DWI联合MRI动态增强扫描在诊断宫颈癌分期中的应用
王新婧 施磊 李兵 冯吟 朱楠
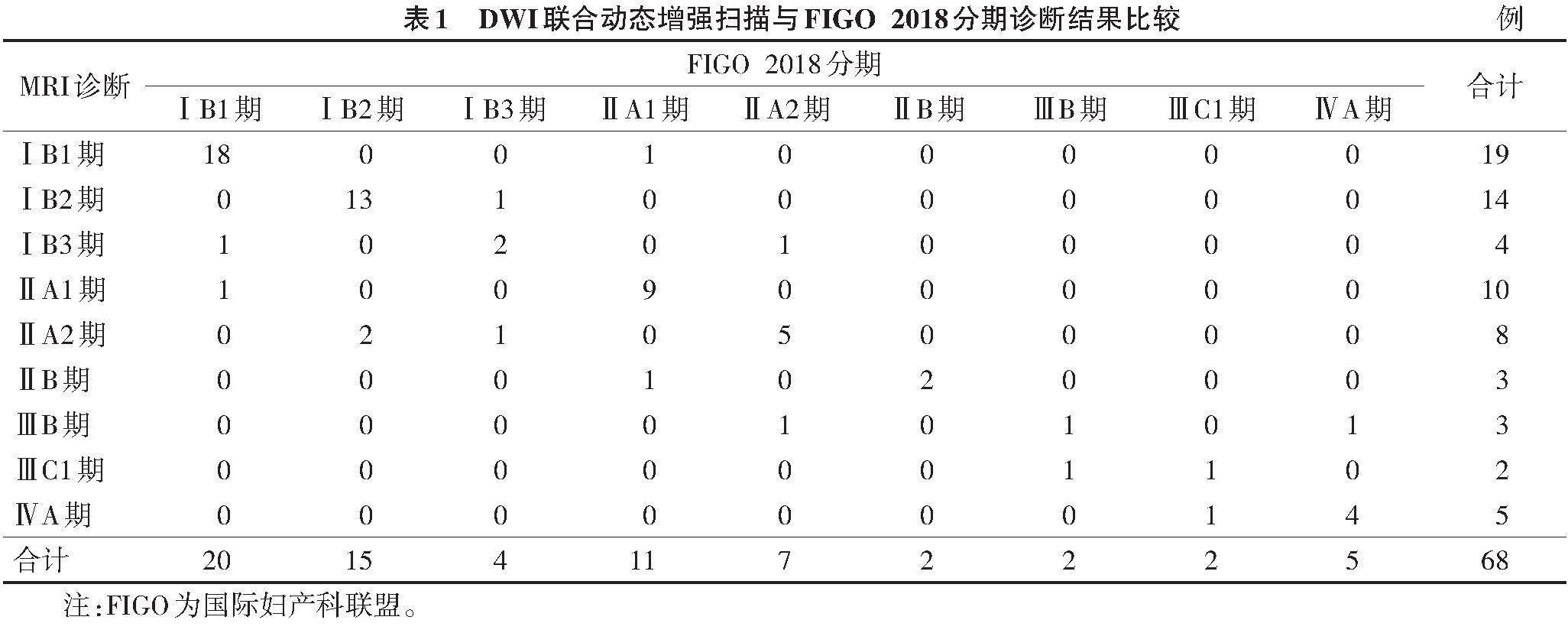
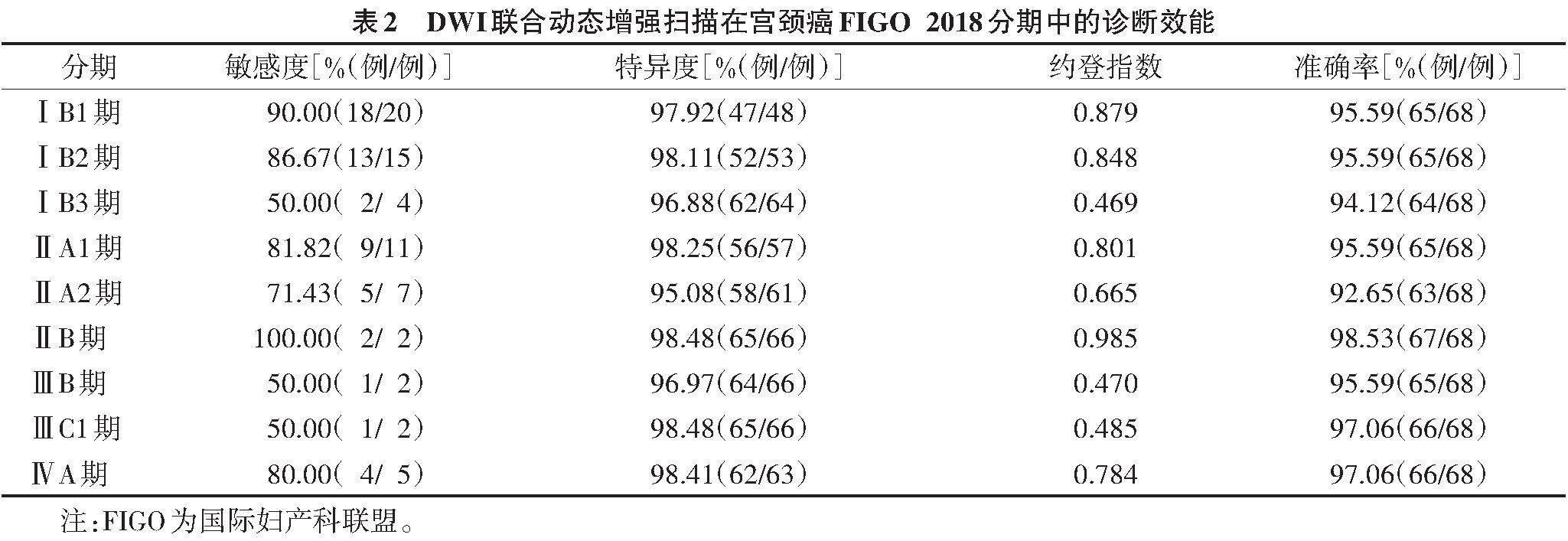
[摘要] 目的:分析DWI联合MRI动态增强扫描在宫颈癌国际妇产科联盟(FIGO)2018分期中的应用效果。方法:回顾性分析68例经病理证实的宫颈癌患者,均行DWI和动态增强扫描,分析DWI联合动态增强扫描与FIGO 2018分期的诊断一致性。结果:68例中,FIGO 2018分期ⅠB1期20例、ⅠB2期15例、ⅠB3期4例、ⅡA1期11例、ⅡA2期7例、ⅡB期2例、ⅢB期2例、ⅢC1期2例、ⅣA期5例;DWI联合动态增强扫描示55例与FIGO 2018分期一致,其中,ⅠB1期18例、ⅠB2期13例、ⅠB3期2例、ⅡA1期9例、ⅡA2期5例、ⅡB期2例、ⅢB期1例、ⅢC1期1例、ⅣA期4例。经Kappa检验,2种诊断方法的一致性较好(K=0.768,P<0.05)。DWI联合动态增强扫描诊断宫颈癌ⅠB1、ⅠB2、ⅠB3、ⅡA1、ⅡA2、ⅡB、ⅢB、ⅢC1、ⅣA期的约登指数分别为0.879、0.848、0.469、0.801、0.665、0.985、0.470、0.485、0.784,准确率分别为95.59%、95.59%、94.12%、95.59%、92.65%、98.53%、95.59%、97.06%、97.06%。结论:DWI联合MRI动态增强扫描对宫颈癌的诊断与FIGO 2018分期的一致性较好,诊断准确率较高。
[关键词] 宫颈癌;磁共振成像;扩散加权成像;动态增强扫描;国际妇产科联盟
Application of DWI combined with dynamic contrast-enhanced MRI in diagnosis of cervical cancer staging
[Abstract] Objective:To explore the application of DWI combined with dynamic contrast-enhanced MRI in FIGO 2018 staging for cervical cancer. Methods:The data of 68 patients with cervical cancer were retrospectively analyzed. They all underwent DWI and dynamic contrast-enhanced