Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
Su-Lan Wu, Yi-Qi Chen, Li-Jun Shen, Jian-Bo Mao, Li Lin, Ji-Wei Tao, Huan Chen,Shi-An Zhang, Jia-Feng Yu, Chen-Xi Wang
1Center for Rehabilitation Medicine, Department of Ophthalmology, Zhejiang Provincial People’s Hospital,Affiliated People’s Hospital, Hangzhou Medical College,Hangzhou 310000, Zhejiang Province, China
2The Affiliated Eye Hospital of Wenzhou Medical University in Hangzhou, Hangzhou 310000, Zhejiang Province, China
Abstract
· KEYWORDS: non-contact wide-field viewing system;scleral buckling; silicone oil-filled; retinal detachment
INTRODUCTION
With the development of pars plana vitrectomy (PPV),the reattachment rate of conventional rhegmatogenous retinal detachment (RRD) has exceeded 90%[1], but detachment can recur in some patients after vitrectomy and filling silicone oil (SO) filled[2].The causes of recurrent retinal detachment (re-RD) in SO-filled eyes are mainly as follows[3-4]:proliferative vitreoretinopathy (PVR), non-closure of original breaks, missed new breaks, and insufficient SO filling.The standard surgical method for re-RD in SO-filled eyes is SO removal, retinotomy, preretinal and subretinal proliferative membrane peeling, repositioning of the detached retina after heavy water injection, laser photocoagulation, and repeated SO injection[5].This approach places a significant economic burden on patients, and the inferior periphery of the retina that is not in contact with SO not be attached.Some scholars have tried to treat re-RD in SO-filled with scleral buckling(SB) using binocular indirect ophthalmomicroscope[6-7].However, binocular indirect ophthalmomicroscopes have low magnification and inverted images, which are not convenient for examing the fundus.The procedure is also complicated and difficult to master for young surgeons.We aimed to explore the effectiveness and safety of SB surgery using non-contact widefield viewing system and 23G intraocular illumination for the re-RD in SO-filled eyes.
SUBJECTS AND METHODS
Ethical ApprovalThis retrospective consecutive cohort study was approved by the Ethics Committee of Zhejiang Provincial People’s Hospital (202303102055000128561), and it adhered to the principles of the Declaration of Helsinki.Informed consent was waived due to the retrospective nature of the study.
SubjectsThe study involved 9 patients (9 eyes) with SO-filled eyes who had re-RD between June 2019 and September 2022,and reported to the Zhejiang Provincial People’s Hospital and the Eye Hospital of Wenzhou Medical University.Patients with macular or posterior pole breaks, PVR grade C2 or above,or much preretinal proliferative membrane were excluded.
MethodsThe surgery was conducted under local or general anesthesia by the same experienced surgeon.This surgery was an innovation of the traditional scleral bucking with the assistance of a non-contact wide-field viewing system(Figure 1).The conjunctiva was dissected along the limbus according to the position of the rectus muscle in operation.The rectus muscles were isolated and traction sutures were placed under the insertion of the selected rectus muscle tendon.A 23G cannula was inserted through a trocar 3.5-4.0 mm from the limbus.Under direct visualization through the oculars of the microscope with a wide-field viewing system (MERLIN®Volk Optical Inc.USA; Resight®, Carl Zeiss Meditec AG, Germany) in place, the entire retina was examined, the precise location of the retinal break was marked,and cryopexy or laser photocoagulation was applied around the retinal breaks and lattice degeneration areas.For eyes with marked subretinal fluid (SRF) that affected the cryopexy of the breaks, sclerotomy with choroid puncture fluid drainage was performed.Depending on the condition of the fundus, a small amount of SO was drained from the 23G cannula to increase the height of the band.Encircling or segmental SB was performed to cover the retinal breaks and lattice degeneration areas.SO was removed during this or the subsequent surgery depending on the ocular condition.Patients were followed up at least three months after oil extraction.All patients underwent best corrected visual acuity (BCVA) assessment, tonometry, slitlamp examination, optical coherence tomography, and ultrawidefield fundus photography before and after surgery.The visual acuity was converted to the logarithm of the minimum angle of resolution (logMAR) for analysis.The logMAR equivalents for nonnumeric visual acuities were as follows:counting fingers=1.7 logMAR, hand motion=2.0 logMAR,light perception=2.3 logMAR, and no light perception=3.0 logMAR[8].
Statistical AnalysisGraphpad Prism 7 software was used for statistical analysis.The measurement data were represented as mean±standard deviation, and the count data were represented asn.The rank sum test was used to compare the visual acuity before and after treatment.Statistical significance was denoted by considered at level ofP<0.05.
