巨细胞病毒:激素难治性溃疡性结肠炎的一个可能病因*
薛 猛 姒健敏
浙江大学医学院附属邵逸夫医院消化内科 浙江大学胃肠病研究所(310016)
溃疡性结肠炎(UC)是一种以结肠黏膜弥漫性病变为特征的特发性慢性炎症性疾病。尽管5-氨基水杨酸制剂和激素能缓解大多数UC患者的症状,仍有约30%的住院患者对激素治疗无应答,需通过免疫调节剂和(或)生物制剂甚至手术治疗以缓解症状[1]。许多研究试图阐明UC的潜在致病机制,并寻求有效治疗方法。
巨细胞病毒(cytomegalovirus,CMV)是人类疱疹病毒科中病毒体结构最大的成员,具有一双链DNA核,其外包被衣壳蛋白、壳皮蛋白和囊膜蛋白,这些蛋白有利于CMV逃避宿主免疫反应,并可调节宿主基因转录和翻译[2]。CMV感染包括急性感染和CMV重新激活,是一种可侵犯机体内多个器官,特别是腺上皮和腔道上皮的系统性疾病。CMV病毒体可通过血液循环到达靶器官,继而通过内吞作用进入内皮细胞。感染细胞肿胀并在核内形成巨大的包涵体[3]。
大多数情况下,CMV感染人体后终生保持潜伏,然而在免疫低下患者中,如HIV感染者、器官移植者[4]或因患自身免疫性疾病如 UC[5~7]而接受免疫抑制治疗者,CMV可逃避宿主免疫监视而重新激活(见图1)。
越来越多的证据表明,感染CMV的UC患者易发生激素治疗无效,CMV与激素难治性UC密切相关的观点已被广泛接受。本综述旨在简要回顾现有证据,并讨论这一相关性的可能机制。
一、CMV增加UC患者激素耐药的风险
炎症性肠病(IBD)患者中急性CMV感染并不罕见且常被低估。难治性或复杂IBD患者在接受冲击性免疫抑制治疗前应排除CMV感染[8]。一些研究[9~17]报道,大多数CMV阳性UC患者对激素治疗无应答,CMV阳性者的激素耐药发生率远高于CMV阴性者(见表1)。
Wada等[10]发现,CMV 阳性 UC患者中的重症者比例显著高于CMV阴性患者。Kuwabara等[13]报道,从CMV阴性、CMV轻微感染至CMV重度感染,UC患者的临床表现逐渐加重。与CMV阴性UC患者相比,CMV阳性患者常于激素治疗的基础上接受AZA、CsA 和英夫利西单抗治疗[18]。
二、CMV阳性UC患者的手术治疗
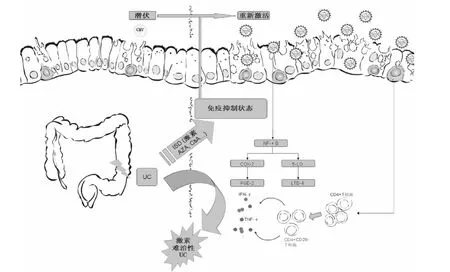
图1 CMV重新激活的机制及其在激素难治性UC中的作用
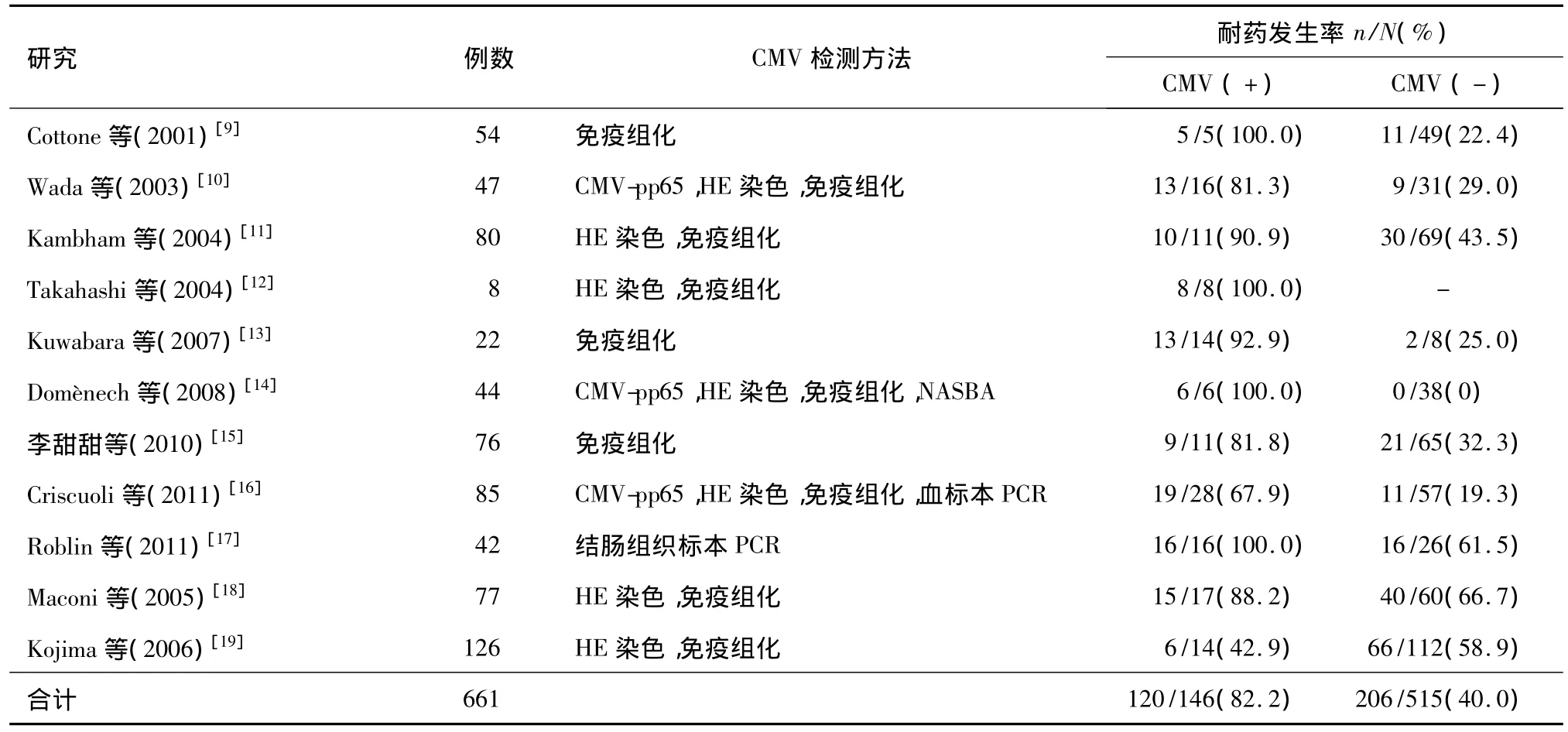
表1 CMV阳性和CMV阴性UC患者激素耐药发生率
