Aflibercept combined with triamcinolone acetonide in the treatment of diabetic macular edema: optical coherence tomography and optical coherence tomography angiography
De-Shuang Li, Hong-Xia Liao, Chuan-He Zhang, Jian-Guo Huang, Wei Chen, Jing-Lin Zhang,Bo Qin
1Shenzhen Aier Eye Hospital, Aier Eye Hospital, Jinan University, Shenzhen 518031, Guangdong Province, China
2Department of Ophthalmology, the University of Hong Kong-Shenzhen Hospital, Shenzhen 518000, Guangdong Province,China
3Guangzhou Aier Eye Hospital, Jinan University, Guangzhou 510040, Guangdong Province, China
Abstract
· KEYWORDS: diabetic macular edema; optical coherence tomography; optical coherence tomography angiography; hyperreflective foci; subretinal fluid; foveal avascular zone; aflibercept
INTRODUCTION
Diabetic retinopathy (DR) is the most common microvascular complication in diabetic patients and is also one of the main causes of vision loss and blindness worldwide[1].DME is a type of DR that can cause central vision loss in diabetic patients.High blood glucose levels in diabetic patients can lead to microvascular damage in the retina, ultimately resulting in retinal ischemia and hypoxia,and activating inflammatory pathways by releasing various cytokines such as vascular endothelial growth factor (VEGF)and interleukin-6[2-3].In diabetic macular edema (DME), the loss and dysfunction of pericytes around capillaries lead to breakdown of the blood-retinal barrier, causing leakage of fluid, protein, and lipids into the retina.These changes result in progressive thickening of the retina and painless vision loss.Although macular edema is reversible in the early stages, longterm edema can lead to ischemia and atrophy of the retinal photoreceptors and retinal pigment epithelium (RPE).If the lesion involves the fovea, permanent vision loss may occur[4-5].Therefore, early detection, diagnosis, and treatment of DME are crucial for controlling disease progression and improving visual function.
Optical coherence tomography (OCT) and OCT angiography(OCTA) are the main non-invasive methods for evaluating retinal microstructure and microvascular pathological changes.They can help locate areas of abnormal retinal thickening,show the spatial distribution characteristics of retinal vessels,and even detect preclinical retinal vascular abnormalities.Furthermore, they can provide detailed information on specific morphological changes in DME[6].Therefore, OCT and OCTA parameters play key role in the diagnosis, monitoring,prognosis, treatment, and long-term follow-up of DME.
Although intravitreal injection of anti-VEGF drugs is currently the preferred treatment for DME[7], its efficacy varies among patients, and some patients show poor response to anti-VEGF treatment or develop DME again after anti-VEGF treatment[8-9].The presence of heightened levels of inflammatory cytokines within the ocular region of patients diagnosed with DME provides evidence to support the notion that inflammation may play a role in the development and progression of DME[10-11].Corticosteroids can effectively treat DME[12],but the complications caused by intravitreal injection of corticosteroids cannot be ignored[13-14].Hence, developing safe and effective combination therapies targeting various pathways related to the pathogenesis of DME may help provide more effective individualized treatment for DME patients and reduce the global burden of vision loss caused by diabetes.
This study investigated changes in the number of HRF and SRF height assessed by OCT and OCTA in 76 eyes of DME patients before and after treatment, with a focus on those treated with aflibercept in combination with triamcinolone acetonide (TA).
SUBJECTS AND METHODS
Ethical ApprovalFrom January 2023 to August 2023,a prospective study was conducted at Shenzhen Aier Eye Hospital and received approval from the Ethics Committee of the hospital (2023-KY014-01).The study adhered to the Declaration of Helsinki, and all participating patients provided their informed consent.
SubjectsBetween January 2023 and August 2023, a cohort of 65 patients (76 eyes) diagnosed with DME and visiting Shenzhen Aier Eye Hospital Affiliated with Jinan University were recruited for the study.The patients were allocated to two groups, aflibercept group (39 eyes) and aflibercept combined with TA group (37 eyes), using a random number table method.The patients received either intravitreal injection of aflibercept or intravitreal injection of aflibercept combined with subtenon’s injection of TA.Inclusion and exclusion criteria and detailed injection methods were same as mentioned in the previous study[15].
