Maternal and neonatal blood vitamin D status and neurodevelopment at 24 months of age: a prospective birth cohort study
Yue Zhang · Chun-Yan Zhou · Xi-Rui Wang · Xian-Ting Jiao · Jun Zhang · Ying Tian · Luan-Luan Li · Chen Chen Xiao-Dan Yu,
Abstract Background This study aimed to explore the relationship of 25-hydroxyvitamin D [25(OH)D] in three trimesters and at birth with neurodevelopment at 24 months of age.Methods From 2013 to 2016,pregnant women from the Shanghai Birth Cohort in China were recruited for the study.Altogether,649 mother-infant pairs were included.Serum 25(OH)D was measured with mass spectrometry in three trimesters,and cord blood was divided into deficiency (<20 and <12 ng/mL,respectively),insufficiency (20–30 and 12–20 ng/mL,respectively),and sufficiency (≥ 30 and ≥ 20 ng/mL,respectively).Bayley-III scale was used to assess cognitive,language,motor,social-emotional,and adaptive behavior development at 24 months of age.The Bayley-III scores were grouped into quartiles,and scores within the lowest quartile were defined as suboptimal development.Results After adjusting for confounding factors,cord blood 25(OH)D in the sufficient group was positively correlated with cognitive [β =11.43,95% confidence interval (CI)=5.65–17.22],language (β =6.01,95% CI=1.67–10.3),and motor scores(β =6.43,95% CI=1.73–11.1);cord blood 25(OH)D in the insufficient group was also positively correlated with cognitive scores (β =9.42,95% CI=3.74–15.11).Additionally,sufficient vitamin D status in the four periods and persistent 25(OH)D ≥ 30 ng/mL throughout pregnancy were associated with a lower risk of suboptimal cognitive development in adjusted models,although the effects were attenuated after applying the false discovery rate adjustment.Conclusions Cord blood 25(OH)D ≥ 12 ng/mL has a significant positive association with cognitive,language,and motor development at 24 months of age.Sufficient vitamin D status in pregnancy might be a protective factor for suboptimal neurocognition development at 24 months of age.
Keywords 25-hydroxyvitamin D · Children’s neurodevelopment · Cord blood · Maternal vitamin D status
Introduction
The critical periods of vulnerability for neural development extend from the embryonic period through 2 years of age[1].Vitamin D,as a fat-soluble steroid hormone,plays an important role in brain development and function [2].Currently,vitamin D deficiency is a major public health problem worldwide,and more than half of pregnant women and newborns in nearly all regions have been reported to have a vitamin D deficiency [3].Concerns about the consequences of vitamin D deficiency during pregnancy on offspring brain development are of great significance.
At present,diverse studies have investigated the association between offspring neurodevelopment and vitamin D status in pregnancy,including in the first trimester (indicated as T1) [4–7],the second trimester (indicated as T2)[8–13],the third trimester (indicated as T3) [14–18],and in cord blood (indicated as CB) [6,10,11,19–21].Due to differences in the timing of blood collection,offspring age at the assessment of neurodevelopmental outcome,and type of neurodevelopmental outcome assessed,the results from these observational studies are mixed and inconsistent [4,16].Recently,some researchers collected all these relevant studies and conducted a systematic review/meta-analysis and found that low maternal 25-hydroxyvitamin D [25(OH)D]level in pregnancy is associated with adverse language and motor development in young children >1 year to 5 years of age [22],and a positive correlation between maternal vitamin D status and offspring’s cognitive and language performance [23,24].Overall,high maternal vitamin D status during pregnancy tends to have a neuroprotective effect on several domains of offspring neurodevelopment,but more well-designed studies are needed to confirm this hypothesis.
To date,none of the studies have investigated the association of vitamin D status during multiple stages of pregnancy with offspring neurodevelopment.Taking advantage of the Shanghai Birth Cohort (SBC),we recruited pregnant women and collected blood in three trimesters and CB for serum 25(OH)D measurement to investigate the effect of vitamin D status in pregnancy on offspring neurodevelopment at 24 months of age.
Methods
Participants and study design
The participants in the current study were from SBC,which was a prospective birth cohort to investigate the association of early life exposure to environmental pollutants with reproductive failure,adverse pregnancy outcomes,physical and mental developmental disorders in children,etc.[25].In this cohort,women in early pregnancy or planning to become pregnant were recruited from six hospitals in Shanghai,China,from 2013 to 2016,and the details,including inclusion criteria,were presented previously [25].Then pregnant women included in the study visited hospitals at T1,T2,T3,and at delivery.At each visit,trained staffcollected maternal peripheral blood (CB at delivery) for serum 25(OH)D measurement.After delivery,eligible infants were followed up to 24 months old for neurodevelopment assessment.Eventually,1086 pregnant women at T1,983 at T2,960 at T3,and 946 at delivery were included,and 649 children at 24 months of age fulfilled the neurodevelopment assessment.The details are displayed in Fig. 1.