RESULTS
Six of the patients were male (6 eyes) and 3 were female(3 eyes).The average age was 49.3y (15-73y).The previous disease was RRD for 6 patients, retinal detachment associated with choroidal detachment (RRD-CD) for 1 patient, and hemorrhagic retinal detachment of polypoidal choroidal vasculopathy (PCV) for 1 patient.The average duration from the last vitrectomy was 5.6mo (2-19mo).All patients had inferior retinal detachment without macula involvement, and the PVR did not exceed C1.Eight patients had retinal breaks,and 1 patient had a subretinal membrane without a break.The preoperative mean BCVA logMAR unit was 1.48±0.92 (0.15-3.0)The preoperative intraocular pressure (IOP) was 12.1-39.3 mm Hg.The average axial lengths were 24.95±3.87 mm (21.74-32.4 mm),and pathological myopia was detected in 3 patients.There were 4 patients with intraocular lens (IOL) implantation, 2 patients of aphakia, 3 patients with cataracts, and 1 case of lens subluxation.The basic characteristics of all patients before surgery are presented in Table 1.
No intraoperative or postoperative complications occurred in all patients.Among the 9 patients, a segmental scleral silicon band was placed in 8; an encircling band was placed in patient 5.The retina of patient 3 reattached well after scleral bucking, the SO was removed, and a gas-liquid exchange was performed.SRF was drained through a sclerotomy for patients 6 and 7.A small amount of SO was aspirated from the 23G cannula in patient 5.The mean time of SO aspiration was 2.6mo (0-8mo), and the mean follow-up duration was 8.22mo (3-22mo) after SO aspiration.No patient had re-RD.The details of the surgery are provided in Table 2.The ultrawidefield fundus photography of patient 7 and patient 8 before and after surgery are showed in Figures 2 and 3.
BCVA improved significantly from 1.48±0.92 logMAR(0.15-3.0) at baseline to 0.95±0.64 logMAR (0.1-2.0) at the last visit (P=0.03).Except for patient 7, BCVA improved in all patients.The IOP of patient 1 was 39.3 mm Hg before surgery,and it fluctuate from 30 to 40 mm Hg after SB.Local eye drops failed to control the IOP.We performed SO aspiration 2wk after SB.The IOP decreased to normal.In patient 5, the IOP was approximately 34.8 mm Hg at baseline, but fluctuated to approximately 30 mm Hg after SB.It was subsequently controlled with eye drops after SO removal.In patient 4, the anterior chamber was filled with SO before the surgery, and IOP was high, and uncontrollable with eye drops after SO removal.We performed cyclophotocoagulation, and the IOP finally decrease.The IOP of the other 6 patients was stable before and after surgery; no obvious decrease or increase in IOP was observed.The change of BCVA and IOP were listed in Table 3.
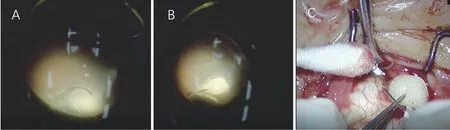
Figure 1 Surgical procedure A: Exploration of the entire retina through the non-contact wide-field viewing system, and localization of the lesion; B: Cryopexy for the lesion; C: SRF drainage via a 1 mL injection syringe.SRF: Subretinal fluid.

Figure 2 Changes of patient 7 before and after surgery A: Retinal detachment in SO-filled eye; a retinal hole inferior.B: Ten days after SB surgery.C: One month after SB surgery.D: One month after SO removal.E: Seven months after SO removal.SO: Silicone oil; SB: Scleral buckling.

Figure 3 Changes of patient 8 before and after surgery A: Retinal detachment in SO-filled eye; subretinal membranes are inferonasal.B:Two days after scleral bucking surgery.C: Three months after scleral bucking surgery.D: One week after SO removal.E: Two months after SO removal.SO: Silicone oil.
DISCUSSION
The success rate of RRD surgery has greatly improved with the adoption of vitrectomy combined with intraocular SO tamponade, but retinal detachment may recurred in some patients.Re-RD typically occurs inferiorly in SO-filled eyes.The opening of previous tears due to inadequately relieved persistent retinal traction, or new tears with recurrent proliferation at the vitreous base PVR and retinalforeshortening are the main causers[6-7].In this study, 8 eyes had retinal holes, 1 eye (patient 8) had no obvious retinal holes, but there was a nasal subretinal membrane, which was considered to be the cause of failure of RD treatment.

Table 1 Characteristics of the patients
The main treatment for re-RD in SO-filled eyes is re-peated vitrectomy with SO removal and elimination of tractions,which usually includes relaxing retinectomy, the use of perfluorocarbon liquids (PFCL), reattachment of the retina, and applying SO or gas tamponade at the end of surgery[9].Ambiyaet al[9]reperformed vitrectomy for 118 patients with re-RD in SO-filled eyes.Of these patients, 64.40% (76/118) had retinal reattachment after local or 180° retinectomy and SO tamponade.However, the surgery was expensive, and patients may have given up due to economic burden.Patients are also more likely to develop PVR due to multiple vitrectomies and wide retinotomy, resulting in re-RD, SO dependence, and low IOP[10-11].Long-term SO tamponade can cause complications,such as corneal endothelium decompensation, secondary glaucoma, retinal toxicity.
