Guiding function of positron emission tomographycomputed tomography examination in the diagnosis and treatment of ocular adnexal mucosa associated lymphoid tissue lymphoma
Xuan Zhang, Qi-Han Guo, Rui Liu, Jing Li, Ying-Chao Li, Jian-Min Ma
1Beijing Ophthalmology and Visual Sciences Key Laboratory,Beijing Tongren Eye Center, Beijing Tongren Hospital, Capital Medical University, Beijing 100005, China
2Tai’an City Central Hospital, Qingdao University, Tai’an 271000, Shandong Province, China
Abstract
· KEYWORDS: ocular adnexal mucosa associated lymphoid tissue lymphoma; positron emission tomographycomputed tomography; ocular tumors
INTRODUCTION
Ocular adnexal lymphoma (OAL) is the most common malignant tumor of the eye in adults, with involvement of the conjunctiva, eyelids, orbit, and any soft tissues within the orbit.It accounts for approximately 8%-20% of ocular adnexal tumors[1-2]and 10.33%-49% of malignant eye tumors[3-5].Ocular adnexal mucosa associated lymphoid tissue lymphoma (OAML) represents the most common pathological subtype of OAL[6-7].Most mucosa associated lymphoid tissue(MALT) lymphomas have a relatively favorable prognosis,but a minority of cases experience recurrence, dissemination,and even progression to higher-grade invasive lymphomas,with localized tumor recurrence, extraorbital spread, and transformation associated with poorer outcomes[8-10].Positron emission tomography-computed tomography (PET-CT) imaging has shown potential in the detection, staging, diagnosis,and treatment of ocular tumors[11-12], although its application in OAML patients has been relatively limited.In recent years, there has been a gradual increase in the incidence of OAML, particularly in Asian countries, where the incidence is significantly higher than that in Western countries[13-14].This study collected clinical data and postoperative PET-CT findings from 21 OAML patients in China to explore the role of PET-CT in the diagnosis and treatment of OAML.
SUBJECTS AND METHODS
Ethical ApprovalThe study adhered to the principles of the Declaration of Helsinki and was approved by the ethics committee of Beijing Tongren Hospital (TRECKY2019-093).All patients were informed about the purpose of the histopathological examination and provided informed consent by signing a consent form.
Data CollectionThis study was a retrospective clinical case study.Clinical data of 21 patients diagnosed with OAML through histopathological examination at Beijing Tongren Hospital Eye Center between October 2017 and September 2021 were collected.
MethodsDetailed medical records of OAML patients were collected and documented, including patient sex, age at onset,affected eye, ocular symptoms, primary site, postoperative PET-CT findings, standardized uptake value (SUV), treatment regimens, and prognosis.All patients underwent tumor resection and were histopathologically confirmed to have OAML.Based on the postoperative PET-CT findings, patients were further categorized into either a residual observation subgroup, residual treatment subgroup, non-residual observation subgroup, or non-residual treatment subgroup based on the treatment regimen.The treatment outcomes were analyzed for different patient groups to explore the role of PET-CT in the diagnosis and treatment of OAML.
All PET-CT scans were evaluated for metabolic activity, and an SUV equal to or greater than 2.5 was defined as indicative of malignancy (PET-CT-positive), indicating increased metabolism.Conversely, if no metabolic elevation was observed on PET-CT or if the SUVmax value was less than or equal to the background activity, the result was defined as benign (PET-CT-negative)[15-17].
Statistical AnalysisStatistical analysis was performed using SPSS 26.0 (IBM Corporation, Armonk, NY, USA).Descriptive statistical methods, including frequency distribution,percentages, and medians, were used to analyze the clinical characteristics of OAML and PET-CT findings.Independentsamplet-tests were used for normally distributed continuous variables, while non-parametric tests were used for nonnormally distributed continuous variables.The Chi-squared tests or Fisher’s exact test were used for categorical variables.P<0.05 was considered statistically significant.
