Sutured scleral fixation of existing subluxated/dislocated acrylic one-piece intraocular lenses
Wei-Yu Huang, Yung-Jen Chen
1Department of Ophthalmology, Chi Mei Medical Center,Tainan City 710, Taiwan, China
2Department of Ophthalmology, Chang Gung Memorial Hospital, Kaohsiung City 833, Taiwan, China
Abstract
· KEYWORDS: intraocular lens dislocation; intraocular lens subluxation; lens dislocation; lens subluxation; scleral fixation
INTRODUCTION
Various techniques have been published regarding intraocular lens (IOL) implantation without support of capsule in those experienced trauma or complex cataract surgery.There are numerous ways to implant an IOL,including insertion in the posterior chamberviasutured or sutureless scleral-fixated IOLs or in the anterior chamber with an anterior chamber IOL (ACIOL) or iris-fixated IOLs.Potential complications related to open-loop ACIOLs currently still occur, such as endothelial cell loss, glaucoma, cystoid macular edema, hyphema, and uveitis[1].Modern iris-fixated IOLs may still result in some complications, including pigment dispersion, peripheral anterior synechia formation, papillary distortion, and chronic iritis[2].Implantation of posterior chamber intraocular lenses (PCIOLs)viascleral fixation techniques remains a generally preferable management in eyes with lack of capsular support.These scleral fixation techniques make IOLs able to be placed in the posterior chamber through sutured or sutureless scleral-fixated IOLs.
Acrylic one-piece PCIOLs are recognized as some of the most widely used for IOL implantation.However, trauma,pseudoexfoliation, or zonular dehiscence may dislocate any style of IOL.Sutureless scleral fixation of IOL techniques[3-4]such as embedding haptics of IOLs cannot be applied to most acrylic one-piece PCIOLs.In addition, the position of existing subluxated or dislocated IOLs with or without medium opacity may interfere with the predicted refraction for IOL exchange.Various suture techniques have been published to rescue subluxated/dislocated IOLs[5-8].The purpose of the current case series was to provide our surgical methods and to determine the refraction error in cases after transscleral fixation of existing subluxated or dislocated acrylic one-piece PCIOLs.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by Chang Gung Medical Foundation Institutional Review Board(No.202300881B0).All investigations in this study adhered to the tenets of the Declaration of Helsinki.The need for informed consent was waived by the Institutional Review Board of Chang Gung Medical Foundation because of the retrospective nature of the study.
A consecutive series of patients who experienced a surgery of sutured existing subluxated or dislocated IOLs from October 2018 to June 2020 were enrolled in our study, retrospectively.We documented comprehensive preoperative and postoperative ophthalmologic examinations in all patients, including age,sex, surgical indications, best-corrected visual acuity (BCVA),refractive error, and intraocular pressure (IOP).The BCVA was measured using a Landolt C acuity chart and the presence of intraoperative and postoperative surgical complications was recorded.
All surgical procedures were performed by a single surgeon(Chen YJ), and the general surgical approach of conventional 23-gauge standard three-port pars plana vitrectomy with the infusion cannula set at the 4-o’clock position was performed to operate the subluxated or dislocated acrylic one-piece IOLs in all patients.After removing retained lens nucleus (patient No.4) and all the vitreous surrounding the subluxated or dislocated IOL and discarded capsule, the IOL was grasped using intraocular forceps and brought into the anterior chamber.A Toric lens marker was used to make surgical markings at the 2- and 8-o’clock positions of the limbus.Limited conjunctival limbal peritomies and two 3×3-mm partial thickness triangular sclera-based scleral flaps were created with relaxing radial incisions at the 2- and 8-o’clock positions.A multiplane 2.75-mm limbal incision was created at the 11-o’clock position using a keratome, and one of the IOL haptics was then externalized through the incision.A straight needle of 10-0 polypropylene (blue monofilament,30 cm, Alcon®, Pennsylvania, USA) double-armed suture(straight needle and 1/2-circle needle) and 27-gauge needle were passed through the scleral beds below the flaps, 1.5 mm posterior to the limbus.After the suture needle was docked into a 27-gauge needle and the needles were withdrawn, the suture was retrieved through the limbal incision and cut in half.The free end of the sutures was tied to the distal end of the external haptic of the IOL with 2-1-1-1-1 surgeon’s knots using toothless forceps with appropriate tension, and the knots were then trimmed.Most of the IOLs had two open-loop haptics, and the suture was tied approximately 1 mm from the distal end of the IOL haptics, regardless of whether the haptics had an end knob.If the IOLs had closed-loop haptics with sufficient total IOL length, the suture was tied to the opposite loop ends of the haptics.
