Prevalence of retinal pathologies in people over 60 years:the Tehran Geriatrics Eye Study
Abolghasem Mortazavi, Alireza Hashemi, Alirerza Jamali, Hassan Hashemi, Mohammadreza Aghamirsalim, Mehdi Khabazkhoob
1Department of Neurosurgery, Sina Hospital, Tehran University of Medical Sciences, Tehran 1416753955, Iran
2Noor Ophthalmology Research Center, Noor Eye Hospital,Tehran 1983963113, Iran
3Rehabilitation Research Center, Department of Optometry,School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran 1545913487, Iran
4Noor Research Center for Ophthalmic Epidemiology, Noor Eye Hospital, Tehran 1983963113, Iran
5Translational Ophthalmology Research Center, Tehran University of Medical Sciences, Tehran 1157715354, Iran
6Department of Basic Sciences, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences,Tehran 1968653111, Iran
Abstract
· KEYWORDS: retinal pathologies; cross-sectional study;vision impairment
INTRODUCTION
The VISION 2020 initiative was launched in 1999 by the WHO in collaboration with the International Agency for the Prevention of Blindness (IAPB) to reduce vision loss[1],which has proved very effective in this regard[2]so that despite a 14% increase in the over-50-year population between 2004 and 2013, the prevalence of blindness has declined by 9%during this time[3].The majority of the measures presented in this initiative are related to diseases of the anterior segment,and the diseases of the posterior segment are ignored in this program despite their non-negligible effects on the community[4]so that Foster and Resnikoff[2]emphasized the need for more focus on cataract, glaucoma, and diabetic retinopathy.
Retinal pathologies are the most important cause of irreversible blindness in developed countries and the second most important cause of blindness in developing countries[5-6].The mean age of the people is increasing in general due to improved health[7], and retinal physiological and pathological changes are one of the consequences of population ageing.Several studies have investigated the prevalence of retinal diseases in different populations.Depending on their design,some studies addressed only one retinal pathology while some other studies evaluated a number of pathologies together,including studies reporting a prevalence of 1.14% for diabetic retinopathy in the general population[8], a prevalence of 6.7%for hypertensive retinopathy (HTR) in the general population[9],and a prevalence of 23.9% for age-related maculopathy(AMD)[10].The results of different studies indicate variations in the prevalence of diseases in various populations, underlining the need for epidemiological studies in this regard; for example, the prevalence of AMD is mentioned from 4.3%[11]to 25.3%[12]in different studies.
Age pyramid changes are suggestive of increased life expectancy and mean age of the general population in Iran[13].Evaluation of different retinal pathologies in the elderly population provides the grounds for planning for supportive or preventive measures.According to this, the present study was conducted to investigate the prevalence of a group of the most important vision-threatening retinal pathologies in subjects over 60y in Tehran, Iran.
SUBJECTS AND METHODS
Ethical ApprovalThe principles of the Helsinki Declaration were followed in all stages of the study.The protocol of the study was approved by the Ethics Committee of the National Institute for Medical Research Development (NIMAD) under the auspices of the Iranian Ministry of Health (ethics code:IR.NIMAD.REC.1397.292).Informed consent was obtained from all participants.
A population-based cross-sectional study was conducted in Tehran, Iran between January 2019 and January 2020.The target population was the above-60-year population of Tehran selected through multistage cluster sampling.
Tehran has 22 municipality districts (22 strata).The over 60-year-old population of each district was obtained from the Statistical Center of Iran and to determine the population that was to be selected from each district proportional to its size.Then, using a block-by-block map Tehran, each block was considered a cluster, and 160 blocks each containing 20 subjects were randomly selected from all 22 districts so that the number of clusters in each district was proportional to its population.After selecting the clusters, a sampling team was dispatched to its address.The first house on the southwest side of the block was considered as the head cluster.The next households were selected in a counter clockwise manner and all individuals above 60y were invited to participate in the study after explaining the objective of the study and assuring them of data confidentiality.This process continued until the required sample size was achieved in each cluster.If the number of eligible people in the last household of a cluster exceeded one person, the cluster could include more than 20 people.If a household was not found, another visit was scheduled (preferably in the same afternoon).Upon willingness to join the study, free-of-charge transportation was arranged to the examination site.