The study was approved by the Medical Ethics Committee of Shanghai Xinhua Hospital affiliated with Shanghai Jiao Tong University School of Medicine,and written informed consent was obtained from all participants.
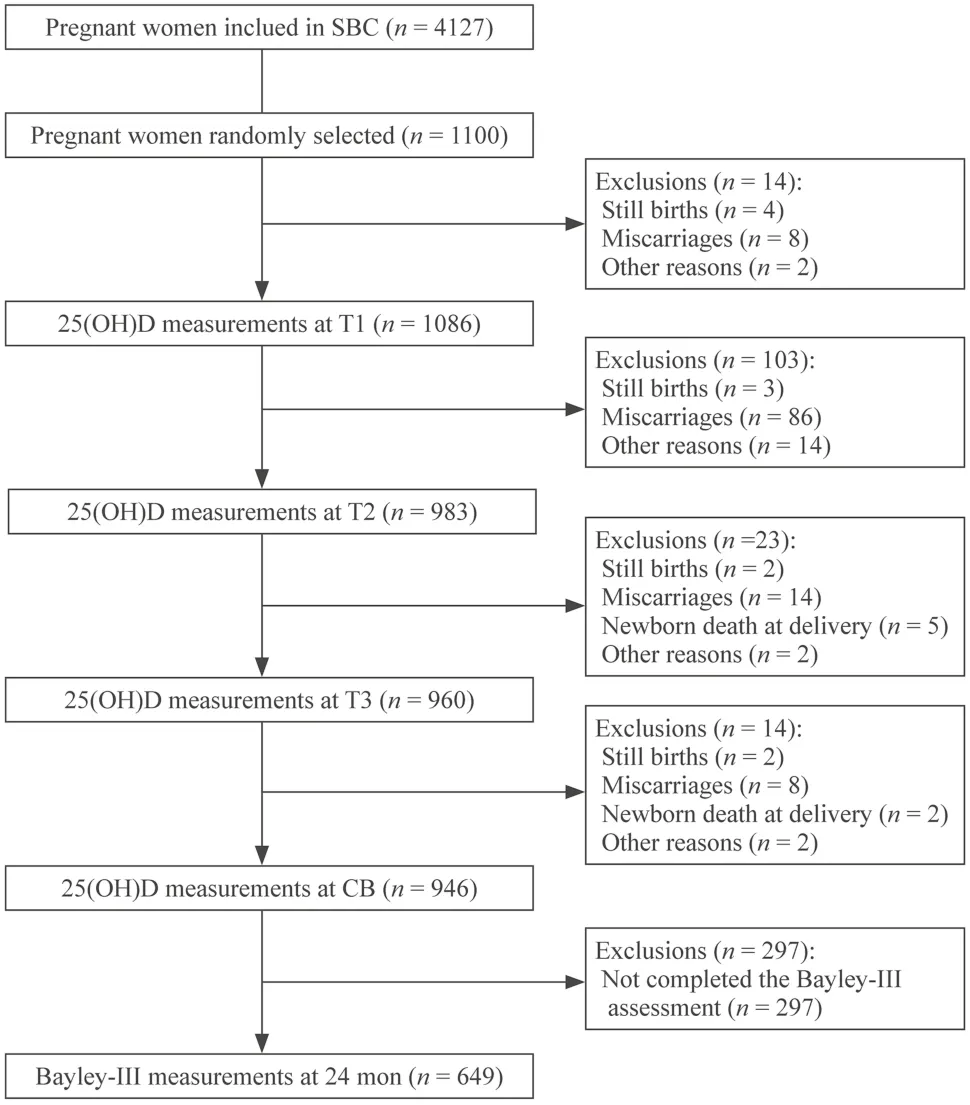
Fig.1 Flow chart of the participants included in the study. SBC Shanghai Birth Cohort,25(OH)D 25-hydroxyvitamin D,T1 first trimester,T2 second trimester,T3 third trimester,CB cord blood
25-hydroxyvitamin D measurement
Blood collected from pregnant women and neonates was centrifuged to obtain serum,which was frozen at − 20 °C until further use.Serum 25(OH)D concentrations were measured using liquid chromatography–tandem mass spectrometry as previously described [26].All samples were analyzed in duplicate to test 25(OH)D2and 25(OH)D3.The sum of the 25(OH)D2and 25(OH)D3levels was confirmed as the total 25(OH)D concentration.
Vitamin D status in pregnant women was determined according to the recommendations of the Institution of Medicine (IOM) [27] and Endocrine Society [28],which defined 25(OH)D levels ≥ 30 ng/mL,20–30 ng/mL and <20 ng/mL as sufficiency,insufficiency,and deficiency,respectively.Vitamin D status in newborns was confirmed based on our previous study [29] and recommendations of IOM[27] in which 25(OH)D levels ≥ 20 ng/mL,12–20 ng/mL,and <12 ng/mL were considered sufficient,insufficient,and deficient,respectively.
