Fecal microbiota transplantation in childhood: past,present,and future
Xu Gu · Zhao-Hong Chen · Shu-Cheng Zhang
Abstract Background Fecal microbiota transplantation (FMT) has been well described in the treatment of pediatric diseases;however,the latest updates regarding its use in children are unclear and the concepts involved need to be revisited.Data sources We performed advanced searches in the MEDLINE,EMBASE,and Cochrane databases using the keywords“Fecal microbiota transplantation OR Fecal microbiota transfer” in the [Title/Abstract] to identify relevant articles published in English within the last five years.To identify additional studies,reference lists of review articles and included studies were manually searched.Retrieved manuscripts (case reports,reviews,and abstracts) were assessed by the authors.Results Among the articles,studies were based on the mechanism (n =28),sample preparation (n =9),delivery approaches(n =23),safety (n =26),and indications (n =67),including Clostridium difficile infection (CDI) and recurrent C. difficile infection (rCDI; n =21),non-alcoholic fatty liver disease (NAFLD; n =10),irritable bowel syndrome (IBS; n =5),inflammatory bowel disease (IBD; n =15),diabetes (n =5),functional constipation (FC; n =4),and autism spectrum disorder(ASD; n =7).Conclusions Concepts of FMT in pediatric diseases have been updated with respect to underlying mechanisms,methodology,indications,and safety.Evidence-based clinical trials for the use of FMT in pediatric diseases should be introduced to resolve the challenges of dosage,duration,initiation,and the end point of treatment.
Keywords Autism spectrum disorder · Children · Clostridium difficile infection · Fecal microbiota transplantation ·Functional constipation · Safety
Introduction
Fecal microbiota transplantation (FMT) is a method that transfers stool from a healthy donor to a recipient to restore the intestinal microbiota environment and achieve a therapeutic benefit.FMT was first recorded in the Jin Dynasty in ancient China.A Chinese physician,Hong Ge,elaborated the effect of stool by mouth on patients with food poisoning or severe diarrhea.In the “Compendium of Materia Medica,” written by Shi-Zhen Li in the Ming Dynasty,over 20 FMT methods were documented for treating gastrointestinal diseases such as food poisoning,diarrhea,fever,vomiting,constipation,and abdominal pain [1].FMT was also applied in veterinary medicine in Europe in the sixteenth century.Additional therapeutic use of human excretions was described in Europe in the eighteenth and nineteenth centuries and in World War II,during which gut bacteria were administered to German soldiers suffering from dysentery in the North African campaign [2].More scientifically,in 1958,Eismann successfully utilized fecal transplantation via enemas in four patients for the treatment of severe pseudomembranous colitis [3].Three of the four patients recovered and were discharged from the hospital after several days,while the fourth patient died from nonintestinal-associated diarrhea.Taken together,these results suggested the clinical value of FMT [3].
In early 2011,FMT was proposed to treat gastrointestinal diseases[4].Physicians called for the use of FMT by colonoscopy,gastroscopy,and gastroduodenal catheterization forClostridium difficileinfection (CDI) instead of surgery in an effort to reduce deaths.Since that time,the number of studies focusing on FMT has increased rapidly.In 2012,Khorouts et al.carried out the first study using standard cryopreserved bacteria [5].In 2013,Nood et al.reported that FMT was successful in the treatment of a recurrentC.difficileinfection (rCDI) in a randomized controlled trial at the University of Amsterdam [6].At the same time,the Food and Drug Administration (FDA) approved the use of FMT in humans [7].In the pediatric population,the first use of FMT can be traced to Massachusetts General Hospital in the United States in 2010.Russell et al.reported a two-yearold child with rCDI whose symptoms resolved completely 36 hours after FMT administration and no recurrences or adverse events (AEs) occurred during the six-month followup period [8].Although the enormous potential of FMT is apparent,FMT-related AEs have been identified in the published literature [9–13].Therefore,the acceptance,use,and safety of FMT are still under investigation.