Optometric examinations started with objective refraction using the auto ref/keratometer ARK-510A (Nidek Co.LTD,Aichi, Japan).Then, uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) were measured using the Smart LC 13 LED visual chart (Medizs Inc., Korea) at 6 m.Finally, subjective refraction was measured.
Then, complete slit lamp biomicroscopy including the anterior and posterior segments were done by an ophthalmologist using the B900 biomicroscope (Haag-Streit AG, Bern,Switzerland) and a +90 D lens.Indirect ophthalmoscopy was done to examine the retinal periphery.Slit lamp and retinal examinations were performed half an hour after instilling tropicamide 1% drops (three drops, 10min apart).It should be noted that anterior segment assessment and angle measurement were done before using drops, and tropicamide was instilled in patients without contraindications.All participants underwent corneal imaging using the Pentacam AXL between 9 and 14, biometric components were measured using the IOL Master 500 (Carl Zeiss Meditec, Jena, Germany).Finally, all participants underwent retinal imaging with dilated pupils(using tropicamide 1% drops) by spectral-domain optical coherence tomography (SD-OCT; Heidelberg Engineering,Heidelberg, Germany).
Retinal pathology problems that were investigated in this study were: retinal pigmented epithelium (RPE) change, drusen,geographic atrophy (GA), HTR, nonproliferative diabetic retinopathy (NPDR), proliferative diabetic retinopathy (PDR),choroidal neovascularization (CNV), central retinal artery occlusion (CRAO), myopic retinopathy (MR), branch retinal vein occlusion (BRVO), and central retinal vein occlusion(CRVO).Each evaluated retinal pathology is defined in Table 1[14-24].
Statistical AnalysisThe prevalence of retinal pathologies is reported as percentage and 95% confidence interval.The effect of cluster sampling was considered for standard error calculation.The prevalence of these pathologies was standardized according to the 2019 census using the direct method.Multiple logistic regression analysis was performed to investigate the correlation of demographic and ocular factors with the study variables.
RESULTS
Of 3791 people invited through cluster sampling, 3310 participated in the study (82%), including 1921 females(57.8%).The mean age of the participants was 68.25±6.55(60-97)y.Table 2 presents the prevalence of different retinal pathologies in total population and in each gender; Besides, Table 3 presents the prevalence of these pathologies according to age group.According to Table 2, RPE change was the most common and CRVO, and MR were the rarest pathologies in total population.The relationship between sex and retinal pathologies was evaluated using multiple logistic regression analysis (Table 4).After removing the effect of age, the odds of NPDR were 1.68 times higher in women compared to men(P=0.014).Other pathologies had no significant correlation with gender.According to the results of logistic regression analysis, after removing the effect of sex, the odds of drusen,RPE change, GA, CNV, BRVO and CRVO increased significantly with age.According to Tables 3 and 4, the greatest changes with age were related to GA with odds of 13% for each one-year increase in age so that its prevalence of 1.17%in the age group 60-64y and about 17% in subjects over 80y.Table 5 presents the mean BCVA, intraocular pressure (IOP),and axial length (AL) in subjects with and without retinal pathologies.According tot-test results, BCVA was worse in subjects with all pathologies except HTR compared to participants without retinal pathologies.Moreover, the mean IOP was significantly higher in patients with drusen, RPE change, GA, NPDR, and HTR.The mean AL was significantly shorter in subjects with drusen, NPDR, PDR, regressed PDR and HRT, and significantly longer in subjects with MR.

Table 1 The definition of retinal pathologies
DISCUSSION
The most common pathology was RPE change with a prevalence of 27.42%.This is one of the few studies about the prevalence of RPE change in the elderly population;However, Eleftheriadouet al[25]found that 30% of the patients with AMD had signs of complete or incomplete pigmented epithelium atrophy.In the present study, changes in the density of pigments of the RPE have been investigated as a measure of the presence of changes; RPE pigmentation changes are known as an indicator of AMD progression[15].Our results showed that age had a significant correlation with the prevalence of RPE change; shortening of the RPE microvilli with age is probably due to thinning of this layer[26].Although there are differences among studies regarding changes in the density of RPE cells[27],Jonaset al[28]found that the number of the RPE cells decreased by about 0.3% per each one-year increase in age.