RESULTS
Clinical PresentationAmong the 21 patients with OAML,there were nine men (42.8%) and 12 women (57.2%), for a male-to-female ratio of 3:4.The age of onset ranged from 28 to 74y, with a median age of 52y.Among the affected eyes,eight cases (38.1%) involved the left eye, four cases (19.1%)involved the right eye, and nine cases (42.8%) involved both eyes.Ocular symptoms included eyelid swelling in 12 cases(57.1%), masses in eight cases (38.1%), and proptosis in one case (4.8%).The tumors were located in the conjunctiva in nine cases (42.8%), the orbit (excluding the lacrimal gland) insix cases (28.6%), the lacrimal sac in one case (4.8%), and the lacrimal gland in five cases (23.8%; Table 1).

Table 1 Clinical characteristics of 21 patients with ocular adnexal mucosa associated lymphoid tissue lymphoma
Positron Emission Tomography-Computed Tomography FindingsAll 21 OAML patients underwent PET-CT examinations within 1-2mo after tumor resection.The results were as follows: two patients exhibited both local ocular metabolic elevation and systemic metastasis, and one of these patients had cervical lymph node metastasis (SUVmax=7.96;Figure 1A, 1B), while the other had submandibular and parotid gland metastasis (SUVmax=3.45; Figure 1C, 1D).Nine patients showed only local ocular metabolic elevation, while 10 patients had no abnormal metabolic activity locally (Table 2).The primary site involvement and local metabolic results in the 21 OAML patients were as follows (Table 3): among the nine patients with conjunctival involvement, six showed no local metabolic elevation, while three exhibited local metabolic elevation.Among the seven patients with orbital involvement,three showed no local metabolic elevation, while four exhibited local metabolic elevation.Four patients had involvement of the lacrimal gland, with two showing no local metabolic elevation and two showing local metabolic elevation.One patient had involvement of the lacrimal sac with local metabolic elevation.Treatment and PrognosisAmong the 21 OAML patients, two with systemic metastasis continued to receive chemotherapy.Among the nine patients with only local ocular metabolic elevation, five continued to receive radiotherapy, one continued to receive chemotherapy, and three were under observation.Of the 10 patients with no abnormal metabolic activity locally,two were under observation and eight still continued to receive radiotherapy to reduce the risk of recurrence.
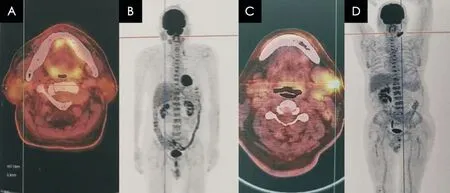
Figure 1 PET-CT findings A, B: PET-CT images showing cervical lymph node metastasis.C, D: PET-CT images showing submandibular-gland metastasis.
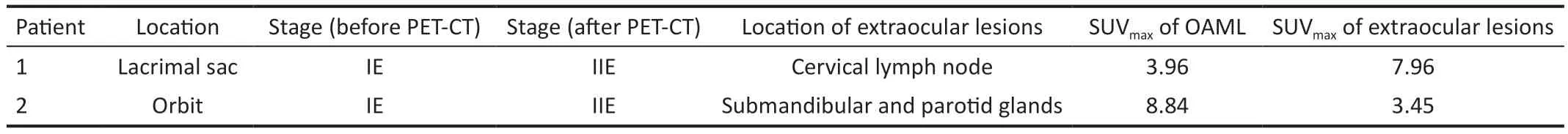
Table 2 PET-CT results in patients with systemic metastases
All enrolled patients underwent tumor resection and were histopathologically confirmed to have OAML.The decision for further treatment or observation was made based on postoperative PET-CT findings, the impact of treatment on organ function, patient preferences, and consultation with hematologists.Based on the postoperative PET-CT findings,patients were divided into a residual group (10 cases) and a non-residual group (11 cases).Subsequently, they were further categorized into a residual observation subgroup (3 cases),residual treatment subgroup (8 cases), non-residual observation subgroup (2 cases), and non-residual treatment subgroup (8 cases), respectively.In the residual observation subgroup,one patient experienced recurrence in the conjunctiva 3mo after surgery.There were no recurrences in the non-residual observation subgroup.In the residual treatment group, one patient experienced recurrence in the lacrimal gland 79mo after surgery.In the non-residual treatment group, two patients experienced recurrence in the conjunctiva 48mo after surgery(Table 4).