SB is a classical surgery for RRD.It can be used for re-RD in patients with SO-filled eyes, whose PVR grades of C1 and below, and mild retinal membrane.For SO-filled eyes, SB can increase the contact between the inferior retina and SO,which helps to release the retina and promote the closure of retinal breaks by the silicone band.Churashovet al[12]treated patients with inferior recurrence of RRD with PPV+SB, PPV,PPV+retinotomy (RT), or PPV+RT+pPFCL.There was no recurrence in the PPV+SB group.The recurrence rate of the PPV+SB group was significantly lower than those of the other groups (P=0.0012).PPV+SB appears to be a more convenient and less complex procedure.However, the number of patients with SO-filled eyes was not established.Weiet al[6]used an encircling band combined with 360° laser photocoagulation using a binocular indirect ophthalmomicroscope for re-RD in SO-filled eyes.However, it is easy to miss retinal breaks, because of the limited clarity of binocular indirect ophthalmomicroscopy for SO-filled eyes, which leads to surgical failure.In addition, re-RD usually presents inferiorly in SO-filled eyes.Then 360° laser photocoagulation is not necessary, and there is no benefit in increasing the reattachment rate[13].Zhanget al[14]achieved a success rate of 90.48% (19/21) for re-RD in SO-filled eyes, using SB with microscopy, but patients with refractive interstitial opacity and small pupils were excluded.A non-contact widefield viewing system has a visual range of 120° and strong penetration, which is not affected by pupil size, and a certain degree of refractive interstitial opacity does not affect the surgery[15].We performed SB with a non-contact wide-field viewing system for 8 patients with SO-filled eyes who sufferedretinal detachment.All of them achieved retinal reattachment.SO was successfully removed, and no retinal detachment occurred.The reason for retinal detachment in 7 patients was a retinal hole or inferior PVR, and we placed a segmental silicon band.Patient 4 had an inferior retinal hole, nasal lattice degeneration, and condensation and photocoagulation scars at the entire peripheral retina.In addition, SO moved into the anterior chamber because of lens subluxation.The cornea was damaged, opacities formed in the optical media.Therefore, we performed encircling SB.We believe non-contact wide-field viewing system assisted SB surgery for retinal detachment in SO-filled eyes has the following advantages[16-17].1) It enables a direct, clear and magnified image of the fundus under an ophthalmic surgical microscope.The entire surgical procedure can be performed under the surgical microscope without wearing a binocular indirect ophthalmoscope.A clear and wide-field image of the peripheral retina helps detect retinal breaks that have not been detected before surgery.2) Small pupil, lens opacity, and capsule opacification do not influence the surgery with the assistance of a wide-field viewing system.3) A 23G cannula can help to remove SO, and facilitate laser photocoagulation.4) SB can increase the contact between the inferior retina and SO, and patients do not need to keep their face-down strictly.5) The visual system provides good visualization to allow young doctors to learn.

Table 2 Surgical details of the patients in this study
In this study, retinal detachment did not involve the macula in all patients.At the last follow-up, the BCVA of most patients were improved, except for patient 7.The previous disease of patient 7 was hemorrhagic retinal detachment caused by PCV, and the scar under the macula affected the BCVA.Three patients suffered high IOP after the surgery, but this was stabilized after treatment with eye drops.The IOP was stable in the remaining 6 patients.No complications such as infection,intraocular hemorrhage or anterior segment ischemia occurred in any patients.
However, it is a retrospective study with a small sample size.Prospective, large-sample randomized controlled studies are needed to verify this treatment for re-RD in SO-filled eyes.In conclusion, for the re-RD in patients with SO-filled eyes, PVR≤C1, few retinal membranes, SB surgery with a non-contact wide-field viewing system and 23G intraocular illumination provides a new safe treatment with a satisfactory success rate.
ACKNOWLEDGEMENTS
Foundations:Supported by National Natural Science Foundation of China (No.81700884); Scientific Research Foundation of National Health and Health Commission(No.WKJ-ZJ-2037); Zhejiang Public Welfare Technology Application Project (No.LGF21H120005); Science and Technology Project of Wenzhou (No.Y20190649).
Conflicts of Interest:Wu SL,None;Chen YQ,None;Shen LJ,None;Mao JB,None;Lin L,None;Tao JW,None;Chen H,None;Zhang SA,None;Yu JF,None;Wang CX,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Algorithm of automatic identification of diabetic retinopathy foci based on ultra-widefield scanning laser ophthalmoscopy
- CD3ε of a pan T cell marker involved in mouse Aspergillus fumigatus keratitis
- Neuroprotective effects of acteoside in a glaucoma mouse model by targeting Serta domain-containing protein 4
- Neuroprotective and anti-inflammatory effects of eicosane on glutamate and NMDA-induced retinal ganglion cell injury
- Bone morphogenetic protein-6 suppresses TGF-β2-induced epithelial-mesenchymal transition in retinal pigment epithelium
- Dry eye rate and its relationship with disease stage in patients with primary hypertension: a cross-sectional study in Vietnam
