Clinical epidemiology and disease burden of bronchiolitis in hospitalized children in China: a national cross-sectional study
Jiao Tian · Xin-Yu Wang · Lin-Lin Zhang · Meng-Jia Liu · Jun-Hong Ai · Guo-Shuang Feng · Yue-Ping Zeng·Ran Wang · Zheng-De Xie
Abstract Background Bronchiolitis is a common acute lower respiratory tract infection (ALRTI) and the most frequent cause of hospitalization of infants and young children with ALRTI.Respiratory syncytial virus is the main pathogen that leads to severe bronchiolitis.The disease burden is relatively high.To date,few descriptions of the clinical epidemiology and disease burden of children hospitalized for bronchiolitis are available.This study reports the general clinical epidemiological characteristics and disease burden of bronchiolitis in hospitalized children in China.Methods This study included the face sheet of discharge medical records collected from 27 tertiary children’s hospitals from January 2016 to December 2020 that were aggregated into the FUTang Update medical REcords (FUTURE) database.The sociodemographic variables,length of stay (LOS) and disease burden of children with bronchiolitis were analyzed and compared using appropriate statistical tests.Results In total,42,928 children aged 0–3 years were hospitalized due to bronchiolitis from January 2016 to December 2020,accounting for 1.5% of the total number of hospitalized children of the same age in the database during the period and 5.31%of the hospitalizations for ALRTI.The male to female ratio was 2.01:1.Meanwhile,more boys than girls were observed in different regions,age groups,years,and residences.The 1–2 year age group had the greatest number of hospitalizations for bronchiolitis,while the 29 days–6 months group had the largest proportion of the total inpatients and inpatients with ALRTI in the same age group.In terms of region,the hospitalization rate of bronchiolitis was the highest in East China.Overall,the number of hospitalizations from 2017 to 2020 showed a decreasing trend from that in 2016.Seasonally,the peak hospitalizations for bronchiolitis occurred in winter.Hospitalization rates in North China in autumn and winter were higher than those in South China,while hospitalization rates in South China were higher in spring and summer.Approximately,half of the patients with bronchiolitis had no complications.Among the complications,myocardial injury,abnormal liver function and diarrhea were more common.The median LOS was 6 days [interquartile range (IQR)=5–8],and the median hospitalization cost was 758 United States dollars (IQR=601.96–1029.53).Conclusions Bronchiolitis is a common respiratory disease in infants and young children in China,and it accounts for a higher proportion of both total hospitalizations and hospitalizations due to ALRTI in children.Among them,children aged 29 days–2 years are the main hospitalized population,and the hospitalization rate of boys is significantly higher than that of girls.The peak season for bronchiolitis is winter.Bronchiolitis causes few complications and has a low mortality rate,but the burden of this disease is heavy.
Keywords Bronchiolitis · Children · Clinical epidemiology · Disease burden · Respiratory syncytial virus
Introduction
Bronchiolitis is a common acute lower respiratory tract infectious (ALRTI) disease in infants and children that mainly occurs in children aged under 3 years old,especially those under 2 years old.The peak age of onset is 2–6 months.Bronchiolitis is often associated with infectious wheezing in infants.This disease is primarily caused by respiratory syncytial virus (RSV) infection,followed by rhinovirus [1].Infections with other viruses,such as influenza virus,parainfluenza virus,adenovirus,and Boca virus,may also cause this disease.In addition,bacterial pathogens such asBordetella pertussisand atypical pathogens,includingMycoplasma pneumoniae,Chlamydia pneumoniae,andChlamydia trachomatis,have been detected in patients with bronchiolitis [2].Bronchiolitis is also the most common cause of hospitalization in infants.In total,150 million new-onset bronchiolitis cases are reported worldwide every year,of which 2%–3% require hospitalization.In the United States (US),approximately 100,000 patients with bronchiolitis require hospitalization each year [3].Shi et al.also found that ALRTI caused by RSV,the major pathogen of bronchiolitis,is responsible for approximately 3.2 million hospitalizations and approximately 60,000 deaths annually in children under 5 years old worldwide [4].Furthermore,bronchiolitis imposes a heavy economic burden on society.For example,between 2000 and 2015,the average cost of hospitalized children with bronchiolitis under 2 years old in Portugal was approximately EUR 900 per capita [5].Despite the differences in medical conditions and costs in different countries,China,a developing country with the world’s second largest child population,suffers from severe health pressure and a high socioeconomic burden from bronchiolitis.