The external haptic was introduced into the posterior chamber using toothless forceps.The other IOL haptic was externalized through the limbal incision and tied to the other free end with the 10-0 polypropylene suture using a similar procedure.After the total IOL was introduced into the posterior chamber and tension was adjusted as necessary to center the IOL, the needle of each arm of the 10-0 polypropylene suture was passed through the scleral bed underneath the flap to form a loop.Each suture was tied with appropriate tension to the loop using 2-1-1-1-1 surgeon’s knots and then trimmed.The scleral flaps and limbal incision were sutured with 10-0 nylon.After removal of the trocars and infusion cannula, the conjunctival wounds were closed with 7-0 Vicryl sutures.In addition,subconjunctival antibiotics and corticosteroids administered via injection.
Postoperative ophthalmologic evaluations including detailed fundus examination for retinal breaks were performed during any follow-up.IOL-induced astigmatism was defined based on the difference between the postoperative total refractive astigmatism and preoperative keratometric astigmatism.To evaluate the surgical effects, the preoperative and 3-month postoperative BCVA (logarithm of the minimum angle of resolution; logMAR values) and astigmatism (diopters; D)were analyzed using the Wilcoxon signed-rank test.AP-value <0.05 was considered statistically significant.
RESULTS
A total of 20 consecutive cases were enrolled for analysis(Table 1), comprising 16 men and 4 women with a mean age of 58y (range, 28-77y).All patients underwent at least a 3-month follow-up, and the mean final follow-up period was 9.8±5.3mo.Twelve eyes (60%) had dislocated PCIOLs in the vitreous cavity, and 8 (40%) had subluxated IOLs.Most IOLs (19/20; 95%) had 2 open-loops haptics and only one had 4 closed-loops haptics.The eye with subluxated closed-loop IOL had elevated IOP pre-operatively, and the IOP stabilized with reduced anti-glaucoma medications postoperatively.The visual acuity improved from a mean of 0.35 (0.46±0.32 logMAR) preoperatively to 0.61(0.21±0.18 logMAR) at the 3-month follow-up (P=0.002).The mean amount of keratometric astigmatism was -1.24±0.80 D preoperatively and the total refractive astigmatism was-1.42±0.97 D 3-month postoperatively.There was no statistically significant difference between preoperative and postoperative astigmatism (P=0.156).The mean IOL-induced astigmatism was -0.23±0.53 D.The mean spherical equivalent(SE) at the 3-month follow-up was -0.1±0.94 D.Seventeen eyes (85%) had postoperative refraction between -1.0 to +1.0 D SE.The patients’ baseline characteristics and postoperative data are shown in Table 2.In all cases, slit-lamp examination revealed the sutured IOL placed centrally with absence of clinically obvious tilt.Postoperative complications, such as hypotony, choroidal detachment, suture breakage, suture granuloma formation,endophthalmitis, IOL dislocation, retinal detachment,suprachoroidal hemorrhage, persistent postoperative inflammation, or uveitis-glaucoma-hyphema syndrome, were not noted during the period of follow-up.