Neurodevelopmental assessment
Children’s neurodevelopment at 24 months of age was assessed with the Bayley-III scale,which consists of five independent subscales (cognition,language,motor,social–emotional,and adaptive behavior subscales) [30].After the assessment,the total raw scores of each subscale obtained from individual children were transferred to composite scores that are scaled to a metric with a mean of 100 and a standard deviation (SD) of 15.Generally,scale scores more than one SD below the mean (<85) were considered delayed [31].In our study,only 5% of children were in the delayed group,which may reduce the reliability of the data analysis.Therefore,we divided the Bayley-III scores into quartiles and defined suboptimal development as scores in the lowest quartile for all subscales [15].
Statistical analysis
Continuous variables and categorical variables are expressed as the mean ± SD and percentage,respectively.Univariate analysis was applied to examine the associations of Bayley-III scores with demographic characteristics,including 25(OH)D levels,in each period.Generalized estimating equations were used to study the correlation between the vitamin D level involving the three measures in pregnancy (T1,T2,and T3) and Bayley-III scores across the five subscales,and multiple linear regression was used to determine the associations between vitamin D status in each period and Bayley-III scores.With multiple linear regression,taking 30 ng/mL in maternal blood during pregnancy and 20 ng/mL in CB as the cutoffpoint for 25(OH)D level,the relationship between vitamin D status in each period and suboptimal neurodevelopment was analyzed.Moreover,a multivariable regression model was also applied to examine the persistent effect of maternal vitamin D status throughout pregnancy,i.e.,25(OH)D level <30 ng/mL in all three trimesters,25(OH)D level <30 ng/mL in T3 but 25(OH)D level ≥ 30 ng/mL in either T1 or T2,25(OH)D level ≥ 30 ng/mL in all three trimesters,and 25(OH)D level ≥ 30 ng/mL in T3 but 25(OH)D level <30 ng/mL in either T1 or T2,on neurodevelopment.Based on previous studies [6,10,11,19–21] and the results of univariate analysis,the potential confounders we considered were maternal age,maternal and paternal sociodemographic characteristics (maternal and paternal education level,annual household income),pre-pregnancy body mass index,and birth outcomes (mode of delivery,birth weight,infant’s gender).
A two-sidedPvalue <0.05 was considered statistically significant.In consideration of the multiple testing,we corrected thePvalues using the BenjaminiHochberg procedure to control the false discovery rate (FDR) [32–35].FDR-adjustedPvalues <0.05 and <0.1 are marked with a superscript asterisk and a superscript pound in tables,respectively.All statistical analyses were performed using Empower Stats ( www.empow ersta ts.com,X&Y solutions,Inc.Boston MA) and R software version 3.6.1 (http://www.r-proje ct.org).
Results
Participant characterization
The general characteristics of the participants and birth outcomes are shown in Table 1.The mean 25(OH)D concentrations in T1,T2,T3,and CB were 25.65 ± 10.02 ng/mL,31.64 ± 11.36 ng/mL,35.63 ± 13.52 ng/mL,and 19.84 ± 9.01 ng/mL,respectively.The vitamin D deficiency at the four periods [25(OH)D level <20 ng/mL in three trimesters,25(OH)D level <12 ng/mL in CB] was not uncommon,with occurrences of 32.70%,16.81%,12.45%,and 19.38%,respectively.Likewise,the frequency of pregnant women with 25(OH)D levels <30 ng/mL in T1,T2,and T3 and newborns with 25(OH)D levels <20 ng/mL in CB was relatively high(65.54%,46.20%,35.41%,and 58.42%,respectively).For the maternal characteristics,the mean age at birth was 28.73 ± 3.41 years;92.46% of them had a college education level or above;87.66% had a household income of 100,000 RMB/year or above.Similarly,fathers with a college education level or above accounted for the largest percentage (93.17%).Finally,approximately 40% of children were delivered by cesarean section,and more than 96% were born full term.