与CMV阴性UC患者相比,CMV阳性患者手术指征更强,手术时机更为迫切,术后住院时间更长,术后并发症更常见,而适当的抗病毒治疗可缩短术后住院时间[13],降低对IBD相关结肠切除术的需求和死亡率[20]。一系列病例报道表明,CMV感染UC患者常发生中毒性巨结肠,在这些患者中,CMV检出的延迟可能最终导致结肠切除[21,22]。Kishore等[23]亦发现,IBD患者如合并CMV感染,需接受手术治疗(4/10对4/53)和死亡结局(3/10对0/53)将更为常见。
三、抗CMV治疗的有效性
一些回顾性和前瞻性研究报道,对于激素难治性UC患者,抗CMV治疗可诱导缓解,避免肠段切除。Kambham等[11]报道,3例确诊CMV感染的UC患者接受静脉输注更昔洛韦或口服伐昔洛韦治疗后症状得以改善,激素逐渐减量并避免了结直肠切除。因此激素难治性UC患者应常规评估有无CMV感染,以避免不必要的药物或手术治疗[22]。一项前瞻性多中心研究[24]显示,78.6%(11/14)的CMV 感染激素难治性UC患者经更昔洛韦治疗后获得缓解。一些研究[7,10,11,14,16,17,22,24~30]评价了抗病毒治疗对CMV阳性激素难治性UC患者的有效性,结果显示不同研究人群缓解率不一,但总体缓解率可达80.2%(见表2)。
四、研究结果的不一致性
然而,并非所有研究均会显示出一致的结果。Maconi等[18]的研究中,CMV阳性与 CMV阴性 UC患者中激素抵抗者的比例差异无统计学意义(88%对67%)。一项回顾性研究[31]显示,激素依赖和需手术治疗与结肠组织检出CMV无统计学相关性。推测CMV检测方法可能会有一些假阴性结果,可以用来解释CMV阴性的激素难治性UC。此外,据信CMV感染是激素难治性UC的重要原因但并非惟一原因,因此一些小样本研究结果不一致并不能否定大量支持性证据。
Kojima等[19]将UC患者根据手术指征分为重度UC、难治性UC和UC相关异型增生/癌变组,评估三组患者的CMV感染率以及组间关系,发现难治性UC组CMV感染率低于重度UC组(8.3%对25%),重度UC患者因症状危重或致死性并发症(已排除UC相关异型增生/癌变患者)而寻求手术治疗可以用来解释这一现象。如果这些患者对激素治疗应答良好,手术治疗就不会成为首选治疗方式。这些患者病情过于严重,以致缺乏足够长的激素治疗“时间窗”,正是他们未被诊断为激素难治性UC的原因。
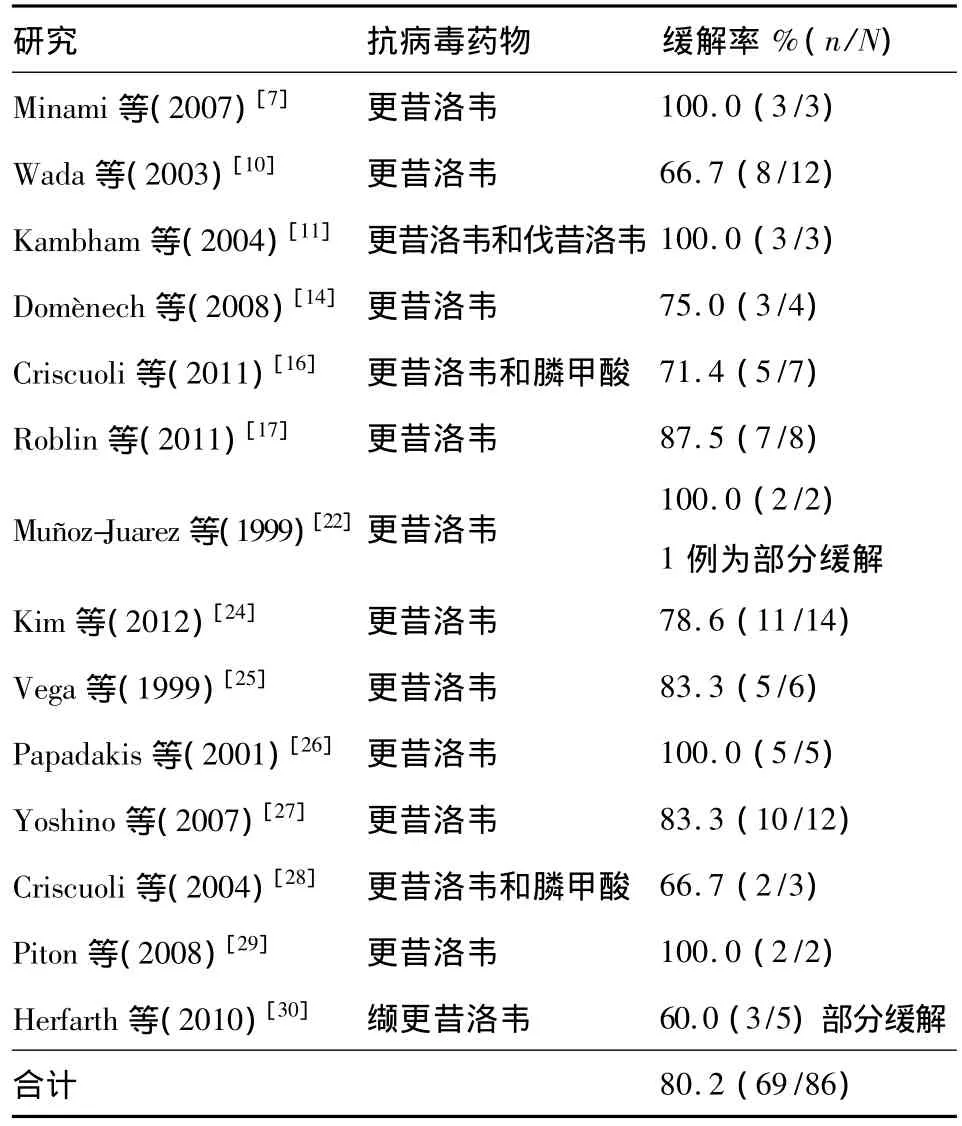
表2 CMV阳性激素难治性UC患者接受抗病毒治疗后的缓解率
Matsuoka等[5]报道,在一些活动期UC患者中,重新激活的CMV感染在未使用抗病毒药物的情况下自行消失。一些CMV重新激活具有自限性,可以解释CMV阳性活动期UC患者在未使用抗病毒药物的情况下仍能获得缓解[32]。部分CMV感染UC患者抗病毒治疗效果不佳,可能系更昔洛韦耐药所致[33]。
五、可能机制