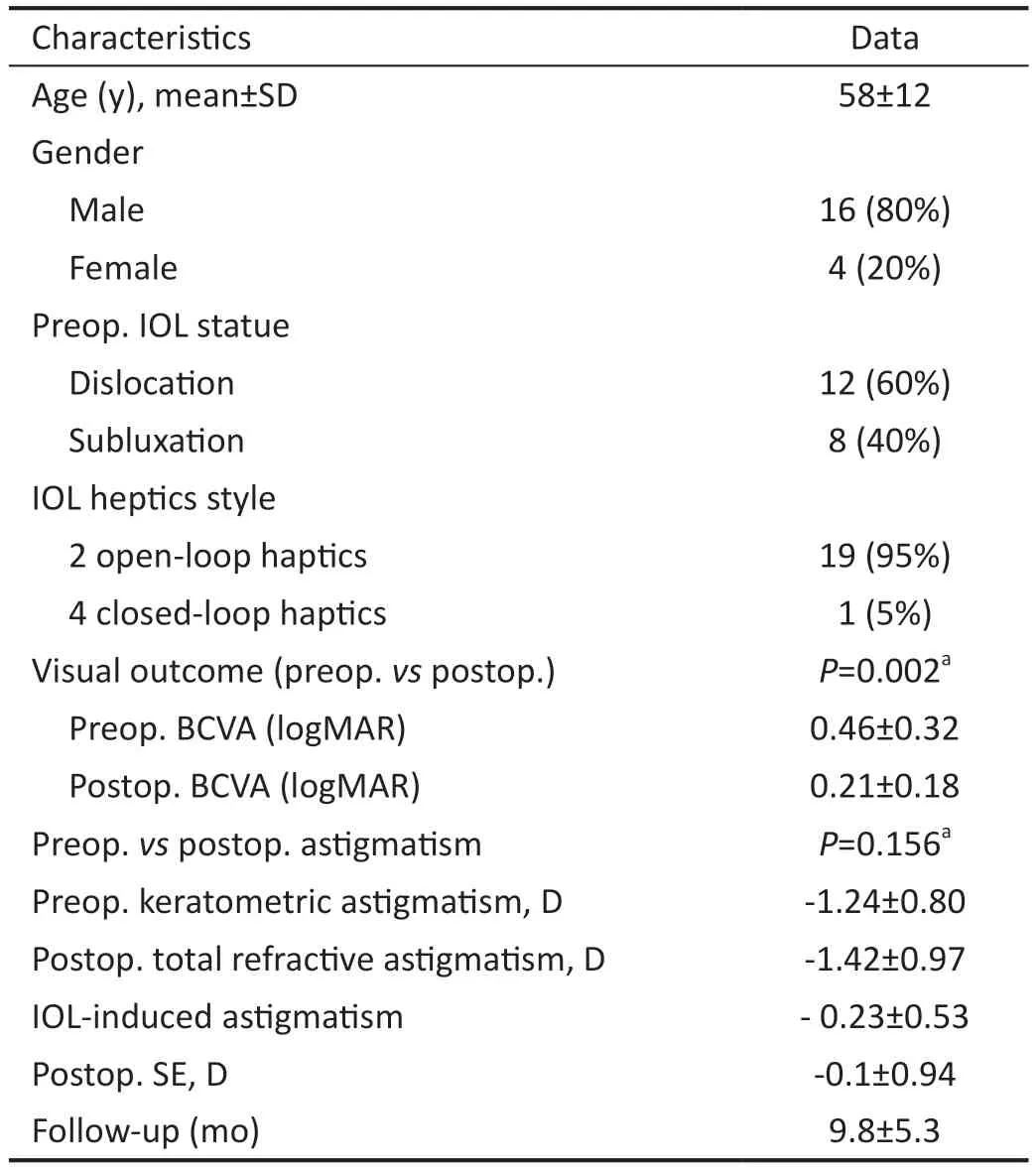
Table 2 Baseline characteristics and postoperative data of 20 eyes
DISCUSSION
A review of the literature conducted by the American Academy of Ophthalmology supports the effective use of variable techniques in the correction of aphakic eyes without adequate capsular support including sclera-sutured PCIOLs, openloop ACIOLs and iris-sutured PCIOLs, allowing for choices based on surgeon’s preferences and clinical factors[1].Although open-loop haptic ACIOLs are considered safe and effective,they are associated with complications, including risks of corneal endothelial damage, chronic iritis, and postoperative astigmatism induced because of the requirement for a large incision and other potential complications during operation[3].Potential complications associated to iris-fixated IOLs include peripheral anterior synechia formation, pigment dispersion,pupillary distortion, and chronic iritis[2].Scleral fixation of PCIOLs prevents lots of these complications owing to the absence of direct contact to the iris and the distance far away from the endothelium of cornea[9].In addition, this procedure may provide more optical satisfaction due to the IOLs are closer to the nodal point inside the eye.