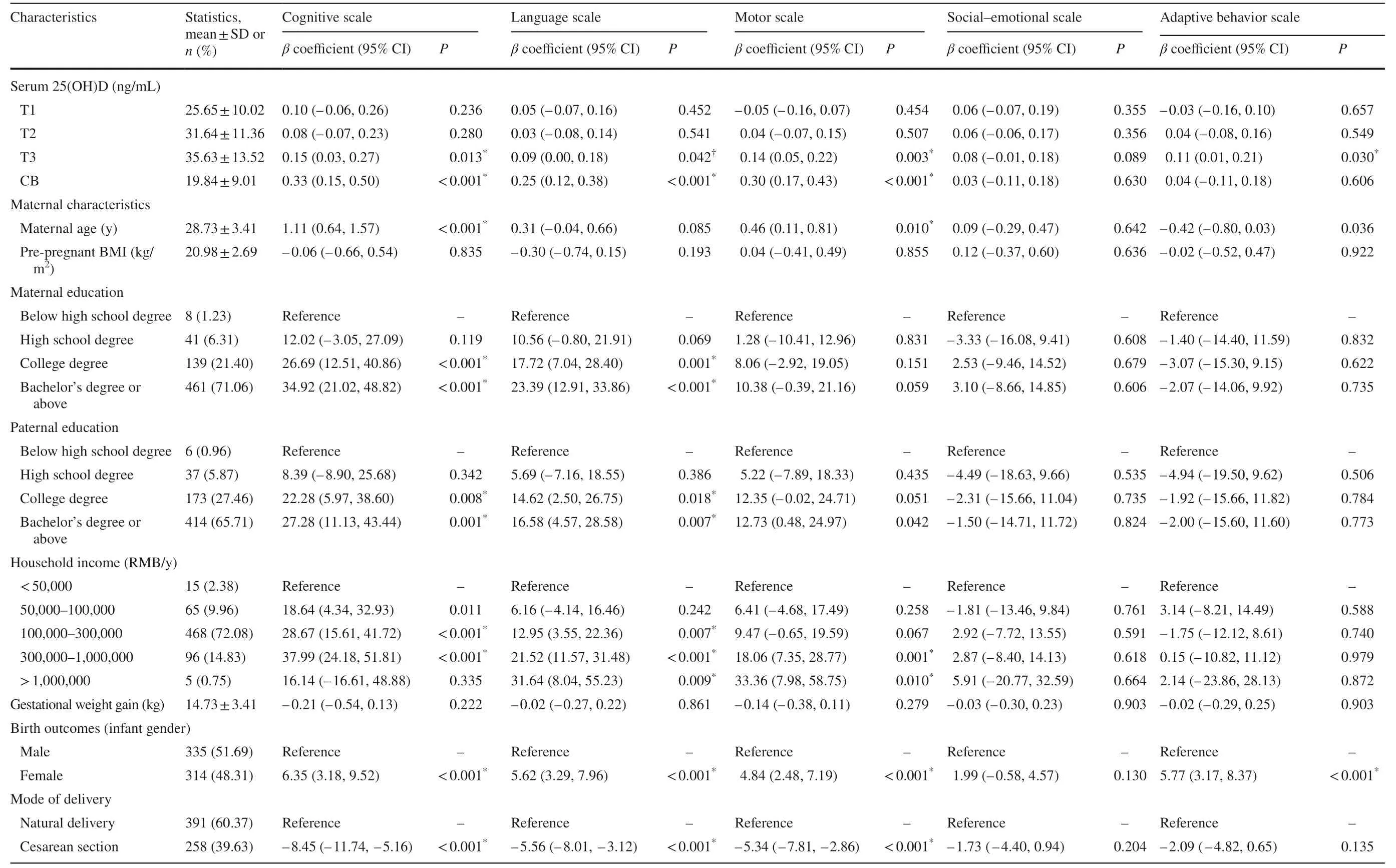
Table 1 Associations of the characteristics of mother–infant pairs with neurodevelopment at 24-month-old (n =649)
Factors related to neurodevelopment
The median Bayley-III scores across the five subscales at 24 months of age were as follows: cognition:115 [interquartile range (IQR)=100–145],language:98.5 (IQR=88–110),motor: 107 (IQR=100–118),social–emotional: 105 (IQR=95–115),adaptive behavior: 105 (IQR=93–118).Then we analyzed the associations between the five subscale scores and all variables,including 25(OH)D concentrations in each period(Table 1),and found that 25(OH)D levels in T3 and CB,maternal age at birth,maternal education,paternal education,household income,infant sex,model of delivery,and gestational week were significantly related to neurodevelopment (P<0.05).
Specifically,cognitive and language development were positively associated with 25(OH)D in CB,higher household income (100,000–1,000,000 RMB/year),high maternal education level (college degree or above),high paternal education level (college degree or above),and female gender but negatively related to cesarean section.In addition,cognitive scores were also positively related to 25(OH)D at T3,maternal age and household income within 50,000–100,000 RMB/year,and language scores were positively related to the highest household income(>1,000,000 RMB/year).Motor function was another domain affected by many factors,including 25(OH)D level in T3 and CB,maternal age,highest paternal education level (bachelor’s degree or above),higher household income (>300,000 RMB/year),female gender,and cesarean section.Among these factors,only cesarean section showed an inverse association with motor development.Social–emotional status had no relationship with any factors,and adaptive behavior was negatively correlated with 25(OH)D levels at T3,maternal age,and female sex.
Vitamin D levels and Bayley-III scale scores
After adjustment for potential confounders,including baby gender,birth weight,maternal age,pre-pregnancy maternal body mass index,socioeconomic position,maternal and parental education level,and mode of delivery,the relationship between 25(OH)D levels in the three trimesters in pregnancy (T1,T2,and T3) and neurodevelopment was analyzed using generalized estimating equations,and no association was observed (Table 2).In addition,the association of 25(OH)D level in each period with neurodevelopment was also analyzed using multiple linear regression (Supplementary Table 1),and only CB 25(OH)D had a significant positive association with Bayley-III cognitive [β=0.30,95% confidence interval(CI)=0.07–0.52,P=0.009],language (β=0.28,95%CI=0.11–0.44,P=0.001),and motor subscale scores(β=0.30,95% CI=0.13–0.48,P=0.001).
