Dry eye rate and its relationship with disease stage in patients with primary hypertension: a cross-sectional study in Vietnam
Tran Tat Thang, Pham Hong Phuong, Nguyen Sa Huynh, Nguyen Trung Kien, Nguyen Duy Toan, Nguyen Thi Thu Ha, Le Ha Khoa, Nguyen Huu Dung, Thai Doan Thang,Le Viet Thang
1Nghe An Eye Hospital, Nghe An 43000, Vietnam
2Nghe An Friendship General Hospital, Nghe An 43000,Vietnam
3Military Hospital 103, Ha Noi 100000, Vietnam
4Vietnam Military Medical University, Ha Noi 100000,Vietnam
5Hanoi Medical University, Ha Noi 100000, Vietnam
6Bạch Mai Hospital, Ha Noi 100000, Vietnam
7TTH Vinh General Hospital, Nghe An 100000, Vietnam
Abstract
· KEYWORDS: primary hypertension; dry eye; stage of hypertension; plasma creatinine
INTRODUCTION
Systemic arterial hypertension, is characterized by the continuous elevation of blood pressure within the systemic arteries.This condition is categorized into two types: primary and secondary hypertension[1-2].The intricate pathophysiological mechanisms behind primary hypertension involve genetics, environmental influences, and the intricate interplay of the integrated nervous system.This includes components such as the renin-angiotensin-aldosterone system,the role of natriuretic peptides and the endothelium, the sympathetic nervous system, and the immune system[2-4].
Primary hypertension is a risk factor for and a contributor to various diseases.These include cardiovascular ailments like stroke, coronary artery disease, heart failure, peripheral vascular disease, and conditions like renal disease and hypertensive retinopathy[1,5-7].Hypertensive retinopathy typically advances subtly, often devoid of symptoms, but in severe cases, it can lead to reduced vision, eye swelling, and even double vision[7].
Apart from the aforementioned clinical manifestations,hypertensive patients have also exhibited dry eye (DE),tied to inflammatory immune responses, oxidative stress,retinal impairment, and antihypertensive medications[1,8-10].The implications of DE encompass diminished visual functionality[11], a negative impact on contrast sensitivity[12],the amplification of stray light due to an unstable tear film,and a decrease in contrast sensitivity[13].Nevertheless, research is scarce exploring DE and its related factors in individuals afflicted with primary hypertension.For these reasons, we hypothesized a correlation exists between DE, disease stage,and other factors among primary hypertensive patients.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the Ethics Committee of Nghe An Eye Hospital, approved under decision No.0678/QD-BVMNA.Informed consent was obtained from all the participants.
PatientsA total of 432 patients diagnosed with primary hypertension (144 individuals within each stage) and receiving treatment at Nghe An General Friendship Hospital in Nghe An Province, Vietnam, were enrolled in this study, spanning from January 2021 to January 2023.The classification of hypertensive stages was established based on target organ complications, as defined by World Health Organization criteria[14].Exclusion criteria encompassed patients with inflammatory eye complications, users of contact lenses, and those with a history of eye surgery.Additionally, individuals with acute infections, suspected surgical conditions, and pregnant or lactating women were omitted from the study.A control group of 144 individuals of similar age and sex and confirmed good health through regular health check-ups was also included.Clinical characteristics and laboratory data were gathered at the study’s outset.Expert medical practitioners verified the identification of target organ complications.
Five hundred and seventy-six participants were referred to ophthalmologists to evaluate the occurrence of DE.These individuals underwent the Ocular Surface Disease Index(OSDI) questionnaire and the Schirmer I test (without anesthetics) following standard protocols[15-16].The OSDI questionnaire consists of 12 items, with scores ranging from 0 to 100.Scores of 0-12 indicate the absence of DE, while scores of 13 or higher signify the presence of DE.For scores between 13-22, the condition is categorized as mild DE; 23-32 indicates moderate DE; and 33-100 reflects severe DE[15].DE is established if Schirmer I values are equal to or below 10 mm in at least one eye.The lowest value between both eyes was used for statistical analysis.