The incidence and prevalence of bronchiolitis have clear seasonal characteristics.Since the disease is mainly caused by RSV infection,its seasonal characteristics are similar to those of the local RSV epidemic season [6].The prevalence of RSV is affected by latitude and meteorological conditions,and its epidemic seasons vary by region and latitude.For example,the epidemic season of RSV infection in northern China is usually winter,while that in southern China is spring or summer.Bronchiolitis mainly involves bronchioles with a diameter of 75–300 μm,resulting in extensive inflammation and edema of the small airways.Children with bronchiolitis mainly present with symptoms of lower airway obstruction,such as wheezing,shortness of breath,and three concave signs.This disease may be benign and self-limited,but the severity of the disease varies among children.Most children with bronchiolitis recover completely without sequelae,while severe cases may require hospitalization and even oxygen or mechanical ventilation.Children who are not treated promptly may develop respiratory failure or heart failure with the progression of the disease,which seriously threatens the safety of children.Statistics show that 2%–3%of hospitalized children require mechanical ventilation [3,7],and approximately 34%–50% of children with bronchiolitis will develop an airway hyperresponsiveness disease [8].Generally,symptomatic and supportive treatments are the mainstays in the management of bronchiolitis.Likewise,no drugs or vaccines are currently available to treat or prevent RSV.
Currently,limited multicenter studies have been conducted to assess the clinical epidemiological characteristics and disease burden of pediatric bronchiolitis in China.Due to the application of the electronic medical record management system for inpatients in the hospital,the basic and essential medical data generated during hospitalization can be aggregated into and presented in the face sheet of discharge medical records (FSMRs) [9].Based on the national pediatric patient medical record database,FSMR data from hospitalized children in 27 tertiary children’s hospitals from January 2016 to December 2020 were collected,and relevant information was extracted for a retrospective analysis.The purpose of this study was to summarize and provide clinicians with relevant data on the clinical epidemiology and disease burden associated with bronchiolitis in hospitalized children in China.
Methods
Data source
Futang Research Center of Pediatric Development (FRCPD),the first nonprofit social service organization engaging in pediatric research in China,was founded in 2016.As of December 2020,FRCPD had 36 provincial and municipal medical institutions and established a multi-tiered pediatric diagnosis and treatment network. Detailed information regarding the FRCPD is available at http:// www.futang.org/ about/ fu-tang-jie-shao.htm.FRCPD has been collecting FSMR data from its member hospitals since December 2015.In 2020,FRCPD developed a system for reporting and aggregating FSMR data,with dedicated stafforganizing and reviewing uploaded data.The data are shared among member hospitals,which will improve the efficiency of data utilization and promote the common development and cooperation of FRCPD hospitals.As the convening unit,the National Center for Children's Health (Beijing),Beijing Children's Hospital,Capital Medical University collected the FSMRs for children hospitalized in 27 tertiary children’s hospitals (21 of which are located in the provincial capital)under the FRCPD to form the FUTang Updating medical REcords (FUTURE) database [10].The data for this study were derived from the FUTURE database,which covers the FSMR information of hospitalized children in 27 tertiary children’s hospitals within the FRCPD framework.
Inclusion and exclusion criteria
Inclusion criteria were as follows: (1) this retrospective study collected basic medical information for all children hospitalized with bronchiolitis between January 1,2016,and December 31,2020,in the FUTURE database.The 10th Revision of International Statistical Classification of Diseases and Related Health Problems (ICD-10) was adopted as the selection criteria for primary screening and classification of diseases;(2) patients aged <3 years old at the time of admission.
Exclusion criteria were as follows: patients with incomplete data,such as sex,age,diagnosis,and disease burden.
Study variables
For patient data included in the study,we extracted relevant medical information,such as sex,age,length of stay (LOS),admission diagnosis,complications,and hospitalization expenses,for analysis.Demographic information is shown in Table 1.We grouped patients by sex,age,region,LOS,and complications.Since the onset of bronchiolitis is mainly in infants and young children,this study included hospitalized children aged less than 3 years old and divided them into five groups according to age (days;months;years),including 0–28 days,29 days–6 months,6 months–1 year,1–2 years,and 2–3 years.The 27 children’s hospitals were grouped into seven geographic regions: East China,North China,Central China,Northwest China,Southwest China,South China,and Northeast China (Supplementary Table 1).