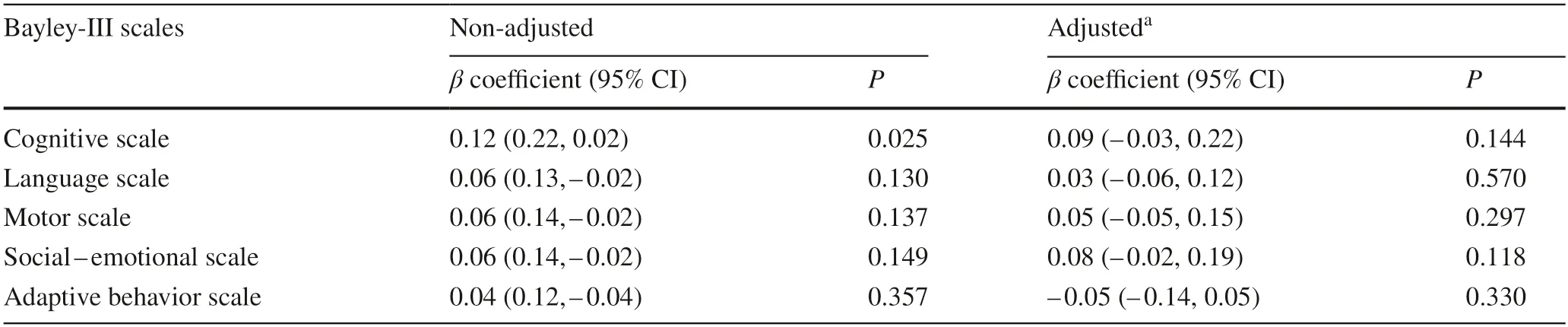
Table 2 Generalized estimating equation analysis of the association between vitamin D status during pregnancy and Bayley-III scales scores(n =649)
Vitamin D status and Bayley-III scale scores
We categorized 25(OH)D levels at the four periods into three statuses,i.e.,vitamin D sufficiency,insufficiency,and deficiency,and analyzed the association of the vitamin D statuses in each period with the scores of each domain subscale(Table 3 and Supplementary Table 2).
Taking vitamin D deficiency as a reference,after adjustment for potential confounders,only children with vitamin D insufficiency and sufficiency at birth had significantly increased cognitive scale scores (β=9.42,95% CI=3.774–15.11,P=0.001,andβ=11.43,95%CI=5.65–17.22,P<0.001,respectively),and children with vitamin D sufficiency at birth had significantly increased language (β=6.01,95% CI=1.67–10.35,P=0.007) and motor scale scores (β=6.43,95% CI=1.14–10.65,P=0.008).
Vitamin D status and suboptimal neurodevelopment
Using the value of 30 ng/mL in the three trimesters and 20 ng/mL in CB as the cutoffpoint for 25(OH)D level,we further analyzed the relationship between vitamin D status in each period and suboptimal neurodevelopment based on the multivariable regression model.In the adjusted analysis,in any of the three trimesters,a 25(OH)D level ≥ 30 ng/mL significantly reduced the risk of suboptimal neurocognitive development at 24 months of age (P<0.05) [T1:odds ratio (OR)=0.53,95% CI=0.30–0.91;T2: OR=0.53,95% CI=0.31–0.91;T3: OR=0.56,95% CI=0.33–0.95](Table 4).After FDR correction of thePvalue,a 25(OH)D level ≥ 30 ng/mL in the three periods showed no substantial decrease in the risk of suboptimal neurocognitive development.No relationship was found between vitamin D status
The persistent effect of maternal vitamin D status through pregnancy on Bayley-III scale scores
We also determined the persistent effect of maternal vitamin D status in three trimesters,i.e.,25(OH)D level <30 ng/mL in all three trimesters,25(OH)D level <30 ng/mL in T3 but 25(OH)D level ≥ 30 ng/mL in either T1 or T2,25(OH)D level ≥ 30 ng/mL in T3 but 25(OH)D level <30 ng/mL in either T1 or T2,and 25(OH)D level ≥ 30 ng/mL in all three trimesters on suboptimal neurodevelopment (Table 5).As shown in Fig. 2,children born to mothers with 25(OH)D levels ≥ 30 ng/mL in all three trimesters had significantly higher scores on the cognitive subscale than children born to mothers with 25(OH)D levels <30 ng/mL in all three trimesters.Likewise,children of mothers with 25(OH)D levels ≥ 30 ng/mL in all three trimesters had a significantly reduced risk of suboptimal cognitive development compared to children of mothers with 25(OH)D levels <30 ng/mL in all three trimesters (adjusted OR=0.39,95% CI=0.18–0.83,P=0.016) (Table 5 and Supplementary Table 4).The significance was minimized after thePvalue was adjusted by FDR.A reduced risk for suboptimal neurodevelopment of the other four domains in children of mothers with 25(OH)D levels ≥ 30 ng/mL in all three trimesters was not observed.