MRI. The consistency between DWI combined with dynamic contrast-enhanced scan diagnosis and FIGO 2018 staging was analyzed. Results:Among the 68 patients,20 cases were FIGO 2018 stage ⅠB1,15 were stage ⅠB2,4 were stage ⅠB3,11 were stage ⅡA1,7 were stage ⅡA2,2 were stage ⅡB,2 were stage ⅢB,2 were stage ⅢC1,and 5 were stage ⅣA. DWI combined with dynamic contrast-enhanced scan were consistent with FIGO 2018 staging in 55 cases,18 cases of stage ⅠB1,13 of stage ⅠB2,2 of stage ⅠB3,9 of stage ⅡA1,5 of stage ⅡA2,2 of stage ⅡB,1 of stage ⅢB,1 of stage ⅢC1 and 4 of stage ⅣA. And Kappa consistency test showed a good consistency between the two diagnostic methods (K=0.768,P<0.05). The Youden indices of DWI combined with dynamic contrast-enhanced scan in the diagnosis of cervical cancer at stages ⅠB1,ⅠB2,ⅠB3,ⅡA1,ⅡA2,ⅡB,ⅢB,ⅢC1 and ⅣA were 0.879,0.848,0.469,0.801,0.665,0.985,0.470,0.485 and 0.784,respectively,and the accuracies were 95.59%,95.59%,94.12%,95.59%,92.65%,98.53%,95.59%,97.06% and 97.06%,respectively. Conclusions:DWI combined with dynamic contrast-enhanced MRI has a consistency with FIGO 2018 staging in diagnosis of cervical cancer,and has a high diagnostic accuracy.