Data on the duration of hypertension, treatment specifics(particularly the use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers), and biochemical markers such as urea, creatinine, albumin, protein, and highsensitivity C-reactive protein (CRP-hs) were concurrently collected alongside the Schirmer I test.

Table 1 Comparison of some characteristics and ratio of DE in hypertension group and control group n (%)
Statistical AnalysisThe continuous data from normally distributed sources were characterized using the mean and standard deviation, and they underwent analysis through the Studentt-test.Conversely, data with skewed distributions were described using the median (25thpercentile-75thpercentile)and were subject to analysis through the Mann-WhitneyUtest and the Kruskal Wallis test.Categorical data were displayed in terms of frequency and percentage, and their analysis was carried out using the Chi-square test.We conducted a multivariable-adjusted regression analysis to identify factors independently associated with DE.Statistical analysis was performed using Statistical Package for Social Science (SPSS)version 20.0 (Chicago, IL, USA) with aP-value <0.05 was considered significant.
RESULTS
The results in Table 1 indicate that the patient cohort exhibited a notably higher OSDI score and significantly lower Schirmer I value than the control group, withP<0.001.The prevalence of DE among hypertensive patients surpassed that of the control group (P<0.001).Table 2 shows that parameters such as age, hypertension duration, plasma urea, creatinine, CRPhs, and DE incidence gradually increased in alignment with the severity of the hypertensive stage,P<0.001.Conversely, the utilization rate of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers displayed a progressive decrease with escalating hypertensive stages,P<0.05.
Table 3 underscores that patients afflicted with DE manifested higher levels of age, hypertension duration, diabetic mellitus ratio, plasma urea, creatinine, and CRP-hs when contrasted with those without DE,P<0.05.Interestingly, the study did not identify a significant connection between using angiotensinconverting enzyme inhibitors/angiotensin receptor blockers medications and DE.Upon analysis, advanced age, prolonged hypertension duration,presence of diabetes mellitus, elevated plasma creatinine, and increased CRP-hs levels independently emerged as factors associated with DE in primary hypertension patients,P<0.01.