Discussion
This is the first prospective cohort study to investigate the association between vitamin D status in four periods and neurodevelopment at 24 months of age.Our findings reveal that CB 25(OH)D concentration has a significant positive association with Bayley-III cognitive,language,and motor scores,and vitamin D sufficiency throughout pregnancy might be a protective factor for neurocognition development at 24 months of age.in any of the four periods and suboptimal development for the other four domains (Table 4 and Supplementary Table 3).
It seems that the prevalence of 25(OH)D levels <20 ng/mL in pregnant women and newborns in Shanghai is much lower than that in other cities in China or other countries.In our study,32.7%,16.8%,and 12.5% of pregnant women had 25(OH)D levels <20 ng/mL in T1,T2,and T3,respectively,and 58.4% of newborns had 25(OH)D levels <20 ng/mL.In Wuxi city in eastern China,the frequencies of pregnant women in T1,T2,and T3 were 81.3%,77.4%,and 78.8%,respectively [36].The values in pregnant women and neonates from Liuzhou city in southern China were 79.18% and 83.27%,respectively [37].In one systematic review that focused on maternal and newborn vitamin D status globally [3],the prevalence of 25(OH)D <20 ng/mL in pregnant women from the Americas,Europe,Eastern Mediterranean,SouthEast Asia,and Western Pacific was 64%,57%,46%,87%,and 83%,respectively;among newborns,these values were as follows: Americas (30%),Europe (73%),Eastern Mediterranean (60%),SouthEast Asia (96%),and Western Pacific (54%).We speculated that the relatively low prevalence of 25(OH)D level <20 ng/mL in pregnant women and newborns in Shanghai may be attributed to vitamin D supplementation during pregnancy,a high proportion of mothers or fathers with college education level or above,family with household income 100,000 RMB/year or above,and relatively adequate time spent in outdoor activities for one week [29,38].
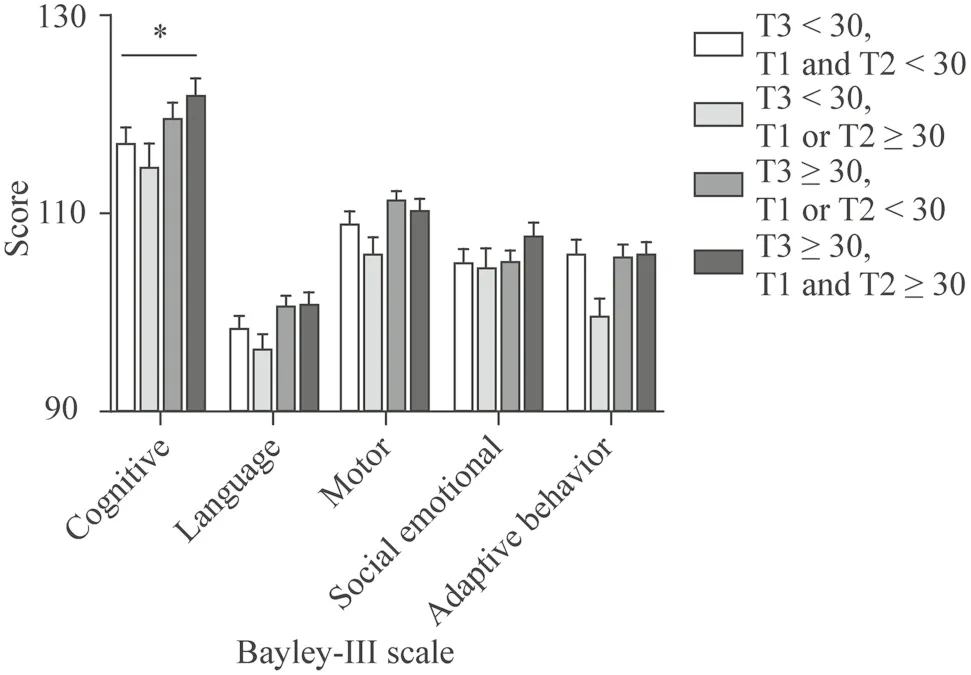
Fig.2 Persistent effect of maternal vitamin D status throughout pregnancy on neurodevelopment at 24 months of age. T1 first trimester,T2 second trimester,T3 third trimester. * Difference among four groups,P <0.05
Neurodevelopment is multifactorial.Our study is in line with previous studies [12,39–43] and shows that parental education,household income,and female sex had a strong positive association with neurodevelopment in early childhood (24 months old),mainly with cognitive,language,and motor development.High socioeconomic status,e.g.,parental high education level and high household income,generally suggests that children will have more intellectual resources,nutrition,high-quality health care,etc.,that are good for brain development [39,44].Gender differences in offspring neurodevelopment may result from the varied rate of mental and psychomotor development in boys and girls during early childhood [45].In addition,in our study,cesarean section was inversely associated with cognitive,language,and motor development at 24 months of age.To date,many studies have investigated the relationship between mode of delivery and neurodevelopment in early childhood [46–48] and implied that cesarean delivery might have an influence on offspring brain development,but the influence seems to gradually diminish or even disappear as children age [48].Since the specific delivery model,i.e.,elective cesarean delivery,emergency cesarean delivery,spontaneous vaginal delivery,and instrumental vaginal delivery,was not considered and only one time point(24 months old) was involved,our findings on the impact of delivery mode on offspring neurodevelopment need to be validated further.