Acrylic one-piece PCIOLs are some of the most popular implanted lenses.Trauma, pseudoexfoliation, or zonular dehiscence may dislocate any style of IOL.Sutureless scleral fixation of IOLs with various modified techniques has been reported[3-4].However, the techniques cannot be applied to acrylic one-piece PCIOLs including externalization and intrascleral embedding of the haptics[10-11].In addition, the technical challenges of sutureless IOL fixation remains, and exchanging the existing IOL for another requires a larger incision that risks corneal endothelial cell loss and increases postoperative astigmatism[12].In our study, the benefit of IOL rescue by sutured scleral fixation of existing IOLs provided the benefit of retaining the same IOLs and required minimal intraocular IOL manipulation; however, the infusion cannula setting is important to maintain ocular pressure during IOL haptic externalization and tying.
For sutured scleral-fixated IOLs, the IOLs should be easily fixated by the suture material.In general, surgeons use IOLs with haptic eyelets, which facilitate the fixation and stable positioning of IOLs[10,13].The tacky and soft nature of acrylic one-piece PCIOLs, square edges, and knob at the haptic tip prevent slippage of the sutures from the IOL haptics[5], even in IOLs without haptic knobs.The square and thicker edges of the haptic ends can provide sufficient contact area for IOL stability even using the one-point fixation technique.In our cases, the IOLs remained well-centered and stable with favorable refractive outcomes postoperatively.The mean postoperative refractive status was -0.1±0.94 D, and 17 (85%)had postoperative refraction between -1.0 and +1.0 D.Most patients had good postoperative refraction results.After the surgery, the IOL location in most of our cases may be similar to the intended in-the-bag fixation of IOLs.In fact, cases 10 and 12 included refractive data before IOL subluxation or dislocation, and the postoperative refraction change were+0.38 and +0.76 D, respectively.Three eyes had postoperative refraction beyond -1.0 to +1.0 D.This may have been due to the target refraction choice of existing IOLs or the slight surgery-induced IOL shifting.Most IOLs diameters between the two open-loop haptic tips (12.5 mm at least) in the market are sufficient for scleral fixation because of the mean diameter(11 mm) of the ciliary sulcus in average length eyes[14].Onepiece acrylic IOLs with closed-loop haptics and sufficient total diameter may be acceptable for sutured scleral fixation of IOLs[11].The suture tension on the sclera and IOLs should be appropriate and not too tight.Tight sutures provide more cutting force that may result in tearing of the haptics of acrylic IOLs[15].Many patients in our consecutive case series are male(16/20; 80%).The reason was out of our understanding and the gender ratio may barely affect the postoperative outcomes.