Statistical analysis
The number of children hospitalized for bronchiolitis is reported as an absolute percentage.Categorical variables,such as sex,age,region,year of admission,and complication groups,are described in absolute percentages.LOS and expenditure are presented as the medians and interquartile ranges (IQRs) to assess central and discrete trends in the data.For unordered categorical variables,comparisons between groups were performed using the Chi-square test or Fisher's exact test.For non-normally distributed data and ordered categorical data,the nonparametric Wilcoxon test or KruskalWallis test was used for comparisons between groups.All data were statistically analyzed with SPSS 19.0 software (SPSS Inc.,USA).APvalue <0.05 was considered statistically significant.
Ethical approval
This study was approved by the Ethics Committee of Beijing Children’s Hospital,Capital Medical University (approval number: 2022-E-064-R).The requirement for informed consent from patients was waived because the analysis only involved a retrospective analysis of pooled data from medical records.Our data were completely deidentified and anonymized to protect privacy.
Results
Demographics
According to the ICD-10 disease code,the FSMR information of hospitalized children with bronchiolitis from January 1,2016,to December 31,2020,was collected in the FUTURE database (Table 1).During this period,42,928 children were hospitalized for bronchiolitis,accounting for 1.5% (42,928/2,853,116) and 5.31% (42,928/808,166) of the total and ALRTI hospitalizations of patients less than 3 years of age in this database,respectively.Among them,66.80% (28,676 patients) were male,and 33.20% (14,252 patients) were female,with a male to female ratio of 2.01:1.
The proportion of males was higher than that of females in different regions,age groups,admission years and residences (Fig. 1 a–d).As shown in Table 1,in terms of the age of onset of bronchiolitis,the proportion of children aged 1–2 years was the largest,accounting for 49.60% (21,292 patients),and children aged 29 days–6 months ranked second,with a proportion of 29.55% (12,687 patients),followed by 2–3 years (12.79%,5490 patients),6 months–1 years(7.97%,3422 patients),and 0–28 days (0.09%,37 patients).Regarding the regional distribution,the number of children hospitalized with bronchiolitis in East China was the largest (54.04%,23,199 patients),followed by Central (26.30%,11,288 patients),South (9.26%,3975 patients),Northwest(6.06%,2602 patients),North (2.05%,878 patients),Southwest (1.64%,704 patients),and Northeast China (0.66%,282 patients).Then,we found that bronchiolitis-related hospitalizations initially increased from 2016 to 2017 but have been decreasing since 2017.Finally,a significant seasonal trend in monthly hospitalizations was observed,presenting a significantly higher rate in winter (December–February of the following year) than in other seasons (Fig. 2).Hospitalized children with bronchiolitis living in urban and rural areas accounted for 58.71% (25,202 patients) and 41.29%(17,726 patients) of the total patients,respectively.The hospitalization rate of urban children was higher than that of rural children,regardless of sex,age,and year of admission (P<0.001).However,in East China,the number of hospitalized children was higher in rural areas than in urban areas (Supplementary Table 2).Between 2016 and 2020,the median LOS of hospitalized patients with bronchiolitis was 6 days (IQR=5–8),and the median expense was 758.49 United States dollars (USD) (IQR=601.96–1029.53).