UC是一种主要累及结肠的炎症性疾病。尽管已提出多种假说,但其病因仍未完全阐明。已得到公认的四个UC基本病因为遗传、免疫调节障碍、肠黏膜屏障功能障碍和肠道菌群[34]。已发现一些病原体可能与UC相关,如JC多瘤病毒[35]和鸟分枝杆菌副结核亚种[36]。首例合并CMV感染的UC报道于1961年,但目前对CMV是一种UC病原体还是一个无关“过路者”,观点仍不一致[37],本文所回顾的临床研究大多数显示CMV感染与激素难治性UC密切相关。由于CMV的存在可诱导持续的免疫功能障碍,在UC发病中起关键作用[38],CMV阳性活动期UC患者很少能获得缓解,给予抗CMV药物有利于诱导缓解。
过去数十年中的大量研究揭示了CMV感染与激素难治性UC相关的可能机制。通过插入可模拟宿主基因功能的基因,病毒蛋白与宿主细胞蛋白交叉反应,引起自身免疫样病变[39]。CMV可引起T细胞功能障碍,如诱导CD4+T细胞分化为CD4+CD28-T细胞[40]。在缺乏共刺激分子CD28的情况下,CD4+T细胞可产生大量Th1型细胞因子,如IFN-γ 和 TNF-α,从而加剧炎症反应[41]。此外,CMV尚可激活NF-кB信号通路[42],诱导促炎细胞因子,包括 COX-2[43]、5-LO[44]等表达,导致炎症反应恶化(见图1)。
CMV颗粒的成熟伴随着胞内细胞毒性CD13分子增多。对常规药物治疗无应答而接受手术治疗的重度UC患者较易检出抗CD13自身抗体。在人结肠癌Caco-2细胞中加入上述患者的血清可增加死亡细胞比例,阻断CD13则可降低其比例[45]。
六、展望未来
Koch’s准则包括四条标准,是一种可用于确定某一特定疾病病原微生物的方法,曾被用于发现HIV[46]和幽门螺杆菌[47]。第一条标准为患病个体中大量存在该病原体,健康个体中则不存在,该标准已基本为本文所回顾的研究证实,但仍需大量在严格纳入标准下获得的高质量标本,以检测激素难治性UC患者中CMV的存在情况,可联合应用不同检测方法以降低假阳性率和假阴性率[48]。第二条标准为病原体能在纯培养基上生长,从激素难治性UC患者中可分离出CMV满足该标准。可通过采用UC动物模型评估外源性CMV的致病性,以及确认日后能否从动物模型中分离出CMV,来满足第三和第四条标准。
糖皮质激素的药理作用依赖于糖皮质激素受体(GR)。GR有GRα和GRβ两个亚型,其中GRα为功能亚型,GRβ无生理学活性,但能与GRα结合而阻断其活性。P-糖蛋白170由多药耐药基因MDR编码,定位于淋巴细胞和肠上皮细胞的细胞膜,可将激素泵出细胞以减弱其作用。已发现激素难治性UC患者存在GRβ和MDR高表达[49,50]。检测感染外源性CMV的结肠细胞和实验动物的GRβ和MDR表达可确定CMV是否系通过调节这些靶点诱导UC患者对激素治疗产生抵抗。
七、结论