All 21 OAML patients had primary lymphoma without secondary or concurrent lymphomas in other parts of the body.Among them, five (23.8%) underwent surgery alone, 13(61.9%) received surgery combined with radiotherapy, and three (14.3%) received surgery combined with chemotherapy(Table 5).All patients were followed up on over a periodranging from 8 to 79mo, with a median follow-up period of 16mo.Four cases experienced recurrence, while no deaths were reported by the follow-up deadline of March 31, 2022.
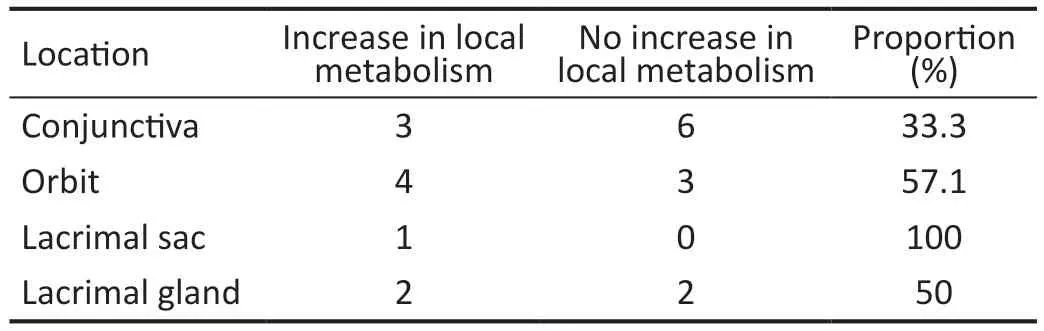
Table 3 Locations and local metabolism of 21 patients with ocular adnexal mucosa associated lymphoid tissue lymphoma
DISCUSSION
PET-CT examination is a novel imaging modality that combines PET, representing functional metabolic imaging,with CT, representing anatomical imaging.It involves the administration of a trace amount of positron-emitting radiopharmaceuticals and uses PET to determine their distribution in various organs of the body.By employing computed tomographic techniques, PET-CT examination displays the physiological and metabolic functions of major organs in the body with precise anatomical localization[18].While PET-CT examination has been widely used in the detection, staging, diagnosis, and treatment of tumors, coronary artery atherosclerosis, and neurological diseases, its application in ocular tumors has only recently gained attention.PET-CT examination has shown potential in the detection, staging,diagnosis, and treatment of ocular tumors[11-12], although its application in OAML has been less frequently reported.In the present study, clinical data and postoperative PET-CT findingsfrom 21 OAML patients in China were collected to analyze the treatment outcomes of different treatment regimens based on postoperative PET-CT findings and explore the role of PET-CT examination in the diagnosis and treatment of OAML.