Proportion of hospitalizations for bronchiolitis by region,age,year,and month
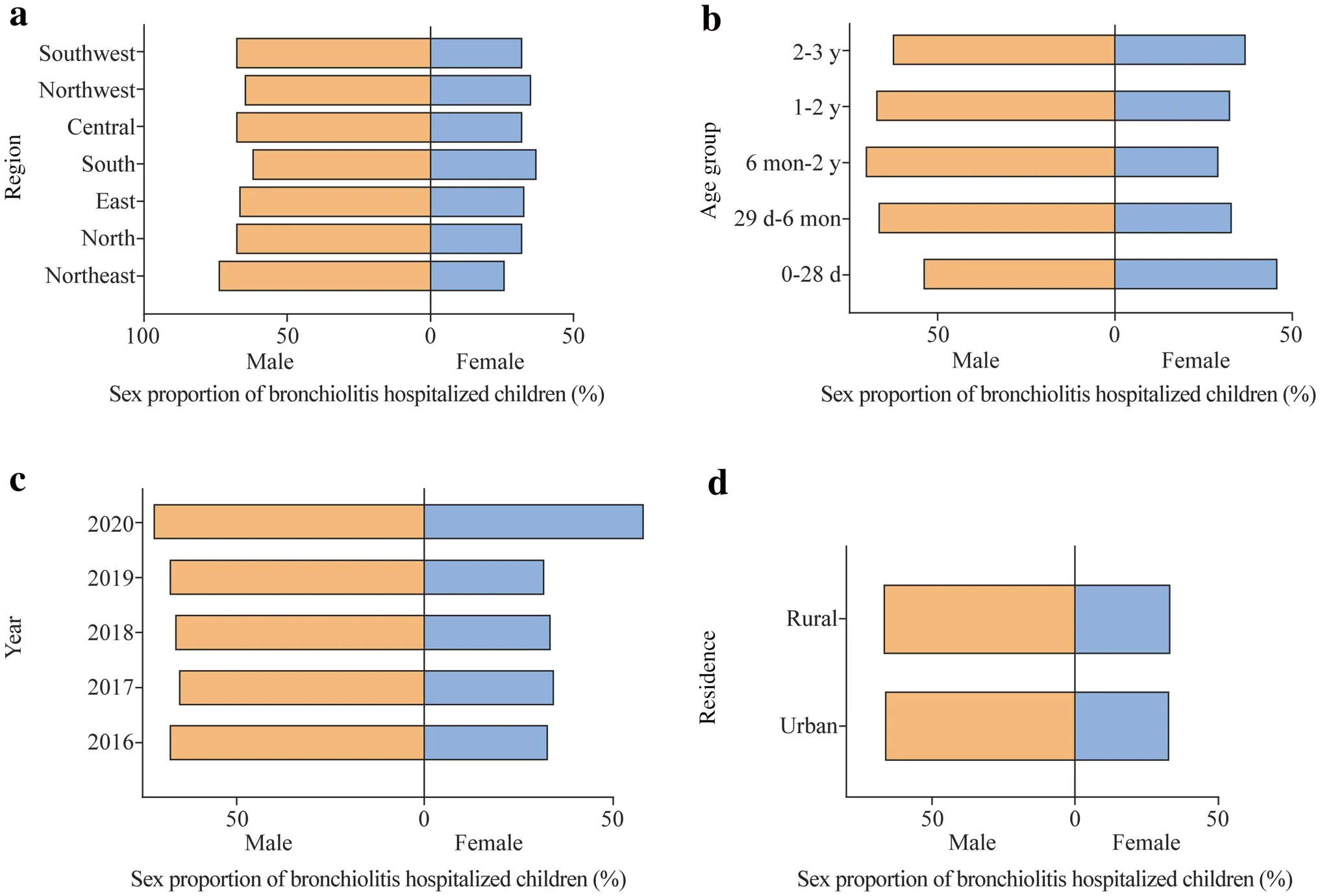
Fig.1 Sex ratios of children hospitalized with bronchiolitis.Sex ratios in different regions (a),age groups (b),years (c),and residences (d)
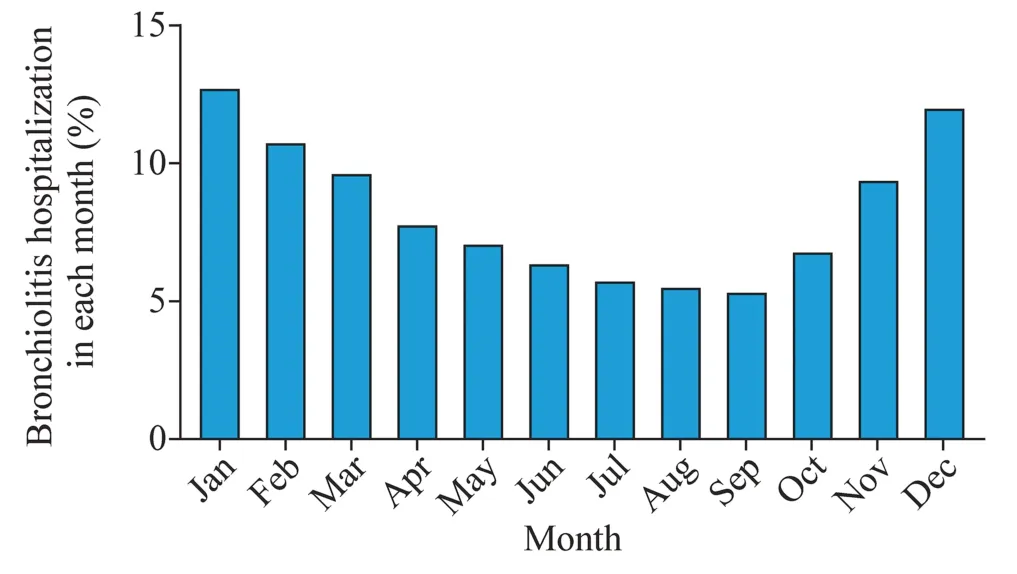
Fig.2 Proportion of hospitalizations for bronchiolitis in different months
We analyzed the characteristics of inpatients with bronchiolitis according to region,age,admission year,and month.First,the proportion of hospitalized patients with bronchiolitis to the total number of hospitalized patients was compared after stratification based on the four indicators.As shown in Fig. 3,in terms of age,infants aged 29 days–6 months had the highest hospitalization rate at 2.85% (12,687/444,953),followed by infants aged 6 months–1 year,1–2 years,2–3 years,and 0–28 days,with rates of 2.53% (3422/135,268),2.06% (21,292/1,036,103),0.82% (5490/669,550),and 0.01% (37/567,242),respectively(Fig. 3 a).Regionally,the hospitalization rate for bronchiolitis was the highest in East China (2.60%,23,199/890,733),and South China and Central China ranked second and third,accounting for 2.08% (3975/190,866) and 1.98%(11,288/569,021),respectively (Fig. 3 b).We found that between 2016 and 2020,the proportion of hospitalizations for bronchiolitis decreased each year,from 2.39%(14,259/596,629) in 2017 to 