[Key words] Cervical cancer;Magnetic resonance imaging;Diffusion weighted imaging;Dynamic enhanced scanning;International Federation of Gynecology and Obstetrics
宫颈癌是女性常见的恶性肿瘤之一,其发病率仅次于乳腺癌,严重威胁女性身体健康和生命安全[1]。因此,宫颈癌的定期筛查和早期诊断非常重要[2]。此外,明确宫颈癌分期对制订治疗方案和改善预后也至关重要。宫颈癌国际妇产科联盟(International Federation of Gynecology and Obstetrics,FIGO)2018分期是世界公认的宫颈癌分期系统,其首次提出根据影像学检查判断肿瘤分期,并将ⅠB期进一步分为ⅠB1期、ⅠB2期和ⅠB3期,将淋巴结转移定为独立分期ⅢC期[3]。在现有的影像诊断技术中,超声因其方便、成本低廉而被广泛应用于癌症筛查,CT密度分辨力高,可清晰显示密度差异较小的器官和软组织结构,但两者均无法判断宫颈癌的浸润和转移,临床应用受到限制[4-5]。MRI具有多参数、多序列成像和高组织分辨力的优点,是宫颈癌诊断和分期的重要检查方法,可明确大部分宫颈癌形态特征,但对宫旁浸润的诊断准确率较低[6]。近年来,DWI和动态增强扫描等技术的出现,极大提高了MRI在肿瘤临床诊断中的准确率。DWI基于水分子微观布朗运动,通过检测水分子活动自由度发现组织微观结构变化,能更明显地显示细微异常[7]。MRI動态增强扫描可根据对比剂强度变化反映肿瘤组织血供和微循环状态[8]。本研究将DWI联合MRI动态增强扫描用于宫颈癌的FIGO 2018分期诊断,探讨其诊断准确性,以期为宫颈癌的临床诊断提供参考。
1 资料与方法
1.1 一般资料
回顾性分析2020年3月至2023年3月合肥市妇幼保健院收治的68例均经病理检查证实的宫颈癌患者,其中,57例经手术获取病灶组织,11例进展期患者经活检获取病灶组织。
纳入标准:均符合宫颈癌诊断标准[9];未行放化疗;MRI图像清晰,资料完整。排除标准:MRI检查禁忌证;精神疾病,沟通或认知障碍;凝血功能障碍;子宫肌瘤患者;先天性心脏病;肝肾功能不全;血液系统疾病;全身感染性疾病。
1.2 仪器与方法
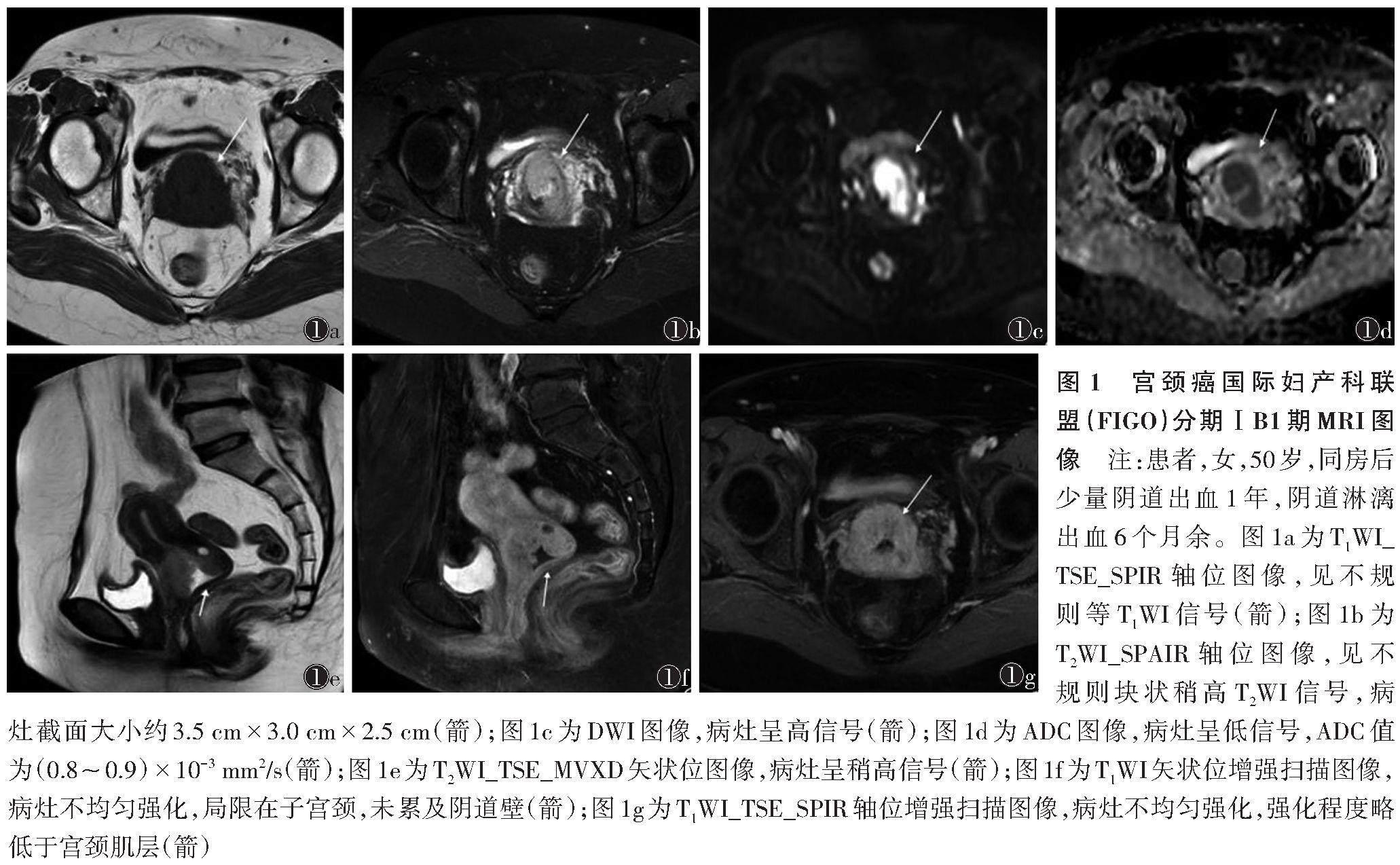