Table 4 Prognoses of 21 patients with ocular adnexal mucosa associated lymphoid tissue lymphoma
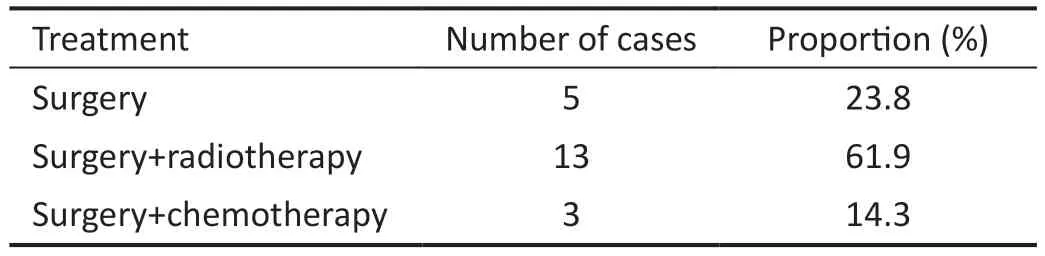
Table 5 Treatment of 21 patients with ocular adnexal mucosa associated lymphoid tissue lymphoma
Clinical Presentation of Ocular Adnexal Mucosa Associated Lymphoid Tissue LymphomaOAML is a slow-growing indolent tumor that primarily affects the ocular adnexa,including the orbit, conjunctiva, lacrimal gland, and eyelids,with rare involvement of extraocular muscles and the lacrimal sac.Most OAML cases are confined to the ocular tissues,although some cases may be associated with extranodal MALT lymphoma in other sites.OAML predominantly occurs in men,with a median age at onset ranging from 41 to 72y[7,19].In the present study, there were nine male and 12 female patients;thus, men accounted for 42.8% of the study population.The age of onset ranged from 28 to 74y, with a median age of 52y.OAML typically affects a single eye, with the orbit being the most commonly involved site, followed by the conjunctiva,eyelids, and lacrimal gland.Extensive involvement of multiple ocular adnexal sites can occur, with an involvement rate of greater than 40% for the orbit, 35%-40% for the conjunctiva,10%-15% for the eyelids, and less than 10% for the lacrimal gland, respectively[6-7].In the present study, the rates of involvement were 42.8% for the conjunctiva, 28.6% for the orbit, 4.8% for the lacrimal sac, and 23.8% for the lacrimal gland.The higher proportion of women and greater rate of conjunctival involvement in our study might have been influenced by the small sample size.
Role of PET-CT Examination in the Diagnosis and Treatment of OAML
Value of PET-CT examination in the diagnosis of OAMLThe clinical advantages of PET-CT examination are demonstrated in the following aspects[20]: 1) Improved localization of metabolic activity in normal and abnormal tissue structures; 2) Better differentiation of inflammatory lesions from PET-negative lesions visible on computed tomography (CT); 3) Detection of incidental abnormalities and determination of their benign or malignant nature; 4) Precise localization for biopsy and radiation therapy targeting.Experts have suggested incorporating PET-CT examination into routine assessments before lymphoma treatment[21].However, PETCT’s diagnostic value is higher for Hodgkin’s lymphoma (HL)and early-stage aggressive non-Hodgkin’s lymphoma (NHL),but lower for indolent NHL.Therefore, we do not recommend PET-CT examination as a routine examination for OAML.
In clinical practice, due to the low malignancy of OAML, the uptake of18F-FDG may be reduced, leading to false-negative results.Typically, physical examinations, blood tests, magnetic resonance imaging (MRI), CT, bone marrow biopsy, and other methods are used for diagnosis.PET-CT examination serves as a supplementary tool for detecting systemic lesions.
Controversy still exists regarding the application of PET-CT examination in patients with MALT lymphoma due to the physiological uptake of18F-FDG.Albanoet al[22]analyzed 32 studies of PET-CT examination in MALT lymphoma patients,revealing variations in18F-FDG avidity depending on several factors such as the primary site, tumor size, morphological features, Ki-67 score, and clinical stage.Mastuoet al[23]reported four cases of OAML, where PET-CT examination after initial surgical resection showed abnormal18F-FDG uptake, later confirmed as MALT lymphoma upon further surgery, indicating that even small and thin conjunctival lesions can be detected by PET-CT examination.
Value of PET-CT examination in initial staging and treatment strategy of OAMLDifferent malignancy grades and sites of involvement in OAML may warrant various treatment approaches and combinations, with a generally favorable prognosis for most patients.Nevertheless, the evaluation of different therapeutic modalities for OAML requires multicenter prospective studies to establish a comprehensive guiding protocol.