0.33% (1481/450,276) in 2020(Fig. 3 c).Our data indicated that the proportion of bronchiolitis-related hospitalizations varied significantly by month,with the lowest hospitalization rate in September at 0.97%(2314/237,523),then increasing monthly until reaching the highest rate in February (2.35%,4653/197,943),and finally decreasing gradually from March to August (Fig. 3 d).
In addition,we analyzed the proportion of bronchiolitis hospitalizations to ALRTI hospitalizations by region,age,and year and month of admission.As shown in Fig. 4,the proportion of bronchiolitis hospitalizations to total hospitalizations was similar across subgroups.Among all age groups,the highest hospitalization rate was observed in children aged 29 days–6 months (6.38%,12,687/198,897),and the lowest was observed in children aged 0–28 days (0.95%,282/29,805;Fig. 4 a).Among the regional groups,ALRTI inpatients in East China had the highest proportion of hospitalizations due to bronchiolitis (9.66%,23,199/240,274;Fig. 4 b).In terms of years,although the hospitalization rates in 2016 and 2017 were comparable,they showed a decreasing trend each year (Fig. 4 c).The proportion of bronchiolitis hospitalizations to ALRTI hospitalizations varied slightly between months,with the highest values recorded in February and March and the lowest value recorded in September,but this difference was not significant (Fig. 4 d).