使用Philips Ingenia 1.5 T MRI扫描仪,腹部相控阵线圈。检查前患者禁食6 h以上,饮水300~600 mL适度充盈膀胱。扫描范围:轴位从双侧髂骨上缘至耻骨下缘,矢状位根据病变具体位置和范围进一步确定。扫描参数:层厚4 mm,回波链长9.6,矩阵320×320,视野28 cm×28 cm,层距1 mm。后行DWI和动态增强扫描,注射对比剂钆双胺注射液,以肿瘤为中心重复扫描收集动态增强扫描图像,连续扫描4个时期,包括T1WI_TSE_SPIR轴位图像、T2WI_SPAIR轴位图像、DWI图像、T2WI_TSE_MVXD矢状位图像和T1WI_TSE_SPIR轴位增强扫描图像。
1.3 图像分析
将图像上传至工作站,由2位经验丰富的放射科医师采用双盲法阅片,根据FIGO 2018分期[10]统计阅片结果,意见不一致时经协商解决。
1.4 统计学分析
应用SPSS 22.0软件分析数据。符合正态分布的计量资料以x±s表示,组间比较行t检验;计数资料用%表示,组间比较行χ2检验。采用Kappa检验评估DWI联合动态增强扫描与FIGO 2018分期诊断的一致性,其中K0.75为一致性较好,0.40~0.75为一致性一般,<0.40为一致性差。以P<0.05为差异有统计学意义。
2 结果
根据FIGO 2018分期,68例中ⅠB1期20例、ⅠB2期15例、ⅠB3期4例、ⅡA1期11例、ⅡA2期7例、ⅡB期2例、ⅢB期2例、ⅢC1期2例、ⅣA期5例。DWI联合动态增强扫描示55例与FIGO 2018分期一致,其中,ⅠB1期18例、ⅠB2期13例、ⅠB3期2例、ⅡA1期9例、ⅡA2期5例、ⅡB期2例、ⅢB期1例、ⅢC1期1例、ⅣA期4例。2种诊断方法的一致性较好(K=0.768,P<0.05)(表1)。宫颈癌FIGO 2018分期ⅠB1、ⅡA2期MRI图像见图1,2。
DWI联合动态增强扫描对宫颈癌的诊断效能较高(表2)。
3 讨论
宫颈癌发病与人乳头瘤病毒感染、衣原体感染、宫内节育器的使用等多种复杂因素有关,发病早期症状隐匿,临床确诊时大多已进入中晚期,治疗难度较大,预后较差[11-12]。据统计,全球每年新增50万例宫颈癌患者,其中死亡人数约26万,占女性所有肿瘤死亡人数的7.5%[13]。病理学检查是临床诊断宫颈癌的金标准,但其为侵入性检查[14]。MRI无创、经济、操作简单,相比CT、超声等其他影像学方法具有高分辨力、多平面、多参数等优点,是目前检查宫颈癌的首选方法[15]。宫颈癌术前分期诊断对治疗方法的选择具有重要作用,根据FIGO 2018分期,ⅡB期前多采用手术治疗,而ⅡB期及以后以放疗为主[16]。