Parket al[24]conducted a retrospective analysis of PET-CT examination in 123 histologically confirmed OAML patients,excluding MALT lymphomas originating from the conjunctiva.Among 50 patients with non-conjunctival OAML evaluated,they measured the SUVmax and PET parameters of all lesions and compared them with the sensitivity of MRI in detecting primary tumors.The results revealed that 83.3% of nonconjunctival OAML cases exhibited18F-FDG uptake positivity,and the detection rate was similar to that of orbital MRI.PETCT examination detected extraocular lesions in 14% of OAML patients, leading to a change in treatment approach from radiotherapy to chemotherapy in six cases.Without PET-CT examination, these extraocular lesions would have remained undetected and untreated.Therefore, PET-CT examination plays a certain role in the initial staging and treatment strategy formulation for patients with non-conjunctival OAML.
In the present study, PET-CT findings of 21 patients were analyzed: two patients showed not only increased local ocular metabolism but also distant metastases, with one patient having neck lymph node metastasis (SUVmax=7.96) and another having submandibular and parotid gland metastases(SUVmax=3.45).Based on the information provided by PET-CT examination, the staging changed from IE to IIE due to suspected residual disease, and both patients underwent chemotherapy.Among the nine patients with only increased local ocular metabolism, five received radiotherapy, one underwent chemotherapy, and three opted for follow-up observation.Ten patients exhibited no abnormal metabolic activity in the local region, with two choosing follow-up observation and the remaining eight receiving radiotherapy to reduce the risk of recurrence.These findings suggest that PET-CT examination contributes to accurate staging of OAML patients and facilitates the formulation of personalized treatment strategies, thereby improving patient prognosis.
Value of PET-CT examination in the evaluation of treatment efficacy for OAMLMost primary OAML cases manifest as localized lesions, with approximately 5% involving lymph nodes and 10%-15% showing systemic involvement[25].PET-CT examination, through the quantitative analysis of metabolic activity, can provide valuable information for evaluating OAML treatment efficacy and prognosis.Studies have suggested that SUVmax not only serves as a prognostic indicator but also correlates well with clinical TNM staging[26].SUVmax is a novel prognostic factors, aims to stratify highrisk groups and develop individualized treatment plans based on patients’ actual conditions.Although both TNM and CT have been used for prognostic evaluation, they cannot accurately reflect the radiotherapy effects due to variations in tumor radiosensitivity.In contrast, PET-CT examination reflects tumor functional changes at the molecular level,enabling earlier and more accurate assessment of the treatment response[27].
Fujiiet al[28]conducted a retrospective analysis of nine patients with confirmed OAL through histopathological examination.PET-CT scans were performed before and after treatment, and the18F-FDG uptake in the ocular adnexa and systemic disease sites was assessed using a 5-point Deauville scale.Among the nine enrolled patients, eight showed significant reductions in SUVmax in the ocular adnexa after treatment, and seven patients exhibited complete metabolic response in the ocular adnexa with the first post-treatment18F-FDG uptake, which was associated with improved clinical ophthalmic symptoms and no recurrence in the ocular adnexa.It was concluded that PET-CT examination facilitated the evaluation of treatment response in OAL; however, this method may be influenced by histopathological type and lesion location.
In the present study, all patients underwent tumor resection and were diagnosed with OAML based on histopathological examination.Follow-up observation or further treatment was determined based on factors like postoperative PET-CT results,the impact of further treatment on organ function, patient preferences, and consultations with hematologists.One patient in the residual observation group experienced recurrence in the conjunctiva 3mo after surgery, while no recurrence was observed in the non-residual observation group.Separately, one patient in the residual treatment group experienced recurrence in the lacrimal gland 79mo after surgery, and two patients in the non-residual treatment group experienced recurrence in the conjunctiva 48mo after surgery.As of March 31, 2022,the follow-up period ranged from 8 to 79mo, with four cases of recurrence and no deaths.Among the four recurrent cases,three involved the conjunctiva as the primary site, while one involved the lacrimal gland as the primary site, suggesting that the conjunctiva is prone to recurrence in OAML patients.Patients in the non-residual observation group showed the best outcome, with no cases of recurrence, while the non-residual treatment group included two cases of recurrence, both in the conjunctiva.This further confirms that the conjunctiva is a common site for recurrence in OAML patients.It also demonstrates that PET-CT examination can detect the presence of residual lesions and recurrence after surgery, clarify the extent of lesion involvement, and guide the need for further treatment.