Test IndicatorsAll patients underwent ophthalmic examinations one day before surgery and one month after each treatment, including: 1) intraocular pressure using a noncontact tonometer; 2) best-corrected visual acuity (BCVA),with the results converted to logarithm of minimum angle of resolution (logMAR) visual acuity; 3) detailed examination of the anterior segment of eye using a slit lamp; 4) the vitreous and retina using a slit lamp and a 90-D lens after sufficient dilation; 5) central macular thickness (CMT),number of hyperreflective foci (HRF), height of subretinal fluid (SRF) using OCT, and foveal avascular zone (FAZ) area,superficial capillary plexus (SCP) using OCTA.Changes in these indicators before and after treatment were observed and analyzed for their correlation to evaluate treatment effectiveness.
Optical Coherence TomographyOCT was performed using the Spectralis SD-OCT (Heidelberg Spectralis,Heidelberg, Germany).CMT was automatically calculated by the instrument in central horizontal and vertical OCT scans passing through the fovea.The presence of SRF and HRF was also evaluated in these scans.HRF included hyperreflective spots with a size of 20-40 μm, with reflectivity similar to that of the nerve fiber layer.HRF in the entire retina within a 6-mm length were manually counted.The height of SRF under the fovea was manually measured using Image J software.
Optical Coherence Tomography AngiographyOCTA(CIRRUS HD-OCT, Carl Zeiss Meditec Inc, Dublin, CA,USA) was used to perform three horizontal and vertical cross scans in a 3 mm×3 mm area of the macular region using the AngioPlex mode.The collected retinal and choroidal blood flow images were analyzed using the built-in software of the system.The images of SCP were converted into 8-bit grayscale images using Image J software.The SCP was selected to measure the FAZ area because of its clearer structure and vascular contour, which is closer to the anatomical concept of FAZ.All patients underwent a thorough examination conducted by the same qualified and experienced ophthalmologist(Figure 1).
Statistical AnalysisAll data were analyzed using SPSS 26.0 statistical software.Data are described as mean±standard deviation (SD).Independent samplet-tests were used to compare the differences between two groups.Pairedt-test or Wilcoxon sign rank-sum test was used for intra-group comparison.P-value of less than 0.05 was considered statistically significant.

Figure 1 Diagrammatic representation displaying the measured parameters A: Representative images with SRF and HRF.The double-headed arrows indicate the SRF; The red arrow indicates the HRF.B: The red circle represents the FAZ area.HRF: Hyperreflective foci; SRF: Subretinal fluid; FAZ: Foveal avascular zone.
RESULTS
The baseline age, sex, BCVA and various macular measurements showed no significant differences between the two groups before treatment (Table 1).After every treatment,there was a statistically significant difference in BCVA(logMAR) between the two groups (Table 2).
After the first treatment, the CMT of patients in the aflibercept and the combination group were 378±25.51 and 357±22.60 μm,respectively (t=3.26,P<0.01).After the second treatment,the CMT of the two groups were 333±24.55 and 311±25.34 μm,respectively (t=3.07,P<0.01).However, after the third treatment, the CMT of the two groups were 294±18.78 and 295±16.92 μm, respectively, with no statistically significant difference (t=-0.16,P=0.875; Table 3).
The number of HRF (1mo: 7.41±8.25vs10.86±7.22,P=0.027;2mo: 5.33±6.13vs9.12±8.61,P=0.034; 3mo: 3.58±3.00vs6.37±5.97,P=0.007; Table 4) and height of SRF (1mo:82.39±39.12vs105.77±42.26 μm,P=0.011; 2mo: 36.84±10.02vs83.59±37.78 μm,P<0.01; 3mo: 11.57±3.29vs45.43±12.60 μm,P<0.01; Table 5) in combined group were statistically significant less than aflibercept group after each injection,while the area of FAZ showed no significant change before and after treatment in both groups (Table 6).No injection-related complications were observed in either group of patients during the treatment period.