Mechanism underlying fecal microbiota transplantation
The goal of FMT is to re-establish the intestinal flora by normalizing the amount and activity of immune and inflammatory responses,neurotransmitters and vasoactive substances,and energy metabolism [14].The diversity of the microbiota prevents the colonization and overgrowth of pathogens when homeostasis is achieved in the gastrointestinal tract.FMT can make the composition of the gut microbiota similar to that of the donor so that the proportion and diversity of beneficial bacteria is balanced [15].FMT can reduce intestinal permeability and maintain the integrity of the epithelial barrier by increasing the production of short-chain fatty acids,thereby reducing the severity of the disease [14,16,17].Moreover,gut microbiota can activate the humoral immune response and induce the synthesis of immunoglobulin A (IgA),immunoglobulin G (IgG),and immunoglobulin M (IgM) through the Toll-like receptor (TLR) pathway,thus protecting the intestinal mucosa [14].FMT inhibits the secretion of proinflammatory cytokines and promotes T helper 1 (Th1) cell differentiation,T cell activity,leukocyte adhesion,and immunestimulating factors [7].FMT also reduces intestinal pH and increases the adhesion of bacteria to H2O2,inhibiting the transport of pathogens [18].All these findings serve as the presumed mechanism underlying FMT effectiveness [14–18].
Indications
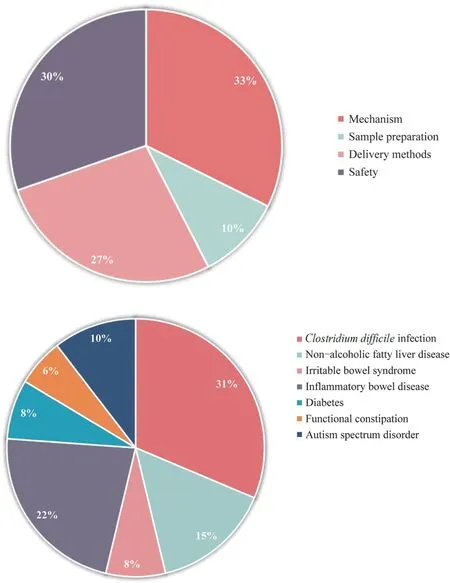
Fig.1 Literature related to fecal microbiota transplantation (FMT)includes indications,mechanism,donor exclusion,sample preparation,and delivery methods
Advanced searches in the MEDLINE,Embase,Cochrane Library,and Cochrane IBD Group Specialized Register databases with the terms “Fecal Microbiota Transplantation OR Fecal Microbiota Transfer” in the [Title/Abstract] field were performed.Based on the research strategy,a bibliometric analysis was performed on the use of FMT in children in the last five years,and 67 articles reported the indications of FMT in children (Fig. 1).The acquired literature includedClostridium difficileinfection (CDI) and recurrentClostridium difficileinfection (rCDI;n=21),non-alcoholic fatty liver disease (NAFLD;n=10),irritable bowel syndrome (IBS;n=5),inflammatory bowel disease (IBD;n=15),diabetes (n=5),functional constipation (FC;n=4),and autism spectrum disorder (ASD;n=7).The references,study design,interventions,and results of the indicated diseases for pediatric FMT were retrieved and are summarized in Table 1.