常规MRI檢查对宫颈两侧缘边界显示不清,易导致分期诊断准确率较低[17]。研究发现,与常规MRI扫描相比,DWI图像组织对比度更高,可清晰显示宫颈病灶和宫旁组织,但分辨力相对降低[18-19]。此外,MRI动态增强扫描可反映病灶血流动力学特点,通过对比剂浓度变化评估肿瘤血管结构和功能特性[20-21]。因此,常规MRI扫描、DWI及动态增强扫描三者联合可为临床诊断提供更充分的证据。
本研究DWI联合动态增强扫描示55例与FIGO 2018分期一致,其中18例ⅠB1期、13例ⅠB2期、2例ⅠB3期、9例ⅡA1期、5例ⅡA2期、2例ⅡB期,1例ⅢB期、1例ⅢC1期、4例ⅣA期,与FIGO 2018分期诊断一致性较好(K=0.768)。宫颈癌肿瘤细胞分裂活跃,大多排列紧密、细胞间隙小,常导致水分子扩散运动受限,宫颈癌病灶DWI多呈高信号,周围结构组织则呈低信号[22-23]。肿瘤可使阴道壁扩张,导致阴道壁变薄,可能出现阴道壁受侵的假阳性结果[24]。MRI动态增强扫描可反映病灶组织血供差异,宫颈癌组织新生血管多,血管壁不成熟,通透性大,导致对比剂进入血管的速度加快,且分期高的病灶组织新生毛细血管更多,对比剂更易向血管间外隙渗漏[25]。本研究中,DWI联合动态增强扫描诊断宫颈癌ⅠB1、ⅠB2、ⅠB3、ⅡA1、ⅡA2、ⅡB、ⅢB、ⅢC1、ⅣA期的约登指数分别为0.879、0.848、0.469、0.801、0.665、0.985、0.470、0.485、0.784,准确率分别为95.59%、95.59%、94.12%、95.59%、92.65%、98.53%、95.59%、97.06%、97.06%。王静等[26]将DWI联合MRI动态增强扫描用于宫颈癌术前分期诊断发现,不同临床分期宫颈癌患者ADC值、动态增强扫描参数(容量转移常数、速率常数、血管外细胞外容积分数)差异明显,可通过定量参数判断宫颈癌术前分期。将MRI平扫、DWI与动态增强扫描联合应用于宫颈癌分期诊断,能够分辨盆腔内器官、盆腔内壁及子宫组织结构等,还能显示盆腔内淋巴结情况,判断肿瘤大小及转移部位,进一步提高诊断准确率[24]。本研究存在的不足:纳入例数有限,且部分分期宫颈癌患者仅2例,使统计效能降低,后续应扩大样本量,使用MRI参数定量反映病灶分期情况。
综上所述,DWI联合MRI动态增强扫描与宫颈癌FIGO 2018分期诊断一致性较好,诊断准确率较高。
[参考文献]
