Penetrating canaloplasty in corticosteroid-induced glaucoma: a report of two cases
Fang Liu, Liu-Shan Zhou, Wei-Wei Zhang
Department of Ophthalmology, Daqing Longnan Hospital, the
Fifth Affiliated Hospital of Qiqihar Medical College, Daqing
163453, Heilongjiang Province, China
Dear Editor,
We have treated two patients of glucocorticoid-induced glaucoma with penetrating canaloplasty (PCP)since 2021.PCP is a new type internal drainage surgery for glaucoma, which is a bleb-independent filtering surgery combined canaloplasty with trabeculectomy, and the surgery shows a great efficacy of intraocular pressure (IOP) reduction with no surgical complication.
PCP surgery started with a fornix-based conjunctival flap and double scleral flap, and Schlemm’s canal was opened,a 10-0 prolene suture was positioned and tensioned within Schlemm’s canal, trabucular meshwork segment was excised and peripheral iridectomy was performed, the scleral flap and the conjunctival flap were closed watertight with 10-0 prolene sutures.
Ethical ApprovalThe study was conducted in accordance with the principles of the Declaration of Helsinki.The informed consent was obtained from the subjects.
Case 1A 47-year-old female with IgG4-related disease was found high IOP for 7mo after taking oral prednisone for 11mo.The patient was previously diagnosed with IgG4-related disease in West China Medical University in July 2020, and was given prednisone 40 mg combined with immunosuppressant orally.In November 2020, when the patient visited the Department of Ophthalmology due to decreased vision, the IOP of both eyes was increased,and fluctuated between 28 and 32 mm Hg.After using two antihypertensive eye drops, the IOP could be controlled at 21.0 mm Hg.The patient’s IOP was not well controlled since March 2021, and the number of antiglaucoma eye drops was increased from 2 to 4.The IOP of the left eye was controllable,but the IOP of the right eye was still not well controlled, and the IOP was 58.8 mm Hg on admission.The patient underwent bilateral lacrimal gland inflammatory pseudotumor resection in 2005 and left parotid gland tumor resection in 2020.She denied the history of hypertension, diabetes, cerebral and cardiovascular diseases, drug and food allergy, trauma,infection, and family history of glaucoma and other family genetic history.The right eye visual acuity 20/500 corrected to 20/50 (-9.50 D), the left eye visual acuity 20/500 corrected to 20/100 (-10.0 D).IOP of the right eye was 58.8 mm Hg,the left eye was 19.4 mm Hg, the upper eyelid was obviously swollen in both eyes, the induration in the lacrimal gland area was palpable, conjunctival hyperemia in the right eye, corneal transparency, deep anterior chamber, mild opacity of bilateral lenses, white optic disc in the right eye, the cup-disc ratio (C/D)was 0.7, peripapillary choroidal atrophy spots were seen, and the macular foveal reflex was positive.IOL-Master showed that the axial length of the right eye was 25.36 mm in the right eye and 25.7 mm in the left eye.The corneal thickness was 474 μm in the right eye and 487 μm in the left eye.Ultrasound biomicroscopy (UBM) showed that the angles of the eyes were open in all quadrants.The angle examination showed that the angles of the eyes were open in all quadrants, and the trabecular pigmentation was grade Ⅱ in gonioscopy.The patient was diagnosed as bilateral glucocorticoid-induced glaucoma; High myopia in both eyes; Cataract in both eyes;IgG4-related disease.PCP surgery was performed in the right eye on June 22, 2021, and the postoperative IOP decreased significantly, with a fluctuation of IOP of 9-13 mm Hg in the right eye for 2y with no antiglaucoma medication (Figure 1),and no filtering bleb was seen for 2y after surgery.The best corrected visual acuity was 20/50 after the operation and 20/20 after surgery of cataract 1y later.
Case 2A 34-year-old male patient was admitted to the hospital on April 25, 2022 due to high IOP for 7y and poor control of IOP in the right eye for 3mo.Seven years ago, the patient was admitted to the Department of Ophthalmology because of eye distensions and discomfort one month after discontinuous using nasal spray of triamcinolone for 3mo.The IOP was 37.0 mm Hg at the time of the visit.The IOP of the right eye was gradually uncontrolled 3mo before admission.The IOP of the right eye was still higher than 48.0 mm Hg after using 4 kinds of antiglaucoma drugs.He denied the history of allergic rhinitis, surgery, hypertension, diabetes, cerebral and cardiovascular diseases, drug and food allergy, trauma,infection, and family history of glaucoma and other family genetic history.Ophthalmic examination: visual acuity of right eye 20/60 corrected to 20/25 (-2.250 D), visual acuity of left eye 20/50 corrected to 20/20 (-2.25 D), IOP of right eye was 42.0 mm Hg and left eye was 22.0 mm Hg, The optic nerve was pale in the right eye, C/D=0.7, left eye optic disc color light red, C/D=0.3.Axial length was 24.50 mm in the right eye and 24.3 mm in the left eye.The Octopus perimeter showed arcshaped scotoma in the nasal inferior side of the right eye, and the left eye was almost normal.UBM showed that the angle of both eyes was open in all quadrants.The angle examination showed that the angles of the eyes were open in all quadrants,and the trabecular pigmentation was grade Ⅱ in gonioscopy.The patient was diagnosed as bilateral secondary glaucoma.On April 27, 2022, he underwent PCP surgery in the right eye.The IOP decreased to 19.0 mm Hg on the first day after surgery, and increased to 37.0 mm Hg on reexamination one week after surgery.The IOP was 12.0 mm Hg with 3 anti-glaucoma medications (brinzolamide and timolol maleate eye drops,0.2% brimondine tartrate eye drops and acetazolamide tablets)3wk postoperative.The IOP was stable after withdrawal.The IOP was stable at 12 to 15 mm Hg one year postoperative(Figure 2) with no antiglaucoma medication, and with no filtering bleb.The postoperative visual acuity showed no change with the preoperative visual acuity.