根据本文所回顾的证据,可以认为CMV可能在激素难治性UC的发病中起一定作用。尚需进一步开展基础研究和前瞻性大样本临床研究,以使该假说更令人信服。
1 Moss AC,Peppercorn MA.Steroid-refractory severe ulcerative colitis:what are the available treatment options[J]?Drugs,2008,68(9):1157-1167.
2 Britt WJ,Boppana S.Human cytomegalovirus virion proteins[J].Hum Immunol,2004,65(5):395-402.
3 Sinzger C.Entry route of HCMV into endothelial cells[J].J Clin Virol,2008,41(3):174-179.
4 Crough T,Khanna R.Immunobiology of human cytomegalovirus:from bench to bedside[J].Clin Microbiol Rev,2009,22(1):76-98.
5 Matsuoka K,Iwao Y,Mori T,et al.Cytomegalovirus is frequently reactivated and disappearswithoutantiviral agents in ulcerative colitis patients[J]. Am J Gastroenterol,2007,102(2):331-337.
6 Nguyen M,Bradford K,Zhang X,et al.Cytomegalovirus reactivation in ulcerative colitis patients[J].Ulcers,2011,pii:282507.
7 Minami M,Ohta M,Ohkura T,et al.Cytomegalovirus infection in severe ulcerative colitis patients undergoing continuous intravenous cyclosporine treatment in Japan[J].World J Gastroenterol,2007,13(5):754-760.
8 Maher MM,Nassar MI.Acute cytomegalovirus infection is a risk factor in refractory and complicated inflammatory bowel disease[J].Dig Dis Sci,2009,54(11):2456-2462.