[1] ARBYN M,SIMON M,PEETERS E,et al. 2020 list of human papillomavirus assays suitable for primary cervical cancer screening[J]. Clin Microbiol Infect,2021,27(8):1083-1095.
[2] SALEHINIYA H,MOMENIMOVAHED Z,ALLAHQOLI L,et al. Factors related to cervical cancer screening among Asian women[J]. Eur Rev Med Pharmacol Sci,2021,25(19):6109-6122.
[3] MOHAMUD A,H?GDALL C,SCHNACK T. Prognostic
value of the 2018 FIGO staging system for cervical
cancer[J]. Gynecol Oncol,2022,165(3):506-513.
[4] PARK B K,KIM T J. Useful MRI findings for minimally invasive surgery for early cervical cancer[J]. Cancers (Basel),2021,13(16):4078.
[5] MAHANTSHETTY U,POETTER R,BERIWAL S,et al. IBS-GEC ESTRO-ABS recommendations for CT based contouring in image guided adaptive brachytherapy for cervical cancer[J]. Radiother Oncol,2021,160(2):273-284.
[6] ZHU Y,SHEN B,PEI X,et al. CT,MRI,and PET imaging features in cervical cancer staging and lymph node metastasis[J]. Am J Transl Res,2021,13(9):10536-10544.
[7] HARRY V N,PERSAD S,BASSAW B,et al. Diffusion-weighted MRI to detect early response to chemoradiation in cervical cancer:a systematic review and meta-analysis[J]. Gynecol Oncol Rep,2021,38(3):883-891.