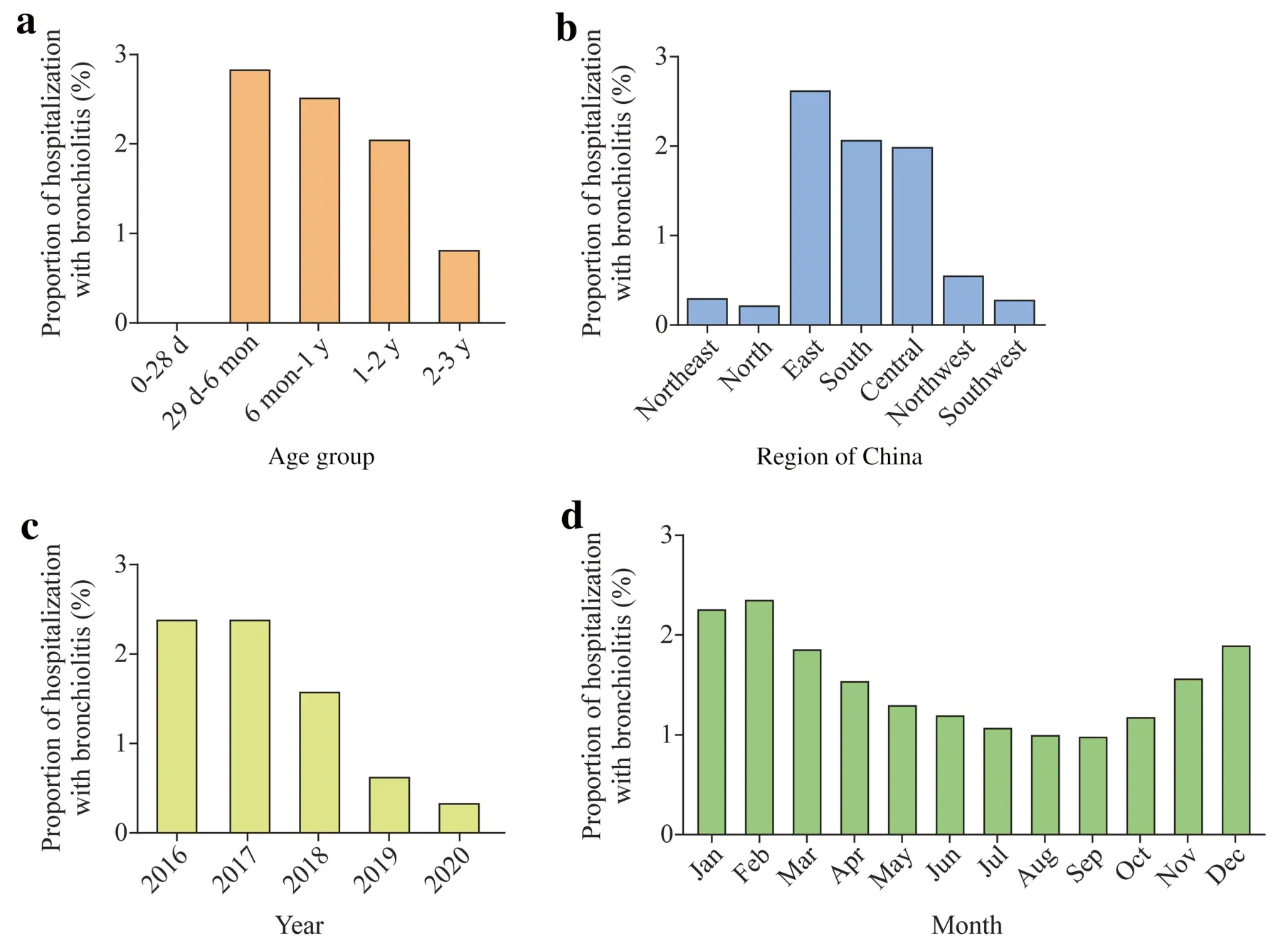
Fig.3 The proportion of hospitalizations for bronchiolitis among the total number of hospitalizations in different age groups (a),regions (b),years (c) and months (d)
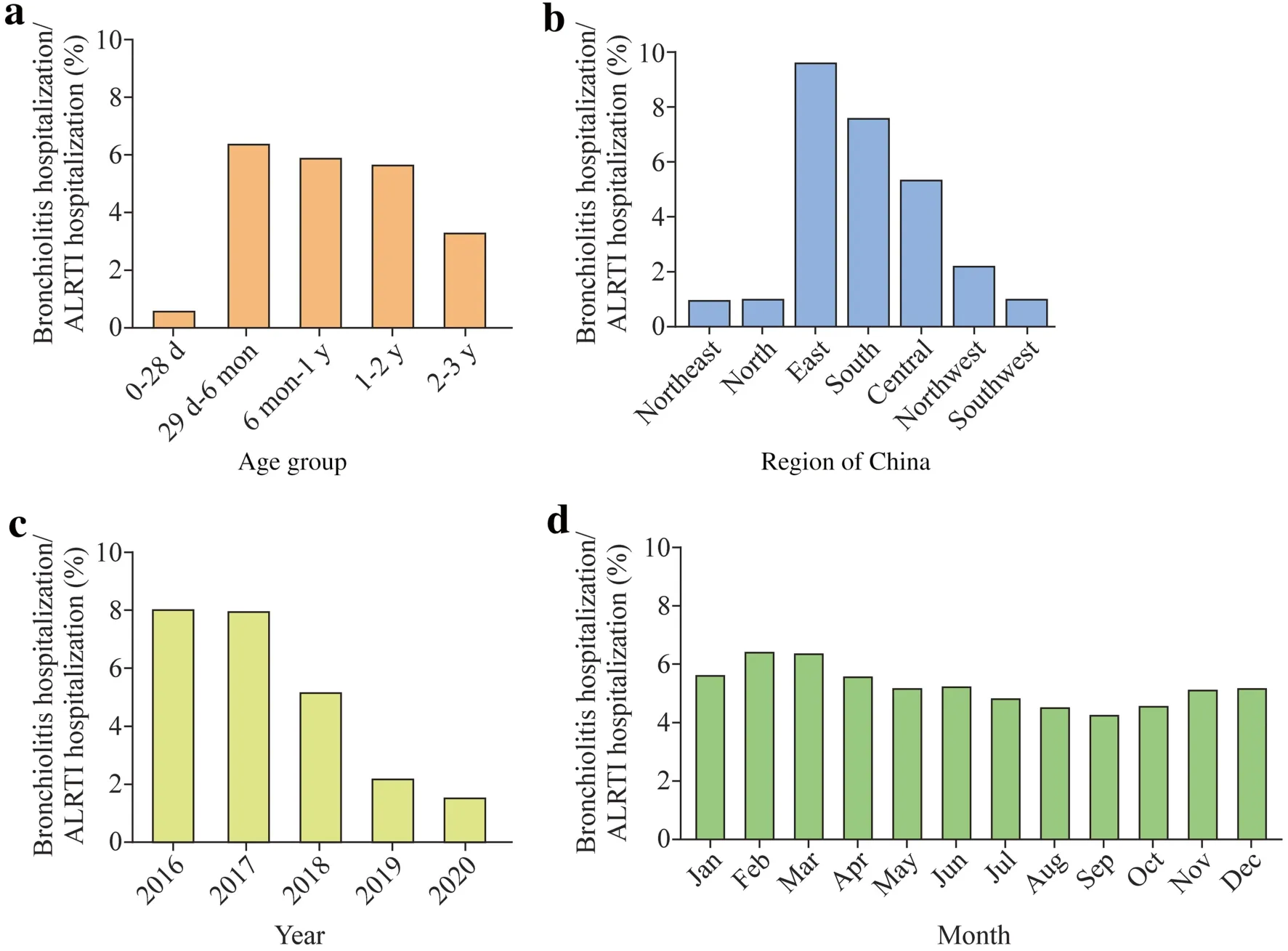
Fig.4 Proportion of bronchiolitis hospitalizations to ALRTI hospitalizations in different age groups (a),regions (b),years (c) and months (d).ALRTI acute lower respiratory tract infection
Seasonality and endemicity of hospitalization for bronchiolitis
According to this study,an apparent seasonality occurred in the time of admission for children hospitalized with bronchiolitis (Fig. 5).The hospitalization rate peaked from December–February every year,gradually decreased until reaching a trough from July–September,and then gradually increased to a peak from December–February.Furthermore,we separated the locations of inpatients with bronchiolitis according to the geographic locations of 27 children’s hospitals using Qinling–Huaihe as the dividing line between northern and southern China.Fifteen hospitals were located in northern China,and 12 hospitals were located in southern China.We plotted line graphs to show the ratio of bronchiolitis inpatients per month to the total number of hospitalizations in northern and southern China (Fig. 6).We noticed seasonal differences in bronchiolitis hospitalization rates in northern and southern China.The seasonal characteristics observed in northern China were more significant,showing that the bronchiolitis hospitalization rate increased rapidly in autumn and winter (September to December),peaked in December (24.48%,962/3929),began to decrease substantially after January and then decreased to the lowest value in April (2.83%,111/3929).However,in southern China,the seasonal fluctuation in the monthly bronchiolitis hospitalization rate was relatively moderate.Beginning in September,the bronchiolitis hospitalization rate in northern China was higher than that in southern China and was maintained until January of the following year.