Table 3 The prevalence of types of retinal pathologies in people over 60y by age %
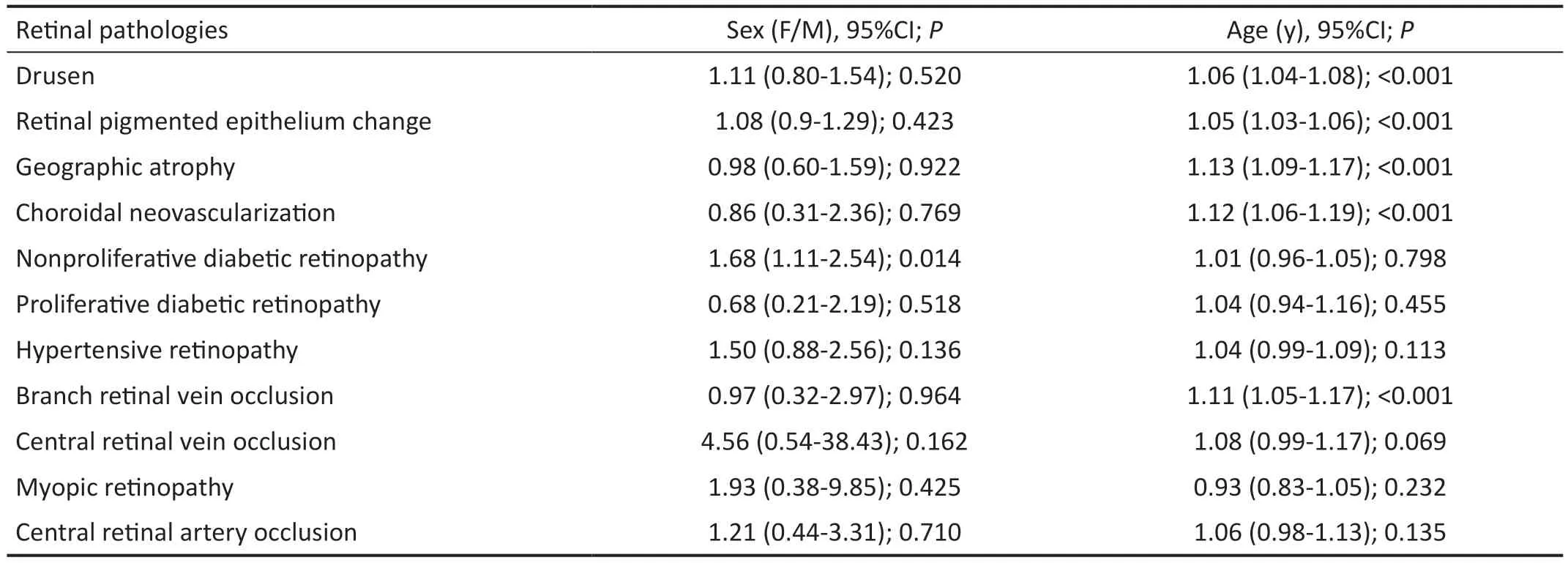
Table 4 Association of types of retinal pathology with age and sex in multiple logistic regressions

Table 5 Comparison of BCVA, IOP, and AL between types of retinal pathology eyes and non-retinal pathology eyes mean±SD
Drusen, as one of the main characteristics of AMD[14], was found on 11.08% of the subjects.Several studies have evaluated the prevalence of drusen in different age groups,including studies reporting a prevalence of 4.3% in the Japanese over-40-year population[11], 10.8% in Americans[29],13.3% in Australian subjects aged above 49y (Blue Mountain study)[30], and 23.9% in Singaporean people above 40y[10].The differences in the results of studies may be related to factors like ethnicity and age range of the participants or definition of drusen so that some studies classified drusen to three groups of distinct soft, indistinct soft, and hard[31]and reported the prevalence according to the type of the study.More recent studies defined a new form of drusen called patchy drusen, which is distinctly different from soft drusen[14]and is commonly found in the eyes of Asian people with exudative maculopathy[32-33].Aging was perhaps the most important determinant of the increase in the prevalence of drusen in the present study, which has a very clear association with an increase in AMD[34].One of the findings of the present study was shorter AL in subjects with drusen compared to participants without it.Similarly, Fraser-Bellet al[34]found that AL had an indirect correlation with the prevalence of soft drusen.In the above study, increased scleral rigidity in shorter ALs[35]was proposed as an effective factor in the relationship between AL and drusen prevalence[34].