DISCUSSION
DME is considered to be the involvement or near involvement of the central fovea due to abnormal accumulation of fluid in the macula, which leads to macular thickening in DR[16].The pathogenesis of DME begins with retinal hypoxia,which causes high permeability of retinal capillaries, and impaired vascular autoregulation leading to increased intravascular pressure[16].Hypoxia-induced upregulation of VEGF is considered the primary cause of increased capillary permeability, which plays a significant role in the pathogenesis of DME[17].Currently, intravitreal injection of anti-VEGF has become a first-line treatment for DME.Anti-VEGF drugsTable 2 BCVA after 1, 2, 3mo injections in two groups mean±SD, logMAR can not only improve the retinal function and morphology of DME patients, but also prevent further development of DME[7].Despite the effectiveness of anti-VEGF injections,some patients exhibit an unsatisfactory response.The results of Diabetic Retinopathy Clinical Research (DRCR) Retina Network Protocol T indicate that a significant proportion of patients (31.6%-65.6%) continue to suffer from persistent edema even after multiple intravitreal injections of anti-VEGF therapy[9].It has been suggested that factors other than VEGF may contribute to the occurrence and development of DME.Numerous studies have shown that in addition to VEGF, the pathogenesis of DR and DME is also significantly influenced by immunological and inflammatory mechanisms[18-20].
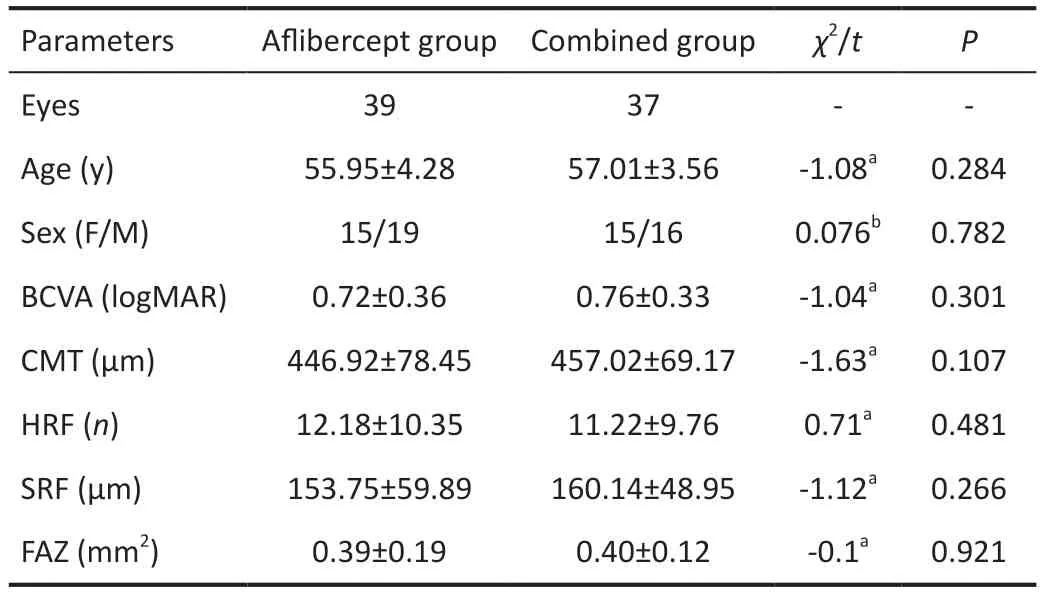
Table 1 The baseline characters of the affected eyes in two groups mean±SD

BCVA: Best-corrected visual acuity.
