On-spot preparation of EDTA solution for the treatment of band keratopathy: a case report
Yan-Ting Li, Bin Chen, Tian-Hong Wu, Bo Jiang, Yun-Feng Lu
1Department of Ophthalmology, the First Affiliated Hospital of Soochow University, Suzhou 215000, Jiangsu Province, China
2Department of Ophthalmology, Suzhou EENT Hospital,Suzhou 215000, Jiangsu Province, China
Dear Editor,
We report a case of band keratopathy who experienced several ocular surgeries, secondary uveitis and glaucoma which eventually led to severe band keratopathy.We use commonly-used vacuum blood collection tubes with ethylenediaminetetraacetic acid dipotassium salt (EDTA-K2)to prepare chelation solution on-spot to remove the calcium deposits on the corneal surface.It is proved to be relatively safety, efficacy, cost-effective.We obtained the written informed consent from the patient, and this case study is in accordance with the tenets of the Declaration of Helsinki.
CASE PRESENTATION
A 34-year-old man, complained about the left cornea opacity which affected the appearance, came for treatment at March 9, 2023.He accepted par plane vitrectomy with silicone oil tamponade and scleral buckling for traumatic retinal detachment about ten years ago, and then silicone oil removal combined with cataract extraction was performed without intraocular lens implantation.In December 2014, he underwent secondary intraocular lens implantation surgery which was found dislocation in September 2021, then be
repositioned with sclera fixation.Since October 2021, he had
been experiencing recurrent uveitis, secondary glaucoma controlling by brinzolamide and carteolol hydrdchloride eye drops, while ring-shaped lesions occurred in peripheral cornea and became worse.From October 2022, corneal opacity appeared in the palpebral fissure area already affected daily life and work.The right eye kept normal during this period.There was no significant medical history, recent medication history,personal history, or family history.Ophthalmic examination revealed best-corrected visual acuity of 1.0 in the right eye and light perception in the left eye with correction helpless.Intraocular pressure was within normal of both eyes.All ocular examinations of the right eye showed no positive signs.The left conjunctiva exhibited mild congestion, and a horizontal milky-white opacity was observed crossing the palpebral fissure area of the cornea, with the upper and lower cornea remaining transparent (Figure 1A1), and details of fundus was occluded.Pentacam (OCULUS, Germany) revealed irregular corneal topography on the anterior surface with most parameters within the normal range, but central corneal thickness couldn’t be counted accurately showing as the red coding (Figure 1B1).Scheimpflug imaging illustrated strong reflection in the corneal epithelial layer and anterior elastic layer (Figure 1C1).Because of the severe opacification of cornea, there was no result of endo-corneal endoscope.The diagnosis of this patient was band keratopathy in the left eye.Patient underwent ethylenediaminetetraacetic acid (EDTA,C10H16N2O8) chelation therapy on April 18, 2023.Preoperative preparation requisite included six bottles of sterile vacuum blood collection tubes with EDTA-K2 3.6 mg each (BD,Becton Driver, Franklin Lakes, USA), one ampoule bottle of sterile injection water (5 mL), an iris spatula, disposable gelatin sponge swabs, 1 mL sterile disposable syringe, corneal bandage lens (Johnson & Johnson, Oasys), 0.5% levofloxacin eye drops (Santen, Japan).Notice that sterile injection water can’t be replaced by normal saline or other solution because it may lose efficacy that the solute may produce chemical reaction with EDTA-K2.
EDTA Chelation Solution PreparationDraw 1 mL of sterile injection water into a 1 mL sterile disposable syringe,inject it into the first sterile vacuum blood collection tube,shake it vigorously at least 20 times to make sure EDTA-K2 totally dissolved, withdraw the entire solution with a 1 mL syringe, and transfer it to the second sterile vacuum blood collection tube.Repeat this process until the sixth one which is filled with the required EDTA solution for the surgery, with a concentration of approximately 21.6 mg/mL (3.6 mg×6).Meanwhile, the properties of the solution were been tested precisely as the concentration was 15.30 mg/mL, the pH value was 5.8, osmotic pressure is 146 mOsmol/kg.
Surgical ProcedureAfter topical anesthesia, gently scrape the corneal epithelium using an iris spatula.Extract the solution from the sixth tube using a 1 mL disposable syringe and drop it onto a disposable sponge swab.Use the swab to repeatedly rub the corneal opacity for about 10 to 15min until the cornea gradually become transparent and the intraocular condition are clearly visible.After the procedure, apply the corneal bandage lens (Figure 2).
