejunal anastomoses and genders were independent predictors of POPF.Conclusion:Different types of pancreatic anastomoses are a risk factor for POPF after pancreaticoduodenectomy.
pancreaticoduodenectomy,pancreaticojejunostomy,pancreatic fistula

10.3969/j.issn.1000-8179.20150123
天津医科大学肿瘤医院肝胆肿瘤科,国家肿瘤临床医学研究中心,天津市肿瘤防治重点实验室(天津市300070)
张倜zhangti@tjmuch.com
Department of Hepatobiliary Surgery,Tianjin Medical University Cancer Institute and Hospital,National Clinical Research Center for Cancer,Tianjin Key Laboratory of Cancer Prevention and Therapy,Tianjin 300060,China
黄佳飞专业方向为肝胆肿瘤的外科诊治及基础研究。
E-mail:2438439213@qq.com