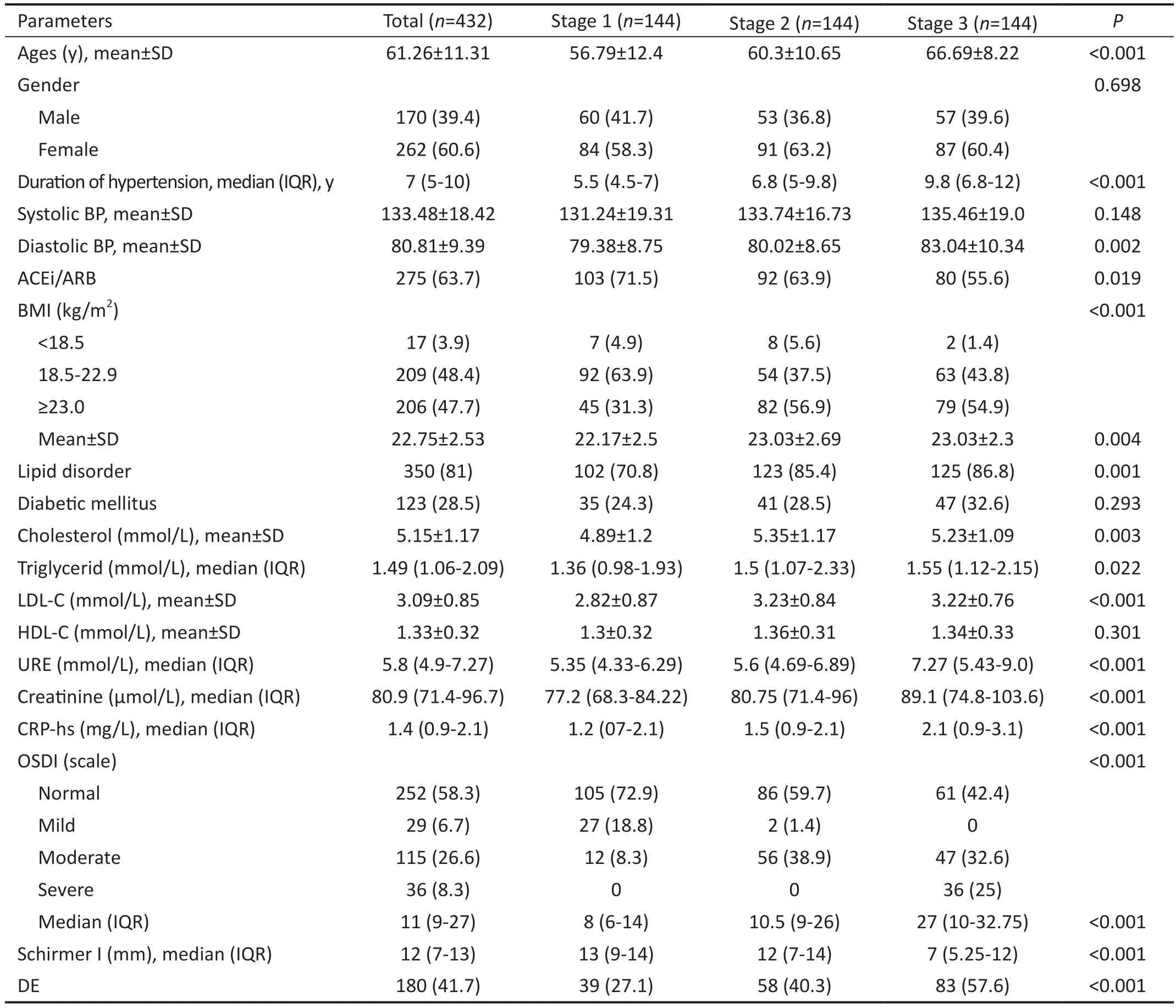
Table 2 Comparison of demographic and laboratory characteristics according to patients with different stages of hypertension n (%)
DISCUSSION
Ratio of Dry Eye in Primary Hypertension PatientsOur study showed up to 41.7% of patients were diagnosed with DE(180/432 patients; Table 1).There are not many studies on DE in primary hypertension patients, but many studies have shown that DE is associated with hypertension in healthy people as well as in people with chronic disease.Marculinoet al[17]studied the rate of DEs and the risk factors in 582 adults.The results showed that the rate of DEs accounted for 24.4%.DEs were more common in the hypertensive group (OR=1.98;95%CI: 1.14-3.43,P=0.015).Ferreroet al[18]found that 34.4%of older people (≥65y) had DEs in a study of 1045 people, and hypertension was an independent factor related,P=0.014.The etiology of DE can vary among individual patients, potentially stemming from factors such as escalated permeability of the tear film and inflammation affecting both the ocular surface and lacrimal gland, as highlighted in reference[19].The role of the inflammatory immune response in the development of DE has more recently been substantiated.This process initiates with the involvement of natural killer cells, which secrete interferon-gamma alongside other proinflammatory cytokines like interleukin-1, interleukin -6, and tumor necrosis factoralpha.These factors prompt the upregulation of antigenpresenting cells at the ocular surface, consequently initiating an adaptive immune response.This response facilitates the infiltration of more inflammatory cells into the ocular surface,damaging its integrity[20].The mechanism underlying ocular damage in hypertensive patients exhibits a connection to ocular hypertension and glaucoma.This linkage arises due to the shared mechanisms and co-occurrence of hypertension and glaucoma[21].Additionally, damage to the retina caused by hypertension and systemic inflammation in hypertensive patients contribute to ocular impairment, ultimately contributing to DE[7,22].Consequently, our study’s findings offer a more lucid depiction of the association between hypertension and DE.