The 25(OH)D level during pregnancy in our study is another key factor related to neurodevelopment.Among the four periods,25(OH)D ≥ 12 ng/mL at birth had a significant positive association with neurodevelopment at 24 months old,mainly with cognitive,language,and motor development,and the results were supported by previous studies.Supriadi et al.[49] and Juwita et al.[50] stated that CB 25(OH)D was significantly positively correlated with the problem-solving domain at 12 or 24 months.Keim et al.[11]observed a positive correlation between vitamin D levels in CB and neurocognitive development at age 7,but the effect estimates were very small.Gould et al.[21] reported that CB vitamin D levels had a weak positive association with language development in children aged 18 months and 4 years old.Overall,CB 25(OH)D levels affect neurodevelopment in early childhood,particularly in cognitive and language domains,although the effect found in some investigations was small.Additionally,consistent with many studies [11,21,50],our study also found no association between maternal and neonatal 25(OH)D levels and social–emotional and adaptive behavior development.Animal studies also supported these findings.Overeem et al.[51] used a rodent model of gestational developmental vitamin D deficiency and observed that mouse dams with vitamin D deficiency during gestation can impair offspring mouse cognitive development but have no effects on social behaviors.Since social skills are largely learned within the context of day-to-day interactions with caregivers during the early years of life,interactions after birth may have a stronger effect than vitamin D status during pregnancy [52,53].
Maternal 25(OH)D levels in the three trimesters had no significant association with neurodevelopment at 24 months of age in our study.Currently,the results regarding the association between maternal 25(OH)D levels in the three trimesters and neurodevelopment in early life remain mixed and inconclusive,which may have been attributed to the following differences in these studies.First,the varied cut-points for vitamin D deficiency were defined since a standard cutoffpoint for vitamin D deficiency has not been confirmed.In our study,CB 25(OH)D >12 ng/mL significantly increased the scores of the cognitive,language,and motor subscales.In another similar study carried out by our colleagues,no association was observed when the 25(OH)D level in CB <20 ng/mL was defined as vitamin D deficiency [19].Likewise,Hanieh et al.[14] stated that maternal 25(OH)D levels <15 ng/mL during late pregnancy were associated with reduced language developmental outcomes at 6 months.In our study,maternal 25(OH)D levels <20 ng/
mL during pregnancy had no significant relationship with neurodevelopment.The prevalence of pregnant women with 25(OH)D levels <20 ng/mL was not high in our study(Results section).If vitamin D deficiency is defined by a lower 25(OH)D level,the number of corresponding pregnant women would be insufficient for reliable analysis.Second,the critical period of brain development is the first 1000 days from conception to 2 years of age [1].Vitamin D deficiency in pregnancy may affect fetal brain development,whereas vitamin D levels in the offspring restored after birth may also rebuild brain development since most associations were found only in early childhood.In Morales et al.’s study [8],a 25(OH)D concentration >30 ng/mL in T1 was associated with improved Bayley-III cognitive and motor scores in infants at 14 months of age.In Gale et al.’s[16] study,exposure to maternal 25(OH)D levels >30 ng/mL in late pregnancy did not appear to influence neurocognitive development at 9 years,and Veena et al.[18] also confirmed the findings in children (age: 9–10 years) and adolescents(age: 13–14 years).Last,some studies reported that a small sample size or a low prevalence of vitamin D deficiency may also contribute to inconsistent results [22].In our study,the percentage of pregnant women with vitamin D deficiency[25(OH)D <20 ng/mL] in the three trimesters was 32.7%,16.81%,and 12.45%,respectively.As mentioned above,the optimal cutoffpoint for 25(OH)D level as vitamin D deficiency may be lower,so unreliable analysis due to the insufficient number cannot be excluded.