Limitations of PET-CT examination in the application of OAML18F-FDG is associated with glycolysis, and falsepositive results can occur in cases of inflammatory reactions,infectious lesions, recently biopsied or necrotic lymph nodes,and radiation-induced lesions[29].Increased local metabolism of18F-FDG is not a specific change in tumor cells, which limits the specificity of PET-CT examination and its ability to detect small lesions.Additionally, PET-CT examination is expensive and considered a self-paid service, which can be challenging for economically disadvantaged patients to afford.
Tregliaet al[30]conducted a meta-analysis of 376 patients with MALT lymphoma, reporting a detection rate of 71%for PET-CT examination in MALT lymphoma patients.This finding suggests that the use of PET-CT examination can more objectively assess metabolic imaging in clinical research on MALT lymphoma.In the present study, the PET-CT examination results of 21 OAML patients showed that the proportion of increased metabolism in the conjunctiva was the lowest.Whether this is related to the insufficient display of small lesions by PET-CT examination or whether the small sample size needs to be expanded to confirm the results requires additional investigation.
LimitationsThis study is conducted using a retrospective design, which may introduce recall bias and relies on existing medical records that may be incomplete or have variations in data quality.In addition, this study has a small sample size and further expansion of the sample size is needed.However,considering the rarity of OAML, the sample size of this study has some explanatory significance.The prognosis of OAML is generally good, so we only perform PET-CT examination for special populations such as patients with large tumors, more adhesion to surrounding tissues or recurrence, which can better assist in judging the prognosis.
In conclusion, OAML exhibits diverse clinical manifestations,and its diagnosis should be based on the integration of clinical, radiological, and histopathological findings to avoid misdiagnosis.PET-CT examination can provide evidence for the clinical diagnosis of OAML and plays a role in initial staging and treatment strategy formulation.It also provides valuable information for evaluating treatment efficacy and prognosis.Finally, PET-CT examination could lead to changes in the clinical staging of OAML, assist in radiation therapy or chemotherapy, enable timely adjustment of treatment plans,improve patient prognosis, and observe the presence of residual lesions and recurrence after surgery to guide the need for further treatment.However, considering its high false-positive rate, we recommend performing PET-CT examinations only on patients who have received histopathological diagnosis confirming OAML, thereby improving the diagnostic accuracy and reducing patients’ medical expenses.This study had a small sample size and significant heterogeneity, and we look forward to future multicenter, multidisciplinary, large-sample,and prospective studies.
ACKNOWLEDGEMENTS
Authors’ contributions:Zhang X and Guo QH analyzed and wrote the manuscript; Liu R, Li J and Li YC helped collect the data; Ma JM read and revised the manuscript.All authors critically read and edited the manuscript.All authors read and approved the final manuscript.
Foundations:Supported by the Beijing Science and Technology Rising Star Program-Cross-cooperation Project(No.20220484218); the Tai’an City Science and Technology Innovation Development Project (No.2021NS207).
Conflicts of Interest: Zhang X,None;Guo QH,None;Liu R,None;Li J,None;Li YC,None;Ma JM,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Algorithm of automatic identification of diabetic retinopathy foci based on ultra-widefield scanning laser ophthalmoscopy
- CD3ε of a pan T cell marker involved in mouse Aspergillus fumigatus keratitis
- Neuroprotective effects of acteoside in a glaucoma mouse model by targeting Serta domain-containing protein 4
- Neuroprotective and anti-inflammatory effects of eicosane on glutamate and NMDA-induced retinal ganglion cell injury
- Bone morphogenetic protein-6 suppresses TGF-β2-induced epithelial-mesenchymal transition in retinal pigment epithelium
- Dry eye rate and its relationship with disease stage in patients with primary hypertension: a cross-sectional study in Vietnam