OCT and OCTA are the main non-invasive methods used to evaluate retinal microstructural and microvascular pathologicalchanges in DME.HRF are defined as independent, welldefined, artifact-free, circular or elliptical high-reflectivity signal points scattered throughout the retinal layers on OCT,with a maximum diameter of approximately 20-50 μm[21].Leeet al[21]suggested that HRF are produced by the abnormal deposition of lipoproteins in the retina due to the breakdown of the blood-retinal barrier caused by various factors.Vujosevicet al[22]believed that the formation of HRF is closely related to the activation and accumulation of retinal microglia or retinal inflammatory reactions caused by monocyte-macrophages from the blood.In animal models, when the retinal barrier is damaged, microglia are activated and migrate from the inner to the outer layers of the retina[23].Therefore, HRF observed using OCT or OCTA in DME patients are considered to be biomarkers of active inflammatory cells.
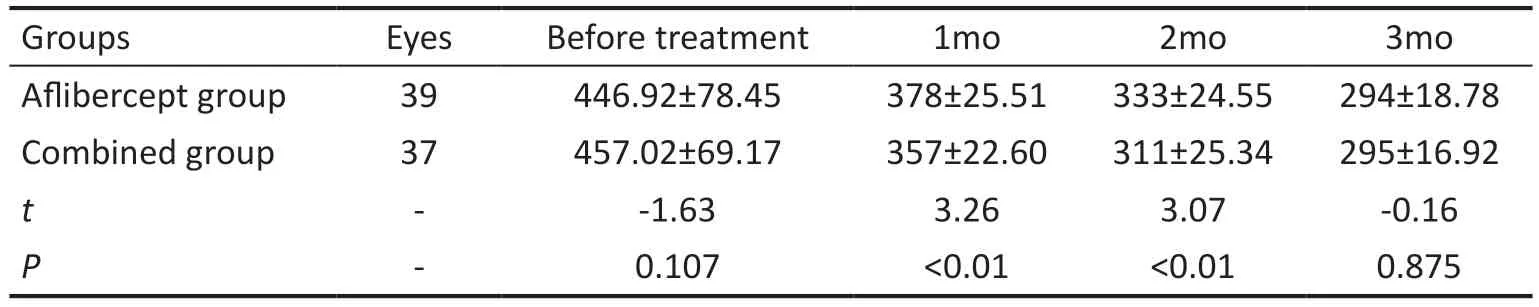
Table 3 CMT after 1, 2, 3mo injections in two groups mean±SD, μm
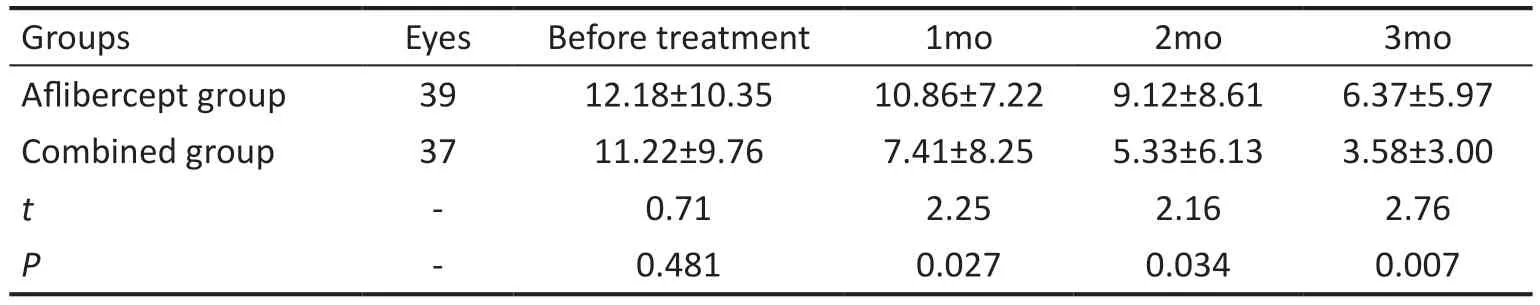
Table 4 The number of HRF after 1, 2, 3mo injections in two groups mean±SD