Although not all four periods of 25(OH)D levels were associated with neurodevelopment at 24 months of age in our study,we found that sufficient vitamin D status in four periods shows an effect on reducing the risk of suboptimal cognitive development at 24 months of age.Indeed,some studies focused on the critical time window for neurodevelopment related to vitamin D status.Voltas et al.[6] and Veena et al.[18] suggested that the early stage of gestation (T1 and T2) was more critical for neurodevelopment,particularly for cognitive and language development.In one review article,the early stage of gestation was identified as the critical period in the development of the fetal nervous system due to the beginning of neurogenesis and the myelination process [6,54].Interestingly,deficient vitamin D status in T1 [7] and T3 [6,15] was also reported to be correlated with worse motor performance.In O'Loan et al.’s [55] study using a rat model of vitamin D deficiency,they observed that maternal vitamin D deficiency in T3 could disrupt offspring’s brain function,whereas deficiency in T1 did not.Overall,it appears that vitamin D status throughout pregnancy is involved in neurodevelopment,but it is hard to conclude which period is more critical.In our study,a high 25(OH)D level in the late stage of pregnancy (at delivery) can improve neurodevelopmental outcomes (cognitive,language,and
motor domains),while sufficient vitamin D status from the early stage to late stage of pregnancy continuously influenced neurocognitive development,both indicating the critical role of a high 25(OH)D level in the late stage of pregnancy and the necessity of a high 25(OH)D level in the early stage for neurodevelopment.At present,our study is the first cohort-based report to measure the effect of 25(OH)D levels in multiple stages of pregnancy on offspring neurodevelopment.Additionally,the period after birth to 2 years of life is also critical for neurodevelopment[1],whereas related studies are extremely limited.Hence,the sensitive time window for neurodevelopment needs more studies to investigate.
To our knowledge,our study,with a prospective multicenter design that would help provide stronger evidence,is the first longitudinal study including 25(OH)D level data from four periods.Nevertheless,this study has some limitations.First,the follow-up rate was not high at 24 months of age.Second,sample selection bias cannot be excluded since this study was conducted in one city.Third,although multiple confounders were adjusted,we could not exclude the possibility of confounding from other factors,e.g.,smoking and alcohol consumption.Fourth,we also cannot exclude the potential effect of genetic variants on neurodevelopment,which have been reported to correlate with neurodevelopment [56],and the analysis cannot be performed because of the lack of available data.Finally,our study was conducted in this population only,and it is important to be cautious when extrapolating our findings to other populations.
In conclusion,our study provides evidence that CB 25(OH)D levels are significantly positively associated with cognitive,language,and motor development at 24 months of age,and sufficient vitamin D status in four periods or persistent sufficient vitamin D status throughout three trimesters will reduce the risk of suboptimal neurocognitive development.Currently,there are still many unsolved questions,e.g.,the optimal cutoff points for 25(OH)D level defined as deficient vitamin D status during pregnancy,the sensitive time window for neurodevelopment related to vitamin D status,and whether vitamin D levels in the offspring restored after birth could rebuild brain development.All these questions need to be solved urgently.
Supplementary InformationThe online version contains supplementary material available at https:// doi.org/ 10.1007/ s12519-022-00682-7.
AcknowledgementsWe are extremely grateful to all the families who took part in this study.And we would like to thank the doctors,midwives,and nurses involved in our study for patient management.
Author contributionsZY,ZCY,and WXR contributed equally to this work.YXD conceived of the research idea and designed the study,revised and supervised the manuscript.ZY performed 25(OH)D measurements,analyzed the data and performed the statistical analysis,and drafted the manuscript.ZCY performed 25(OH)D measurements and drafted the manuscript.WXR analyzed the data and performed the statistical analysis,and drafted the manuscript.JXT performed 25(OH)D measurements.ZJ and TY conceived of the research idea and designed the study.LLL and CC performed 25(OH)D measurements.All the authors read and approved the final manuscript.
FundingThis work was supported by the National Key Research and Development Program of China (No.2022YFC2705203),the National Natural Science Foundation of China (No.81773411),the Special Program for Women and Children Health (No.2020YJZX0212),Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant Support (No.20152220),the Cultivation Project of Clinical Research from SCMC (No.LY-SCMC2020-06),Shanghai Children’s Health Services Capacity Program (No.GDEK201708),the Key Program for Clinical Nutrition (No.2019ZB0103) from Shanghai Municipal Health Commission.The funding agencies played no role in the design,analyses,or interpretation of this study.
Data availabilityThe data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Ethical approvalThe study was approved by the Medical Ethics Committee of Shanghai XinHua Hospital affiliated to Shanghai Jiao Tong University School of Medicine (XHEC-C-3–001-3) and written informed consents were obtained from all participants.
Conflict of interestAll authors declare no conflict of interest.
 World Journal of Pediatrics2023年9期
World Journal of Pediatrics2023年9期
- World Journal of Pediatrics的其它文章
- Fecal microbiota transplantation in childhood: past,present,and future
- Pediatric endocrinopathies related to COVID-19: an update
- Mapping the quality of prenatal and postnatal care and demographic differences on child mortality in 26 low to middle-income countries
- Clinical epidemiology and disease burden of bronchiolitis in hospitalized children in China: a national cross-sectional study
- Serum levels of the novel adipokine isthmin-1 are associated with obesity in pubertal boys
- Effects of fentanyl and sucrose on pain in retinopathy examinations with pain scale,near-infrared spectroscopy,and ultrasonography:a randomized trial