[8] LU H,WU Y,LIU X,et al. The role of dynamic contrast-
enhanced magnetic resonance imaging in predicting treatment response for cervical cancer treated with concurrent chemoradiotherapy[J]. Cancer Manag Res,2021,13(4):6065-6078.
[9] 胡尚英,趙雪莲,张勇,等. 《预防宫颈癌:WHO宫颈癌前病变筛查和治疗指南(第二版)》解读[J]. 中华医学杂志,2021,101(34):2653-2657.
[10] 鲁琦,张震宇. 国际妇产科联盟2018年版子宫颈癌分期标准的解读[J]. 中华妇产科杂志,2019,54(10):718-720.
[11] LANGBERG G S R E,NYGARD J F,GOGINENI V C,et al. Towards a data-driven system for personalized cervical cancer risk stratification[J]. Sci Rep,2022,12(1):120-126.
[12] TANEJA N,CHAWLA B,AWASTHI A A,et al. Knowledge,attitude,and practice on cervical cancer and screening among women in India:a review[J]. Cancer Control,2021,28:10732748211010799.
[13] LI J,LIU G,LUO J,et al. Cervical cancer prognosis and related risk factors for patients with cervical cancer:a long-term retrospective cohort study[J]. Sci Rep,2022,12(1):139-145.
[14] CHONG G O,PARK S H,PARK N J,et al. Predicting tumor budding status in cervical cancer using MRI radiomics:linking imaging biomarkers to histologic characteristics[J]. Cancers (Basel),2021,13(20):5140-5146.
[15] ZHONG X,ZHANG L,DONG T,et al. Clinical and MRI features of sacral insufficiency fractures after radiotherapy in patients with cervical cancer[J]. BMC Womens Health,2022,22(1):166-175.
[16] QIN F,PANG H,YU T,et al. Treatment strategies and prognostic factors of 2018 FIGO stage ⅢC cervical cancer:a review[J]. Technol Cancer Res Treat,2022,21(3):153-159.
[17] BI Q,BI G,WANG J,et al. Diagnostic accuracy of MRI for detecting cervical invasion in patients with endometrial carcinoma:a meta-analysis[J]. J Cancer,2021,12(3):754-764.
[18] RAMLI Z,KARIM M K A,EFFENDY N,et al. Stability and reproducibility of radiomic features based on various segmentation techniques on cervical cancer DWI-MRI[J]. Diagnostics (Basel),2022,12(12):3125-3131.
[19] 黄文亮. DWI对宫颈癌化疗效果的评价[J]. 中国中西医结合影像学杂志,2019,17(5):464-466.
[20] GAUSTAD J V,ROFSTAD E K. Assessment of hypoxic tissue fraction and prediction of survival in cervical carcinoma by dynamic contrast-enhanced MRI[J]. Front Oncol,2021,11(2):668-674.
[21] 李曼曼,哈传传,谢玉海,等. 多模态磁共振成像对宫颈癌病理分级和分期评估中的应用[J]. 医学影像学杂志,2022,32(9):1551-1554.
[22] QIAN W,LI Z,CHEN W,et al. RESOLVE-DWI-based deep learning nomogram for prediction of normal-sized lymph node metastasis in cervical cancer:a preliminary study[J]. BMC Med Imaging,2022,22(1):221-227.
[23] 王丰,陈士新,付伟,等. MR弥散加权成像结合动态扫描增强在宫颈癌诊断中的临床价值[J]. 医学影像学杂志,2021,31(12):2096-2099.
[24] CAI M,YAO F,DING J,et al. MRI radiomic features:a potential biomarker for progression-free survival prediction of patients with locally advanced cervical cancer undergoing surgery[J]. Front Oncol,2021,11(3):749-756.
[25] 許敏,何永胜,戚轩,等. ADC值和DCE-MRI定量参数对宫颈癌宫旁浸润的判定价值[J]. 医学影像学杂志,2022,32(3):480-483.
[26] 王静,曾小松. 弥散加权成像联合磁共振动态增强扫描在宫颈癌术前分期中诊断价值研究[J]. 临床军医杂志,2021,49(6):713-714.