The prevalence of GA was 4.52% in the present study.Rimet al[36]reported a prevalence of 0.2%, 0.76%, and 2.75%for GA in Asia, East Asia, and South Asia, respectively.The prevalence of GA was 1.16% in the Blue Mountain study[37]and 0.5% in the Baltimore study[38].Altogether these findings indicate a high prevalence of GA in the Iranian elderly population.Ethnicity is one of the most important reasons for the difference in the prevalence of GA[39].A lower prevalence of GA has been reported in the Asians compared to American and European populations[36].The results showed that ageing was one of the major reasons for an increase in the prevalence of GA, which is consistent with the results of studies conducted by Rimet al[36].Moreover, we observed that AL was longer in eyes with GA compared to eyes without it; this is while Lavanyaet al[40]found that a shorter AL and hyperopic refractive error were related to early AMD.Therefore, it can be concluded that although shorter AL increases the prevalence of early AMD, longer AL in people with late AMD causes an increase in the prevalence of GA.
The prevalence of HTR was 3.03% in the present study.Schusteret al[9]reported a prevalence of 6.7% for mild and 4.0% for moderate HTR in a sample of 15 010 subjects which was higher than our results.The prevalence of HTR is reported in two forms in different studies: a percentage of the whole population like the present study and Shusteret al’s[9]study or a percentage of hypertensive subjects like the study of Chenet al[41].Chenet al[41]reported a prevalence of 57.08%for grade 1, 14.97% for grade 2, 2.36% for grade 3, and 0.03%for grade 4 HTR in 9793 subjects with hypertension.The prevalence of HTR was 12.9% in Babol, Iran in a study by Rasoulinejadet al[42]and 5.4% in Bangladesh in a study by Akhteret al[43]; all of these results indicates lower prevalence of HTR in the present study.According to the present study,AL was shorter in patients with HTR compared to subjects without it.Leeet al[44]found that the thickness of the retinal nerve fiver layer reduced in subjects with hypertension, high myopia, or a combination of both.On the other hand, one of the most disputable findings of the present study was the higher visual acuity of the subjects with HTR compared to participants without it, while retinal changes in the presence of HTR increase the odds of reduced visual acuity[45].Therefore,it can be concluded that shorter AL in subjects with HTR is probably associated with less changes of the retinal nerve fiber layer, resulting in lack of any disturbances in the visual acuity of these subjects compared to people with other retinal pathologies.
The prevalence of NPDR and PDR was 4.05% and 0.54% in the present study, respectively.Hashemiet al[46]conducted a review study and reported a global prevalence of 4.37% and 0.72% in the general population and 24.78% and 4.14% in the diabetic population for NPDR and PDR, respectively.In another review study, Songet al[8]reported a prevalence of 0.90% for NPDR and 0.07% for PDR in China.Therefore,although the prevalence of NDPR and PDR is higher in Iran compared to China, it is almost similar to the global average.Our results show that the mean AL was shorter in subjects with NPDR and PDR compared to those without these conditions.Studies[47-49]also reported similar findings.The effective factor in the relationship between AL and diabetic retinopathy is not yet clear[47]; however, studies on eyes without retinal problems have shown that the vascular endothelial growth factor density reduces in longer eyes, which could affect this relationship[50].Finally we observed that the odds of NPDR was higher in women, which could be related to the shorter AL in women compared to men[51].