9 Cottone M,Pietrosi G,Martorana G,et al.Prevalence of cytomegalovirus infection in severe refractory ulcerative and Crohn’s colitis[J].Am J Gastroenterol,2001,96(3):773-775.
10 Wada Y,Matsui T,Matake H,et al.Intractable ulcerative colitis caused by cytomegalovirus infection:a prospective study on prevalence,diagnosis,and treatment[J].Dis Colon Rectum,2003,46(10 Suppl):S59-S65.
11 Kambham N,Vij R,Cartwright CA,et al.Cytomegalovirus infection in steroid-refractory ulcerative colitis:a casecontrol study[J].Am J Surg Pathol,2004,28(3):365-373.
12 Takahashi Y,Tange T.Prevalence of cytomegalovirus infection in inflammatory bowel disease patients[J].Dis Colon Rectum,2004,47(5):722-726.
13 Kuwabara A,Okamoto H,Suda T,et al.Clinicopathologic characteristics of clinically relevant cytomegalovirus infection in inflammatory bowel disease[J]. J Gastroenterol,2007,42(10):823-829.
14 Domènech E,Vega R,Ojanguren I,et al.Cytomegalovirus infection in ulcerative colitis:a prospective,comparative study on prevalence and diagnostic strategy[J].Inflamm Bowel Dis,2008,14(10):1373-1379.
15 李甜甜,吕宗舜,王邦茂,等.难治性溃疡性结肠炎与巨细胞病毒的关系[J].世界华人消化杂志,2010,18(11):1174-1177.