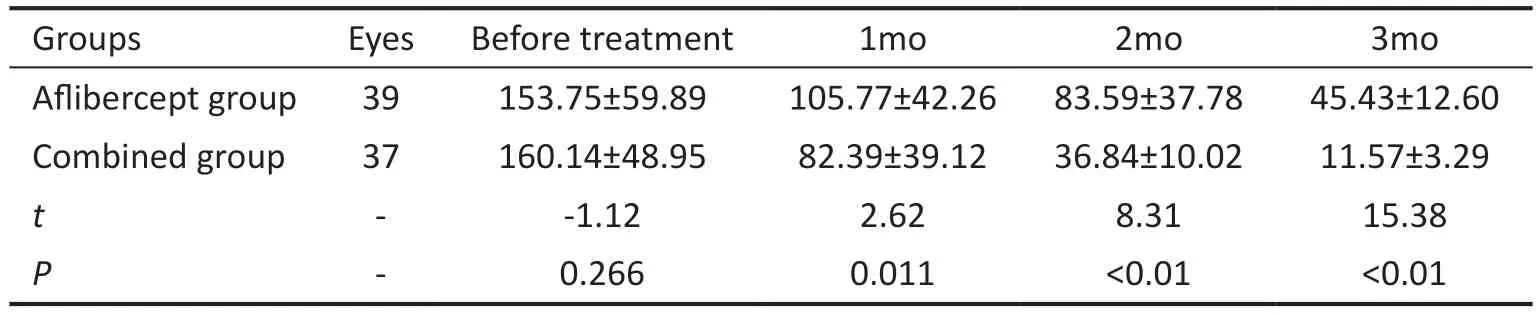
Table 5 Height of SRF after 1, 2, 3mo injections in two groups mean±SD, μm
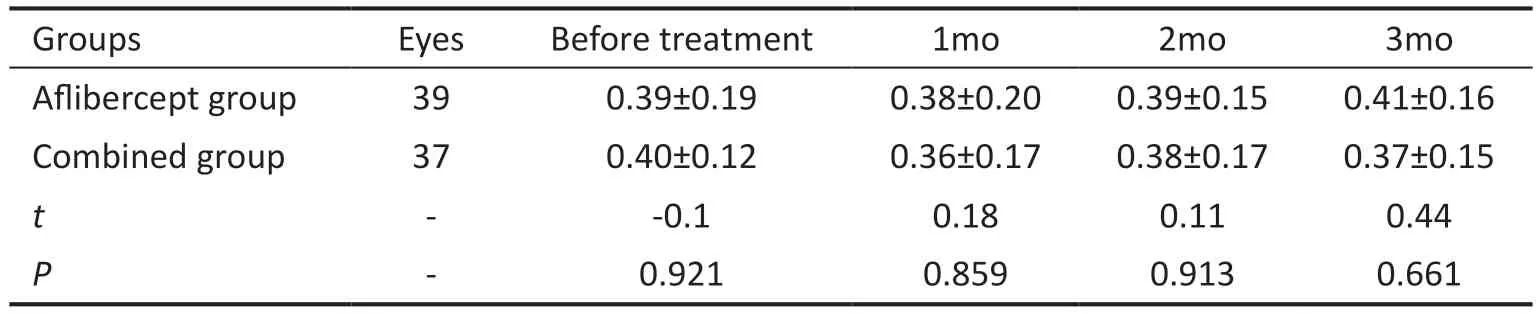
Table 6 Area of FAZ after 1, 2, 3mo injections in two groups mean±SD, mm2
There is a lack of consensus regarding the source of SRF in patients with DME.Some studies have shown that SRF originates from dysfunction of the RPE barrier caused by chronic oxidative stress and metabolic stress[24].Other studies have suggested that the accumulation of SRF usually indicates dysfunction of the RPE, including disruption of the outer blood-retinal barrier and defects in the drainage system and pump function of the RPE[25].This dysfunction is related to the release of pro-inflammatory factors, enhanced permeability mediated by VEGF, protein hydrolysis induced by matrix metalloproteinases, and regulation of cytoskeletal proteins[26].In our study, DME eyes with two OCT biomarkers, SRF and HRF, achieved better results with combination therapy.The differences in the reduction in the number of HRF and the height of SRF between the combination therapy group and the aflibercept group were statistically significant.