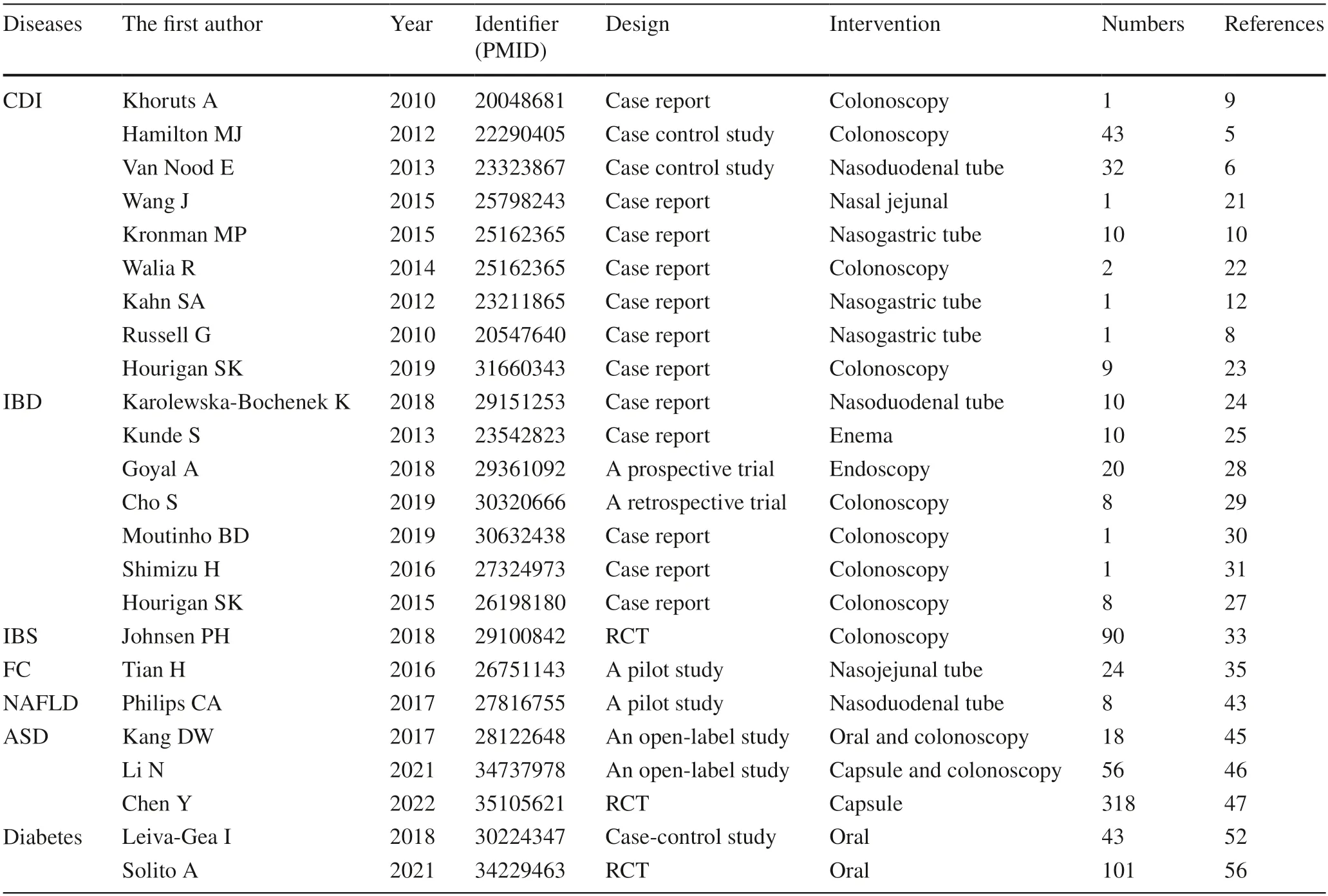
Table 1 Current potential indications for pediatric FMT
Established indications
Clostridium difficile infection
Clostridium difficileinfection (CDI) and recurrentClostridium difficileinfection (rCDI) are considered the most suitable indications for pediatric FMT [19].The incidence of rCDIs has been reported to be as high as 90%,some ofwhich are appropriate for traditional therapy [5,6,9,20].The youngest reported child receiving FMT for CDI was a 13-month-old infant [21];several other reports involved children over three years of age [10,12,22].These cases were successful,and FMT for CDI has been associated with improved growth in young children [22].Russell reported the first case of a two-year-old child with rCDI for whom the donor was transported through a nasogastric tube to the child’s small intestine in 2010 [8].The CDI symptoms resolved completely 36 hours after FMT administration,and there were no recurrences or adverse reactions during six months of follow-up [8].Suchitra selected nine pairs of donor receptors with an average age of 10 years in 2019 to examine the efficacy of FMT in pediatric CDIs [23].Three days after FMT treatment,CDI-related symptoms of all recipients were alleviated,and no recurrences occurred.During the follow-up period,one patient had long-termC.difficile-negative diarrhea and intermittent incontinence,which was mild and different in nature compared with CDI symptoms before FMT [23].Furthermore,a multicenter retrospective cohort study was also conducted on the largest sample size of CDI trials in children [35].Of the 335 children,271 (80.9%) were cured by the traditional therapeutic regimen.In the remaining 64 children with rCDIs,19(53.1%) were cured after FMT treatment,reaching an overall success rate of 88.6%.Inflammatory bowel disease
The efficacy and safety of FMT in pediatric IBD has been confirmed in several studies [24–27].Katarzyna assessed the effectiveness of a two-week FMT course in 10 children(10–17 years of age) with moderate-to-severe IBD by freshly prepared FMT via a nasoduodenal tube and found that a short,intensive course of FMT has a beneficial effect on ulcerative colitis (UC) and Crohn’s disease (CD) [24].Goyal et al.reported 21 patients with IBD refractory to medical therapy who underwent a single FMT by upper and lower endoscopy with a median age of 12 years;57% and 28% demonstrated clinical responses one and six months after FMT administration.Two patients with CDI were in full remission at six months [28].Similarly,in 2019,Cho reported a 75% rate response in eight patients with IBD three months after FMT[29];however,contrary results have also been reported.In a case report of a 17-year-old male with refractory UC,clinical improvement lasted for only one month before symptoms recurred.A second implementation of FMT also led to no improvements [30].In another case involving an 11-year-old girl,the first FMT led to exacerbation of UC symptoms,while repeated procedures allowed her to remain in remission with a minimal dose of steroids [31].There are two points that may contribute to the variation in FMT in childhood IBD.First,the pathogenesis of IBD in children may differ from that in adults.Second,most parents do not allow their children to be research subjects for safety reasons,thus resulting in poor compliance and a high dropout rate in the pediatric population.