The positions of existing subluxated/dislocated IOLs or medium opacity may interfere with the predicted refraction for IOL exchange.In addition, the refractive diopters for existing IOLs may be accurate after previous calculations.Therefore, scleral fixation of existing IOLs is reasonable.In our cases, the sutured scleral fixation of existing IOLs resulted in favorable refractive outcomes comparable to those reported previously[16-17].In the current study, the mean IOL-induced astigmatism (-0.23±0.53 D) was less than that reported previously with scleral fixation of the IOL technique[6,10,18].The IOLs tilting after scleral fixation of IOLs may cause postoperative IOL-induced astigmatism as well as iris chafing.In our cases, slit-lamp examination revealed the sutured IOL placed centrally with absence of clinically obvious tilt.Nevertheless, the real postoperative IOL-induced astigmatism is difficult to estimate.In consideration to the postoperative status, we also calculated the postoperative IOLinduced astigmatism (difference between the postoperative total refractive astigmatism and postoperative keratometric astigmatism).The absolute value of postoperative IOL-induced astigmatism in our study was 0.39±0.14 D.Nineteen eyes(95%) in our case series had IOL-induced astigmatism of less than 1 D, which was less than that in one previous report of a mean 1 D increase in sutured PCIOLs and ACIOLs[19].This may have been due to the minimal surgical manipulation and symmetric scleral passage of the 10-0 polypropylene.
Sutured scleral fixation involves suture passage through uveal tissue, which may lead to potential risks, such as vitreous hemorrhage, retinal breakage, and retinal detachment[1,20].There were no permanent, visually significant postoperative complications and no IOL instability, dislocation, significant tilting, or pupillary capture of the IOL in our study.Besides, no suture-related complications, including erosion or breakage,were noted during the follow-up period in our series.
Late subluxation or dislocation of sutured scleral fixation of IOLs has been documented[21-24], especially occurring in young patients[21-22,24].This may be related to suture erosion,scleral tissue cutting by sutures, suture cutting by IOL haptics,IOL haptics cutting by sutures, suture damage by surgical manipulation, and degradation of the suture material itself.Suture erosion continues to be a troublesome complication of sutured scleral fixation of IOLs but no cases were observed because of the scleral flaps used in this series.Sclera tissue cutting by sutures or IOL haptic cutting by sutures may be prevented by appropriate and not too tight tension while suture tying.For acrylic one-piece IOLs, suture breakage may not be related to suture cutting by haptics because of the soft nature of the IOLs.In order to prevent suture damage by surgical manipulation, toothless forceps should be used in any procedure related to sutures of 10-0 polypropylene.All refinements of the surgical technique were performed in an attempt to prevent late IOL subluxation or dislocation.A clinicopathological study suggested that the surface properties of the positioning holes of IOLs lead to cutting of sutures,and subsequent subluxation of IOLs[23].In addition, suture breakage typically occurs after 10y postoperatively and in young patients[21-22,24].Nevertheless, suture degradation of 10-0 polypropylene cannot be neglected.Therefore, long-term follow-up and larger- diameter sutures or other suture materials instead of 10-0 polypropylene may be used to prevent this complication.
In our case series, techniques of sutured scleral fixation for existing subluxated or dislocated acrylic one-piece IOLs resulted in favorable visual and refractive outcomes.No major complications were noted during the follow-up period.However, a longer follow-up of more cases is required to evaluate the outcomes and complications in the future.
ACKNOWLEDGEMENTS
Conflicts of Interest: Huang WY,None;Chen YJ,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Algorithm of automatic identification of diabetic retinopathy foci based on ultra-widefield scanning laser ophthalmoscopy
- CD3ε of a pan T cell marker involved in mouse Aspergillus fumigatus keratitis
- Neuroprotective effects of acteoside in a glaucoma mouse model by targeting Serta domain-containing protein 4
- Neuroprotective and anti-inflammatory effects of eicosane on glutamate and NMDA-induced retinal ganglion cell injury
- Bone morphogenetic protein-6 suppresses TGF-β2-induced epithelial-mesenchymal transition in retinal pigment epithelium
- Dry eye rate and its relationship with disease stage in patients with primary hypertension: a cross-sectional study in Vietnam