16 Criscuoli V,Rizzuto MR,Montalbano L,et al.Natural history of cytomegalovirus infection in a series of patients diagnosed with moderate-severe ulcerative colitis[J].World J Gastroenterol,2011,17(5):633-638.
17 Roblin X,Pillet S,Oussalah A,et al.Cytomegalovirus load in inflamed intestinal tissue is predictive of resistance to immunosuppressive therapy in ulcerative colitis[J].Am J Gastroenterol,2011,106(11):2001-2008.
18 Maconi G,Colombo E,Zerbi P,et al.Prevalence,detection rate and outcome of cytomegalovirus infection in ulcerative colitis patients requiring colonic resection[J].Dig Liver Dis,2005,37(6):418-423.
19 Kojima T,Watanabe T,Hata K,et al.Cytomegalovirus infection in ulcerative colitis[J].Scand J Gastroenterol,2006,41(6):706-711.
20 Begos DG,Rappaport R,Jain D.Cytomegalovirus infection masquerading as an ulcerative colitis flare-up:case report and review of the literature[J].Yale J Biol Med,1996,69(4):323-328.
21 Shimada Y,Iiai T,Okamoto H,et al.Toxic megacolon associated with cytomegalovirusinfection in ulcerative colitis[J].J Gastroenterol,2003,38(11):1107-1108.
22 Muñoz-Juarez M,Pemberton JH,Sandborn WJ,et al.Misdiagnosis of specific cytomegalovirus infection of the ileoanal pouch as refractory idiopathic chronic pouchitis:report of two cases[J].Dis Colon Rectum,1999,42(1):117-120.
23 Kishore J,Ghoshal U,Ghoshal UC,et al.Infection with cytomegalovirus in patients with inflammatory bowel disease:prevalence,clinical significance and outcome[J].J Med Microbiol,2004,53(Pt 11):1155-1160.
24 Kim YS,Kim YH,Kim JS,et al;IBD Study Group of the Korean Association for the Study of Intestinal Diseases.The prevalence and efficacy of ganciclovir on steroid-refractory ulcerative colitis with cytomegalovirus infection:a prospective multicenter study[J].J Clin Gastroenterol,2012,46(1):51-56.
25 Vega R,Bertrán X,Menacho M,et al.Cytomegalovirus infection in patients with inflammatory bowel disease[J].Am J Gastroenterol,1999,94(4):1053-1056.
26 Papadakis KA,Tung JK,Binder SW,et al.Outcome of cytomegalovirus infections in patients with inflammatory bowel disease[J].Am J Gastroenterol,2001,96(7):2137-2142.
27 Yoshino T,Nakase H,Ueno S,et al.Usefulness of quantitative real-time PCR assay for early detection of cytomegalovirus infection in patients with ulcerative colitis refractory to immunosuppressive therapies[J].Inflamm Bowel Dis,2007,13(12):1516-1521.
28 Criscuoli V,Casà A,Orlando A,et al.Severe acute colitis associated with CMV:a prevalence study[J].Dig Liver Dis,2004,36(12):818-820.
29 Piton G,Dupont-Gossart AC,Weber A,et al.Severe systemic cytomegalovirus infections in patients with steroidrefractory ulcerative colitis treated by an oral microemulsion form of cyclosporine:report of two cases[J].Gastroenterol Clin Biol,2008,32(5 Pt 1):460-464.
30 Herfarth HH,Long MD,Rubinas TC,et al.Evaluation of a non-invasive method to detect cytomegalovirus(CMV)-DNA in stool samples of patients with inflammatory bowel disease(IBD):a pilot study[J].Dig Dis Sci,2010,55(4):1053-1058.
31 Lévêque N,Brixi-Benmansour H,Reig T,et al.Low frequency of cytomegalovirus infection during exacerbations of inflammatory bowel diseases[J].J Med Virol,2010,82(10):1694-1700.