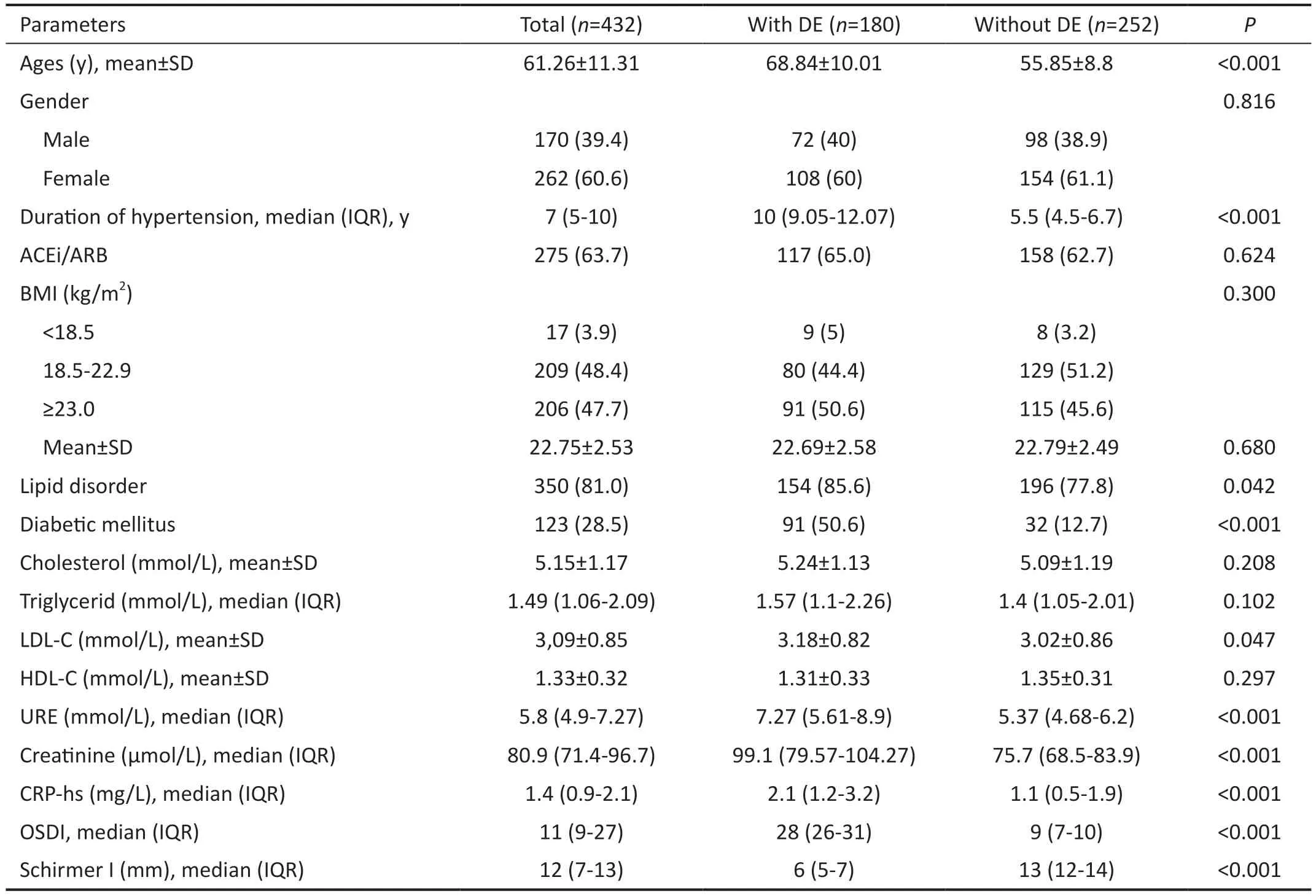
Table 3 Comparison of demographic and laboratory characteristics in primary hypertension patients with and without DE n (%)
Relation Dry Eye and Disease Stage, Some Factors in Primary Hypertension PatientsOur results show that DE was elevated together with the hypertension stage at 27.1%,40.3%, and 57.6%, respectively, for stages I, II, and III,P<0.001.Significantly, the OSDI score gradually increased,and the Schirmer value gradually decreased from the group of hypertensive patients stage I to III,P<0.001 (Table 2).We found that there were some factors related to this result because age, plasma creatinine, and CRP-hs levels increased gradually from the group of patients with stage I to stage III hypertension,P<0.001 (Table 2), that the factors have all been confirmed byprevious studies to be related to DEs[20-23].In multivariate analysis,we found that advanced age, long duration of hypertension,diabetes mellitus, elevated plasma creatinine, and CRP-hs are independent factors associated with DE in patients with primary hypertension,P<0.01 (Table 4).Several factors have been established to cause DE in the elderly, including lack of tears due to low production and evaporation and many abnormalities in the position of the eyelids, causing the tear film to break down more quickly[24-25].DEs, lacrimation,photophobia, burning sensation, and visual dysfunction are common manifestations in diabetic patients[26].CRP-hs is an inflammatory marker, a risk factor, and a predictor for various non-infectious diseases, including cardiovascular diseases such as coronary artery disease, peripheral vascular disease,and atherosclerosis[27].Recently, under the illumination of molecular biology, the primary mechanism of inflammationrelated DE has been confirmed[28-30].Our results demonstrate that inflammation plays a role in the pathogenesis of DE in patients with primary hypertension.