DISCUSSION
Both patients were younger than 50 years old, and their IOP was still greater than 40 mm Hg after using more than 3 kinds of antiglaucoma eye drops.The first patient had systemic autoimmune disease IgG4-related disease, which required long-term oral corticosteroids, resulting in glucocorticoidinduced glaucoma.In the second patient, topical application of triamcinolone nasal sprays resulted in glucocorticoidinduced glaucoma.It is reminded that not only systemic (oral and intravenous) use of glucocorticoids can lead to steroidinduced glaucoma, but also nasal spray and oral atomization of glucocorticoids and dermal use of glucocorticoids can lead to steroid-induced glaucoma[1].
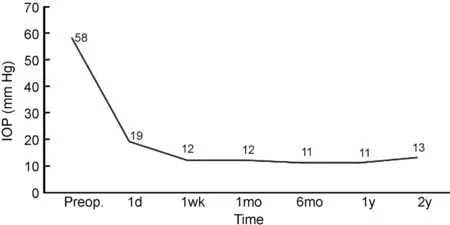
Figure 1 Postoperative intraocular pressure of case 1.
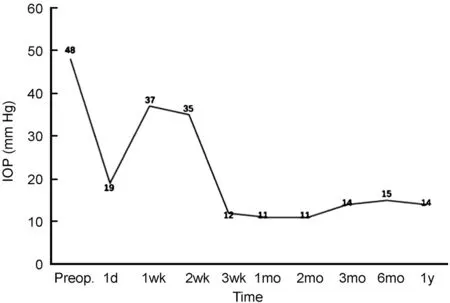
Figure 2 Postoperative intraocular pressure of case 2.
At present, there are three theories about the pathogenesis of glucocorticoid-induced glaucoma: 1) the mucopolysaccharide theory[2-3], 2) the phagocytic cell theory[4], 3) the genetic theory[1-2].The first theory is that glucocorticoids inhibit the secretion of hyaluronidase, which leads to the excessive deposition of mucopolysaccharides in the trabecular meshwork.It leads to increased resistance of aqueous humor outflow from trabecular meshwork.The second theory is that trabecular cells have a phagocytic function, and glucocorticoids inhibit the phagocytic function of trabecular meshwork, resulting in increased resistance to aqueous humor outflow.Both theories suggest that the resistance of glucocorticoid glaucoma lies in the trabecular meshwork.
In recent years, non-filtering bleb dependent new antiglaucoma surgery such as gonioscopy assisted transluminal trabeculotomy, microcatheter-assisted trabeculotomy,Schlemm tube plasty and so on are popular among glaucoma doctors and patients, because there is no need to maintain the filtering bleb for a lifetime, which avoids the dryness of the ocular surface caused by the patients, and avoids the related complications such as filtering bleb infection and leakage[5].PCP surgery introduced by Liang[6], is bleb-independent and does not require antimetabolites.In the operation, suture is implanted into the Schlemm’s canal through a microcatheter to expand the Schlemm’s canal, and the corneoscleral margin is fenestrated, so that the aqueous humor flows directly from the anterior chamber to the broken end of the Schlemm’s canal through the fenestration.It then drains into the eye through the Schlemm’s canal dilated by suture, collecting duct and aqueous humor vein.This surgery solves the problem of outflow resistance of trabecular meshwork due to the opening of trabecular meshwork, and also solves the problem of Schlemm’s canal closure adhesion caused by high IOP, so it can treat open angle glaucoma, including secondary glaucoma,and angle-closure glaucoma[7].This operation really solves the internal drainage essence of trabeculectomy[8].
The surgical procedures of the two patients were performed in accordance with the article on the standard surgical procedure of penetrating canaloplasty by Liang[6]in 2021.The preoperative preparation of PCP was the same as trabeculectomy.The medication used before and after this surgery is the same as trabeculectomy surgery.The most common postoperative complication was microhyphema, which was completely absorbed within 2d after operation in two cases.
The IOP of 2 patients was well controlled by long-term observation (the first patient was followed up for 2y, and the second patient was followed up for 1y).The second patient had transient high IOP (IOP spike) one week after surgery, which returned to normal 1mo after surgery.Transient IOP elevation has also been reported in other glaucoma surgery with Schlemm’s canal, such asab-internocanaloplasty, gonioscopy assisted transluminal trabeculotomy and so on, which may be related to postoperative viscoelastic residue, hyphema and Schlemm’s tube collapse under long-term IOP elevation.Failure of trabecular bypass procedures has been suggested to be due to atrophy of the collector channels secondary to persistent low aqueous outflow.There is a time window for the recovery of the internal drainage pathway of aqueous humor.For these patients, close observation and active reduction of IOP are needed without the need for further intervention, and they will generally return to normal within 3mo[7].
PCP is a new internal drainage procedure for the treatment of glaucoma.Through the treatment of two young patients with glucocorticoid-induced glaucoma, we confirmed the long-term efficacy of PCP in the treatment of glucocorticoidinduced glaucoma[9].A further advantage of this procedure is that neither of the two young patients required filtering bleb maintenance.
ACKNOWLEDGEMENTS
Conflicts of Interest: Liu F,None;Zhou LS,None;Zhang WW,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Comment on: Recurrence after spontaneous separation of epiretinal membrane in a young woman: a case report
- When to repair a retinal detachment?
- Bilateral iridocorneal endothelial syndrome-Chandler’s syndrome: a case report and literature review
- On-spot preparation of EDTA solution for the treatment of band keratopathy: a case report
- Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
- Mesenchymal stem cells for repairing glaucomatous optic nerve