The prevalence of BRVO and CRVO was 0.49% and 0.19%in the present study.Rogerset al[52]reported a total prevalence of 0.442% for BRVO and 0.08% for CRVO in a review study in 2011.These values were 0.64% and 0.13% in a review study by Songet al[53]in 2019, respectively.Comparison of these reports suggests that despite an increase in the global prevalence of CRVO over the past 10y, its mean prevalence is higher in Iranian adults compared to the global average.However, the prevalence of BRVO was lower in the study population compared to the global average in 2019[53].One of the reasons for this difference could be that Rogerset al[52]and Songet al[53]presented the prevalence of BRVO and CRVO in subjects aged over 30y; as mentioned earlier, ageing is one of the most important determinants of the increase in the prevalence of BRVO and CRVO.This relationship was also reported by Rogerset al[52]and Songet al[53].The results of the present study showed longer AL in subjects with BRVO compared to those without it while participants with CRVO had shorter AL.Nonetheless, Szigetiet al[54]and Tsaiet al[55]found shorter AL in both CRVO and BRVO.The reasons for this difference could be the AL measurement method and the presence of absence of macular edema, which may affect measurements[56].
The prevalence of CNV was 0.82% in the present study.Williset al[57]reported a prevalence of 0.017% for CNV in American people over 18y and 0.0079% in the over 65-year population.The majority of the studies presented the prevalence of CNV in patients with pathological myopia[58]; for example, Wonget al[59]reported a prevalence of 5.2%-11.3% in different ethnic populations and Zaouret al[60]reported a prevalence of 6.2% in the Canadian population.The above values indicate that a higher percentage of the Iranian elderly population had CNV.In addition to ethnicity, one of the most important risk factors of CNV is age so that its prevalence was much higher in the over-80-year population compared to the age group 60-64y in the present study.Williset al[57]also found similar results and argued that the retinal degeneration due to ageing was probably effective in increasing the prevalence of CNV with age.
The prevalence of MR was 0.2% in the present study,which was lower than its prevalence in Chinese people over 30y (0.9%)[61], Australian subjects over 49y (1.2%)[62], and Chinese subjects aged over 40y (2.3%)[63].The prevalence of MR is reported to be 0.17% in Indian subjects aged over 30y[28].One of the reasons for the variation in prevalence of MR is the difference in the prevalence of myopia between different populations and ethnic groups so that studies have shown a higher prevalence of myopia in the Asian elderly population[64-65].The lower prevalence of MR in the present study compared to other regions is related to the lower prevalence of myopia in the elderly population of Iran[66].An interesting finding of the present study was the effect of AL on MR so that the mean AL was 27.82 mm in subjects with and 23 mm in subjects without MR.Hashimotoet al[67]found that men and women with AL values of 25.9 and 25.3 mm or more should be further investigated for myopic maculopathy changes.Altogether, our results indicate high prevalence of some retinal diseases in elderly population of Iranian society, this issue shows the importance of conducting regular periodical retinal examinations of the elderly and performing the necessary therapeutic interventions.
ACKNOWLEDGEMENTS
Foundation:Supported by National Institute for Medical Research Development (NIMAD) Affiliated with the Iranian Ministry of Health and Medical Education (No.963660).
Conflicts of Interest: Mortazavi A,None;Hashemi A,None;Jamali A,None;Hashemi H,None;Aghamirsalim M,None;Khabazkhoob M,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Algorithm of automatic identification of diabetic retinopathy foci based on ultra-widefield scanning laser ophthalmoscopy
- CD3ε of a pan T cell marker involved in mouse Aspergillus fumigatus keratitis
- Neuroprotective effects of acteoside in a glaucoma mouse model by targeting Serta domain-containing protein 4
- Neuroprotective and anti-inflammatory effects of eicosane on glutamate and NMDA-induced retinal ganglion cell injury
- Bone morphogenetic protein-6 suppresses TGF-β2-induced epithelial-mesenchymal transition in retinal pigment epithelium
- Dry eye rate and its relationship with disease stage in patients with primary hypertension: a cross-sectional study in Vietnam