Potential indications
Irritable bowel syndrome
In 2019,a systematic review and meta-analysis reported the efficacy of FMT in the IBS through a total of 33 randomized clinical trials (RCTs) involving 4321 patients [32].The authors pointed out that the clinical symptoms of IBS were alleviated after FMT treatment.Other meta-analyses and cohort studies have shown significant improvement in IBS patients after FMT treatment [33,34].FMT has enormous potential in adult IBS.Nevertheless,there is still uncertainty about FMT treatment in pediatric IBS because clinical trials for treating childhood IBS have not been conducted.
Functional constipation
Functional constipation has also been reported as a potential indication for FMT.In 2016,Tian conducted an open-label study of FMT in the treatment of slow-transit constipation(STC) [35].In this trial,24 STC patients (20–74 years of age) were enrolled.FMT was performed on three consecutive days through nasal-jejunal tubes,and the patients underwent follow-up for 12 weeks.Clinical improvement was shown in 50% (12/24) of those recruited,and full remission was found in 37.5% (9/24) with no AEs reported [35].Similar results regarding the use of FMT in childhood constipation have also been reported.In 2016,de Meij TG reported a significant increase in bacterial species in a study using conventional culture techniques in 28 constipated children compared with 14 healthy children [36].By comparing the fecal flora between eight constipated children and 14 healthy children,the authors observed an increase in the abundance of bifidobacteria in constipated subjects [36].Together,these results indicated that FMT has enormous potential for treating childhood constipation [37].
The king had no choice but to give the man the letter, and he strode off, making short work of the distance that lay between the palace and the Underworld
Fatty liver disease
Non-alcoholic fatty liver disease (NAFLD) severity is closely related to the dysregulation of intestinal bacteria and changes in metabolic function.Studies have shown differences in the composition of bacteria in the feces of NAFLD and healthy patients [38].Another study involving non-alcoholic steatohepatitis (NASH) in children mentioned that compared with the control group,the content of bacterial components in NASH children was different.A metaanalysis confirmed that at normal transaminase levels,the laboratory indices of the probiotic experimental treatment group improved significantly compared to the placebo group[39].Reducing the number of harmful microbiota can also increase the concentration of butyrate in the cecum and the expression of the intestinal tight junction protein (ZO-1).The increased butyrate and tight junction protein,ZO-1,is beneficial because butyrate is the energy source of colonic motility,and ZO-1 can repair the mucosal barrier of the colonic epithelium [40].A meta-analysis confirmed that probiotics reduced the number of harmful microbiota and increased the level of butyrate and ZO-1 [41].It has been reported that with the recovery of intestinal flora,the symptoms of portal hypertension and other hepatic symptoms significantly improved [42].Moreover,the implementation of FMT has not increased the incidence of AEs in any NASH/NAFLD patients [43].On the basis of existing clinical and experimental data,FMT has therapeutic potential in NASH/NAFLD [43].