Postoperatively, 0.5% levofloxacin eye drops were prescribed in the left eye four times a day for 1 to 2mo, and kept using anti-glaucoma drops.On the first day after surgery, the patient’s uncorrected visual acuity in the left eye was hand movement in front of the eye, due to the macular scars which could be observed though the pupil using indirect fundus scope.The cornea was transparent with corneal bandage lens covered, so that it could be tell that no significant inflammation in the anterior chamber, the pupil slightly oval, and the intraocular lens in position.About twenty days postoperatively(May 9, 2023), the patient’s uncorrected visual acuity is counting fingers at the front, the cornea is transparent (Figure 1A2), and there was a significant improvement in the aesthetic appearance of the eye.The anterior surface curvature and central corneal thickness on the corneal topography map could be counted and the data was within the reasonable range (Figure 1B2).The Scheimpflug image shows that the central cornea has an almost normal morphology (Figure 1C2),and the intraocular condition was still visible.Endo-corneal endoscope could detect the number of the corneal endothelial cell of 2488/mm2about two months post-operation.As the stubborn inflammation and the exposure of polypropylene suture, mild recovery was appeared after about three months.EDTA eye drops (10 mL:50 mg) was used four times everyday, not only controlled the symptom but also alleviated the cloudy of cornea.
DISCUSSION
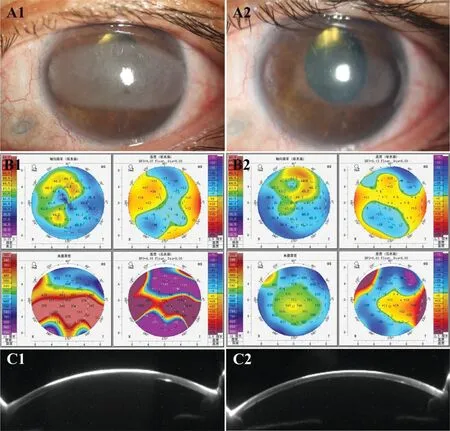
Figure 1 The preoperative and postoperative anterior segment image, corneal topography, and Scheimpflug image of the left eye A1, A2: The preoperative (A1) and postoperative (A2) anterior segment image of the lefteye shows a significant improvement; B1,B2: The preoperative (B1) and postoperative (B2) corneal topography of the lefteye reveals irregularities and error in the anterior surface curvature, which is within the normal range after surgery; C1, C2:The preoperative (C1) and postoperative (C2) Scheimpflug image of the left eye’s anterior segment demonstrates strong reflections in the corneal epithelial layer and anterior elastic layer are essentially normal after surgery eye.

Figure 2 A series of anterior segment image during the surgery A:Preoperative corneal opacity; B: Scrape the corneal epithelium;C: Swab to repeatedly rub the corneal opacity; D: Postoperative,transparent cornea with corneal bandage lens covered.
Band keratopathy is a chronic degenerative corneal disease which is often caused by calcium deposition in the Bowman’s layer[1], as also named calcific band keratopathy (CBK).CBK often occurs secondary to systemic or ocular diseases such as uveitis, hyperparathyroidism, and hypercalcemia due to chronic kidney disease[2-4].The early lesions originate from the peripheral cornea.However, as the lesions progress and involve the pupillary area of the cornea, patients may experience visual impairment and aesthetic concerns[5-6].The treatment of CBK aims to remove the calcific corneal deposits.The main treatment includes mechanical debridement,phototherapeutic keratectomy (PTK), and EDTA chelation therapy[7].EDTA, as a metal ion chelator, can form stable soluble calcium complexes by chelating calcium ions[8],facilitating the elimination of calcium from the cornea.Based on this characteristic, EDTA can be also applied in corneal chemical injuries of lime burn, typically with a concentration of 0.5%[9].However, for CBK, the concentration is usually between 3% and 5%[10].Most patients experience a certain degree of visual improvement after EDTA chelation therapy,and it can also alleviates patient discomfort[3,5,9,11].Furthermore,studies have shown that EDTA has minimal cytotoxicity to corneal cells and, under certain conditions, can promote cell growth[12].Although there is a certain recurrence rate associated with EDTA treatment for corneal band degeneration, retreatment is often unnecessary[9].
In clinical practice, the use of EDTA solution for the treatment of CBK was reported over a decade ago.However, the availability of commercialized EDTA solutions is difficult to purchase, and adjustments in concentration are required before use.Furthermore, there are few commercially available EDTA eye drops, which poses challenges for medical institutions.PTK has become increasingly popular for the treatment of CBK and other superficial corneal diseases.However,PTK is often more expensive, and from a cost-effectiveness perspective, it imposes a significant economic burden compared to the use of EDTA solution on patients with CBK of mild to moderate degree.
The method ascertains the literatures and moderates with advance.But there are still limits that the reason of the inflammation could not be solved so that long-term treatment may be carried out after surgery.The concentration and other properties like pH value, osmotic pressure cannot be acquired precisely because of the inevitable loss during the preparation procedure.As all, from the experience of the present patient,the safety and efficacy of this method have been confirmed.This approach offers advantages such as easy-accessibility,low-cost, and high-safety, thus demonstrating potential for clinical application and promotion.
ACKNOWLEDGEMENTS
Conflicts of Interest:Li YT,None;Chen B,None;Wu TH,None;Jiang B,None;Lu YF,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Comment on: Recurrence after spontaneous separation of epiretinal membrane in a young woman: a case report
- When to repair a retinal detachment?
- Bilateral iridocorneal endothelial syndrome-Chandler’s syndrome: a case report and literature review
- Penetrating canaloplasty in corticosteroid-induced glaucoma: a report of two cases
- Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
- Mesenchymal stem cells for repairing glaucomatous optic nerve