The FAZ is the area of the retina that is most closely related to central vision and its function is directly related to visual prognosis.OCTA can not only quantify the area of the FAZ,but also monitor and follow up on abnormal changes in the FAZ.AttaAllahet al[27]used OCTA to evaluate macular perfusion in patients with simple DME and moderate to severe non proliferative diabetic retinopathy.They compared the vascular density and FAZ area of the macular region in diabetic patients with DME, diabetic patients without DME, and healthy controls.The results showed that the vascular density of the deep capillary plexus was significantly decreased in the diabetic patients with DME compared to the diabetic patients without DME and the control group, while the FAZ of the superficial capillary plexus was significantly enlarged.Nizawaet al[28]studied changes in the microvasculature of the macula in DME patients after intravitreal injection of bevacizumab and found indistinct differences in FAZ area or vascular density in different retinal capillary layers in comparison with baseline.Malagolaet al[29]reported that after intravitreal injection of aflibercept to treat DME (observation time points were 3-25mo), there was no significant change in retinal microvascular density.The results of Zhanget al[30]showed that the FAZ area and retinal capillary density may not change significantly in the short term after receiving anti-VEGF therapy.In our study, there was no significant change in FAZ area in either the combination therapy group or the aflibercept group, which is consistent with the results of the above studies.This study has several limitations including relatively inadequate sample size, short-term tracking in patients’treating progress and assess of effectiveness.Besides, OCTA strongly relies on immobility of patient, minor changes may cause different results in the statistical analysis between the two groups.Consequently, it is imperative to conduct largescale multicenter studies to elucidate the long-term efficacy of aflibercept in combination with TA for the treatment of DME.In addition, it is worth noting that OCTA is incapable of detecting active leakage that can be observed through fundus fluorescein angiography.Therefore, further studies are needed to combine OCTA with other examination methods, such as fundus fluorescein angiography.
In summary, our study results suggest that HRF and SRF may be considered as inflammation-related biological markers in DME patients, and the number of HRF and the height of SRF are associated with visual prognosis in DME patients.Therefore, for DME patients who have such biological markers, the effect of anti-VEGF drugs combined with TA treatment is better than that of anti-VEGF monotherapy.
ACKNOWLEDGEMENTS
Authors’ contributions:Li DS and Qin B designed,performed and analyzed the experiments, wrote the paper.Li DS, Liao HX, Zhang CH, Huang JG, and Chen W carried out the data collection and data analysis.Zhang JL and Qin B conceived and coordinated the study, revised the paper.The work reported in the paper has been performed by the authors,unless clearly specified in the text.
Foundations:Supported by the Natural Science Foundation of Guangdong Province, China (No.2022A1515010742);Hunan Provincial Natural Science Foundation of China(No.2023JJ70039); Scientific Research Program of Xiangjiang Philanthropy Foundation.
Conflicts of Interest: Li DS,None;Liao HX,None;Zhang CH,None;Huang JG,None;Chen W,None;Zhang JL,None;Qin B,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Algorithm of automatic identification of diabetic retinopathy foci based on ultra-widefield scanning laser ophthalmoscopy
- CD3ε of a pan T cell marker involved in mouse Aspergillus fumigatus keratitis
- Neuroprotective effects of acteoside in a glaucoma mouse model by targeting Serta domain-containing protein 4
- Neuroprotective and anti-inflammatory effects of eicosane on glutamate and NMDA-induced retinal ganglion cell injury
- Bone morphogenetic protein-6 suppresses TGF-β2-induced epithelial-mesenchymal transition in retinal pigment epithelium
- Dry eye rate and its relationship with disease stage in patients with primary hypertension: a cross-sectional study in Vietnam