Autism spectrum disorder
Gut flora and its metabolites play an important role in the pathophysiology of ASD [44–47].In 2017,Kang adopted a modified FMT regimen involving 18 participants with ASD(7–16 years of age) [45].An improvement was observed in 89% of the participants with respect to the symptoms of diarrhea,constipation,dyspepsia,and abdominal pain,but the autis
m symptoms were not significantly reduced [45].Subsequently,the author performed a two-year follow-up evaluation,and in 2019,the ASD symptoms of the participants were re-evaluated [45].Interestingly,a significant improvement in behavior symptoms was observed in all participants compared to the baseline measurements,suggesting the effectiveness of FMT in ASD [48].Nevertheless,the remission of ASD symptoms of the participants could not be completely attributed to FMT because the improvement of behavioral symptoms occurred two years later.The brainintestine axis may be a means of communication between the brain and intestinal flora.Several studies have shown how the gut flora may alter brain function [49–51].
Diabetes
To determine the differences in intestinal flora among children with metabolic diseases,Isabel Leiva-Gea published a study in 2018 comparing 15 diabetic and 13 healthy children [52].Leiva-Gea reported that the intestinal flora in children with type 1 diabetes differed in classification and function from healthy subjects,and there were fundamental differences in non-autoimmune diabetes models.In another study,Vrieze administered FMT to patients with metabolic syndrome,and insulin sensitivity improved significantly after FMT administration,suggesting the feasibility of FMT in metabolic diseases [53–55].Solito assessed the effects of probiotic supplementation on weight and metabolism in 101 obese and insulin-resistant young children in a cross-over,double-blind,randomized controlled trial [56].The study demonstrated that eight weeks of intervention was safe,well tolerated,and efficacious in improving insulin sensitivity and supporting weight loss.
Methodology
Donor screening
Preparation
Stool that is used for FMT can be fresh or frozen [19,65–70].Fresh stool should be disposed of within six hours of donation and stored at room temperature for further treatment.The feces are thoroughly stirred with standard sterile sodium chloride,and the filtrate is drawn into a syringe and injected into the gastrointestinal channel of the recipient.Another type of frozen feces is made by collecting feces from a group of pre-screened donors and storing frozen feces in the feces bank in equal aliquots.Final disposal is in storage at −80 °C.On the day of FMT,the fecal suspension is defrosted in a warm water bath (37°C),then dissolved in normal saline to obtain the expected volume of the suspension.The infusion is performed within six hours after defrosting [7].Notably,repeated defrosting and freezing should be avoided.Regardless of the methods used to obtain the fecal liquid,the principle of asepsis must be considered in the process of making fecal bacteria liquid for FMT,and the influence of air oxidation on fecal bacteria should be prevented.It is often not possible to determine the amount of fecal bacteria liquid that the patient needs.Compared with the relatively large amount of the infusion,the risk of failure when the infusion amount is <50 g is more than fourfold higher [20].The determination of the amount of fecal bacteria solution warrants further experimental determination [60], and there is also no clear consensus on the best method of preservation [67,68,71,72].