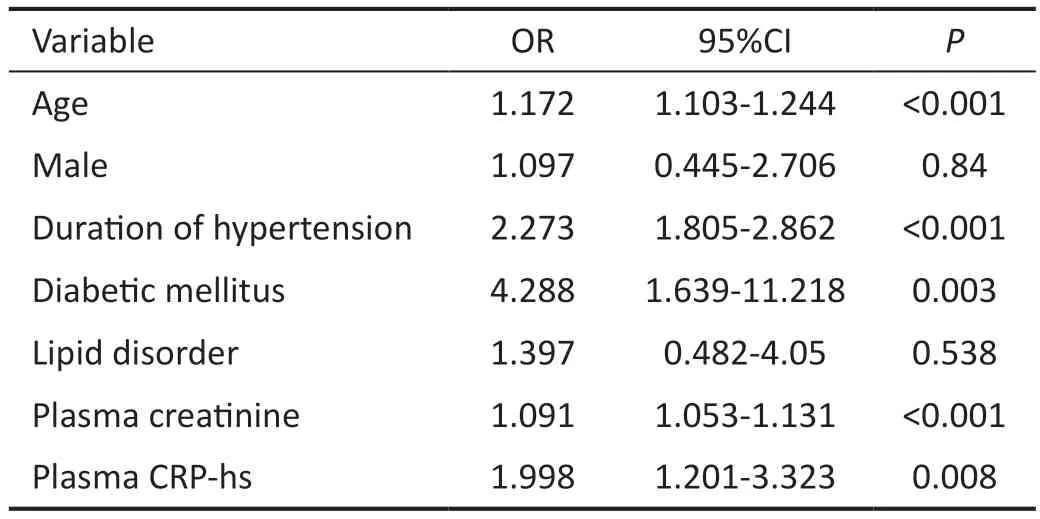
Table 4 Multivariate logistic regression analysis of some clinical variables related to DE in primary hypertension patients
Although the research goal has been achieved, the topic is still limited in some points.First, due to the lack of fluorescence,we could not perform tear film break up time to diagnose DE instead of OSDI and Schirmer test.Second, we could not analyze the relationship between hypertensive retina with DEs and related factors in primary hypertension patients, such as smoking, duration of diabetes, and lifestyle.Finally, the relationship between DEs and some characteristics of patients with primary hypertension had only been described through cross-sectional observations and had not been followed over a long period.
In conclusion, DE is a common disorder in primary hypertension patients, accounting for 41.7% (180/432 patients).Factors associated with DE include advanced age, prolonged disease duration, stage disease, diabetic mellitus, and increased plasma creatinine and CRP-hs levels.
ACKNOWLEDGEMENTS
Conflicts of Interest: Thang TT,None;Phuong PH,None;Huynh NS,None;Kien NT,None;Toan ND,None;Ha NTT,None;Khoa LH,None;Dung NH,None;Thang TD,None;
Thang LV,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Comment on: Recurrence after spontaneous separation of epiretinal membrane in a young woman: a case report
- When to repair a retinal detachment?
- Bilateral iridocorneal endothelial syndrome-Chandler’s syndrome: a case report and literature review
- Penetrating canaloplasty in corticosteroid-induced glaucoma: a report of two cases
- On-spot preparation of EDTA solution for the treatment of band keratopathy: a case report
- Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