32 Ogata M,Satou T,Kawano R,et al.High incidence of cytomegalovirus,human herpesvirus-6,and Epstein-Barr virus reactivation in patients receiving cytotoxic chemotherapy for adult T cell leukemia[J].J Med Virol,2011,83(4):702-709.
33 Lurain NS,Chou S.Antiviral drug resistance of human cytomegalovirus[J].Clin Microbiol Rev,2010,23(4):689-712.
34 Kucharzik T,Maaser C,Lügering A,et al.Recent understanding of IBD pathogenesis:implications for future therapies[J].Inflamm Bowel Dis,2006,12(11):1068-1083.
35 Altschuler EL.Is JC polyoma virus the cause of ulcerative colitis and multiple sclerosis[J]?Med Hypotheses,2000,55(4):335-336.
36 Juste RA,Elguezabal N,Pavón A,et al.Association between Mycobacterium avium subsp.paratuberculosis DNA in blood and cellular and humoral immune response in inflammatory bowel disease patients and controls[J].Int J Infect Dis,2009,13(2):247-254.
37 Lawlor G,Moss AC.Cytomegalovirus in inflammatory bowel disease:pathogen or innocent bystander[J]?Inflamm Bowel Dis,2010,16(9):1620-1627.
38 Brown SJ,Mayer L.The immune response in inflammatory bowel disease[J].Am J Gastroenterol,2007,102(9):2058-2069.
39 Michelson S.Consequences of human cytomegalovirus mimicry[J].Hum Immunol,2004,65(5):465-475.
40 van Leeuwen EM,Remmerswaal EB,Vossen MT,et al.Emergence ofa CD4 + CD28-granzyme B +,cytomegalovirus-specific T cell subset after recovery of primary cytomegalovirus infection[J].J Immunol,2004,173(3):1834-1841.
41 Komocsi A,Lamprecht P,Csernok E,et al.Peripheral blood and granuloma CD4(+)CD28(-)T cells are a major source of interferon-gamma and tumor necrosis factoralpha in Wegener’s granulomatosis[J].Am J Pathol,2002,160(5):1717-1724.
42 Isern E,Gustems M,Messerle M,et al.The activator protein 1 binding motifs within the human cytomegalovirus major immediate-early enhancer are functionally redundant and act in a cooperative manner with the NF-kappa B sites during acute infection[J].J Virol,2011,85(4):1732-1746.
43 Zhu H,Cong JP,Yu D,et al.Inhibition of cyclooxygenase 2 blocks human cytomegalovirus replication[J].Proc Natl Acad Sci U S A,2002,99(6):3932-3937.
44 Qiu H,Strååt K,Rahbar A,et al.Human CMV infection induces 5-lipoxygenase expression and leukotriene B4 production in vascular smooth muscle cells[J].J Exp Med,2008,205(1):19-24.
45 Rahbar A,Boström L,Söderberg-Naucler C.Detection of cytotoxic CD13-specific autoantibodies in sera from patients with ulcerative colitis and Crohn’s disease[J]. J Autoimmun,2006,26(3):155-164.
46 O’Brien SJ,Goedert JJ.HIV causes AIDS:Koch’s postulates fulfilled[J].Curr Opin Immunol,1996,8(5):613-618.
47 Wang TC,Fox JG.Helicobacter pylori and gastric cancer:Koch’s postulates fulfilled[J]?Gastroenterology,1998,115(3):780-783.
48 Nagata N,Kobayakawa M,Shimbo T,et al.Diagnostic value of antigenemia assay for cytomegalovirus gastrointestinal disease in immunocompromised patients[J].World J Gastroenterol,2011,17(9):1185-1191.
49 Fujishima S,Takeda H,Kawata S,et al.The relationship between the expression of the glucocorticoid receptor in biopsied colonic mucosa and the glucocorticoid responsiveness of ulcerative colitis patients[J].Clin Immunol,2009,133(2):208-217.
50 Farrell RJ,Murphy A,Long A,et al.High multidrug resistance(P-glycoprotein 170)expression in inflammatory bowel disease patients who fail medical therapy[J].Gastroenterology,2000,118(2):279-288.