Delivery approaches
We consider differences in treatment and the preparation of fecal specimens,and patient acceptance of the different delivery methods.The current delivery approaches for FMT include the following: (1) nasogastric,nasoduodenal,or nasal-jejunal tube;(2) capsule;(3) colonoscopy (stool deposited into the right colon or terminal ileum);(4) oral;and (5) enema [2,73].Table 3 shows there are notable differences among delivery methods.Colonoscopy is a good option for the delivery of FMT both in children and adults[72,74–77].Compared with other methods,the treatment effects of colonoscopy are better in pediatric patients;however,colonoscopy is invasive,requires sedation,has the standard risks of colonoscopy,and the effectiveness may be limited within the colon (i.e.,not the entire intestine) [78].Capsule technology,which has emerged in recent years,is an effective delivery approach for pediatric FMT and can overcome the psychological problems of “oral feces” [71],but it is very expensive and has high technical requirements that exceed the capabilities of most hospitals.Specifically,an oral capsule is unsuitable in children because an oral capsule has the risks of becoming lodged in the esophagus and aspirated.At the same time,the effectiveness of an oral capsule is tentative because the number of fecal bacteria contained might not meet the requirements for FMT.A nasogastric/nasoduodenal/nasal-jejunal tube is easy to use and has the lowest technical requirements.Retrograde colonic enemas via an anal tube are also a widely used method of delivery.Enemas are easy to perform at home,even in pediatric patients.However,enemas are only effective for colondiseases because the transplanted microbiota may not be distributed throughout the entire intestine.Each FMT method has advantages and disadvantages.Clinicians should,therefore,select the appropriate approach based on the purpose and technical capabilities.
Safety of fecal microbiota transplantation
Although FMT has shown excellent therapeutic effects in pediatric diseases,it is worth noting that many AEs have been reported [34,79].The most common AEs included abdominal pain,gastrointestinal flatulence,diarrhea,constipation,fever,nausea,and vomiting [80,81].Serious complications,such as sedation-induced aspiration,perforation,bleeding,toxic megacolon with sepsis and peritonitis,fatal aspiration pneumonia,and death under anesthesia,have also been reported [80].Potential risks for pediatric FMT include infectious diseases,obesity,diabetes,atherosclerosis,cancer,NAFLD,and asthma [80].In the pediatric population,especially in newborns,specific AEs include belching,abdominal distention,abdominal pain,vomiting,diarrhea,fever,or transient CRP elevation [19,28,48,82].Kumagai reported that the AEs in clinical course of UC in a child who received FMT was transient fever and abdominal pain [83].From 2013 to 2018,Zhang focused on AEs in the short and long terms in pediatric FMT patients.Only a few children developed AEs in the short term,while few AEs occurred during the long-term follow-up.Indeed,no fatal AEs associated with FMT have been reported in children[19,82,84–87].
Perspectives and future
FMT has become widely practiced over recent years,and interest in FMT has surged among pediatricians and patients.Although the therapeutic effect of FMT in adults is satisfactory,the clinical practice of FMT in pediatrics needs to be improved and supplemented.The gap of FMT in the treatment of pediatric diseases reminds pediatricians that they need to consider many challenges,such as the required dosage,duration,onset,and end point of treatment.Future pediatric guidelines/studies should specify established indications versus potential/scientific indications.Additional larger,controlled,and prospective studies are needed to clarify both the safety and efficacy of FMT in pediatrics.
Author contributionsZSC:writing–review and editing.GX: formal analysis,writing–original draft.CZH: data curation. CZH and GX contributed equally as the first author.
FundingThis project was funded by the National Natural Science Foundation of China (30700917,81570465) and Minsheng Foundation of Joint Research Project of Liaoning Province2021JH2/10300129.
Data availabilityNot required.
Declarations
Conflict of interestNo financial benefits have been received from any party related directly or indirectly to the subject of this article.
Ethical approvalThis article does not contain any studies with human participants or animals performed by any of the authors.
 World Journal of Pediatrics2023年9期
World Journal of Pediatrics2023年9期
- World Journal of Pediatrics的其它文章
- Pediatric endocrinopathies related to COVID-19: an update
- Mapping the quality of prenatal and postnatal care and demographic differences on child mortality in 26 low to middle-income countries
- Clinical epidemiology and disease burden of bronchiolitis in hospitalized children in China: a national cross-sectional study
- Serum levels of the novel adipokine isthmin-1 are associated with obesity in pubertal boys
- Effects of fentanyl and sucrose on pain in retinopathy examinations with pain scale,near-infrared spectroscopy,and ultrasonography:a randomized trial
- Maternal and neonatal blood vitamin D status and neurodevelopment at 24 months of age: a prospective birth cohort study