Complications and comorbidities
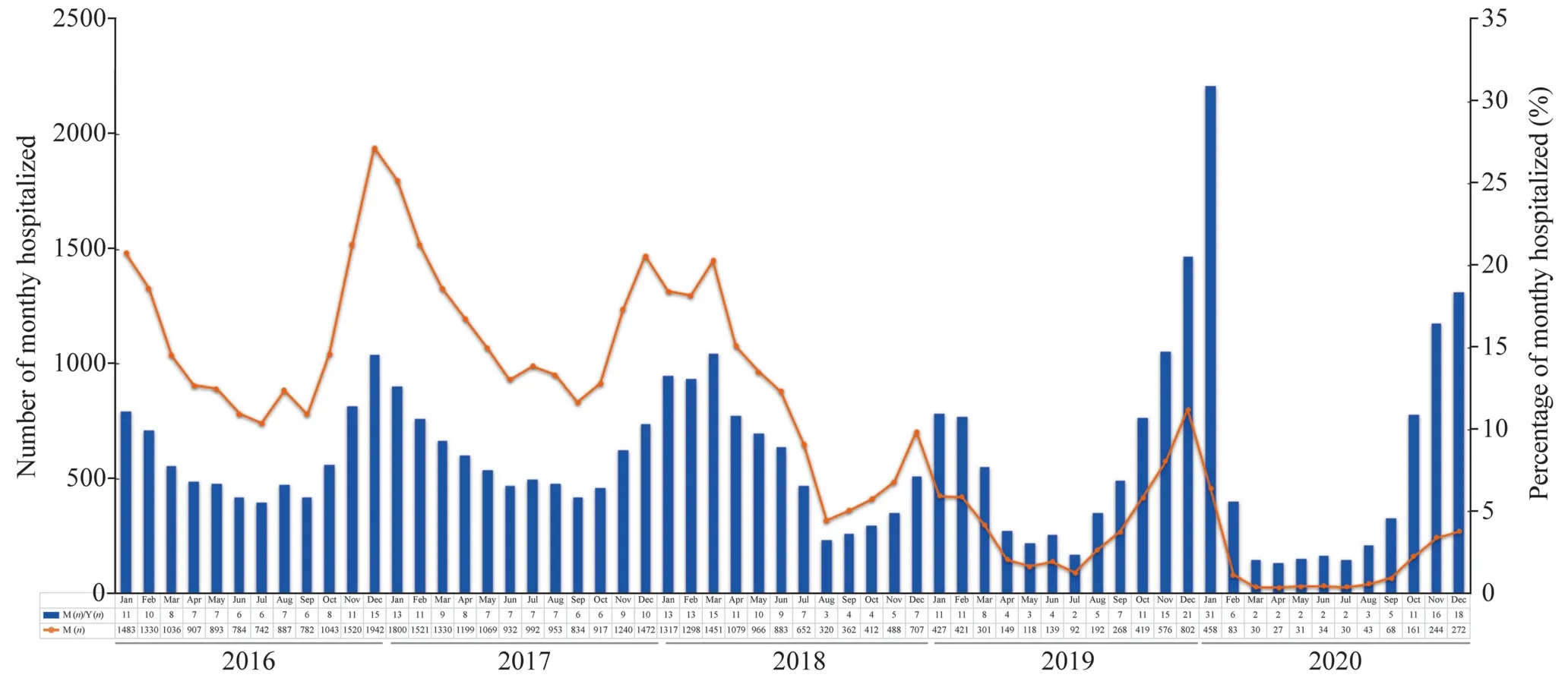
Fig.5 Number and proportion of children hospitalized with bronchiolitis from January 2016 to December 2020. M month,Y year
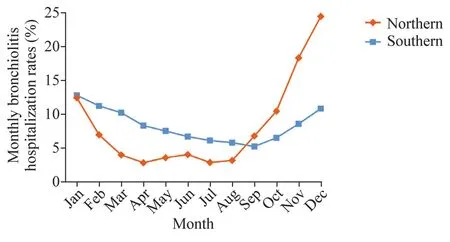
Fig.6 Proportion of hospitalizations for bronchiolitis by month in southern and northern China
Among hospitalized patients diagnosed with bronchiolitis,46.09% (19,786/42,928) had no complications,15.69%(6737/42,928) had bronchiolitis-related complications,and 38.22% (16,405/42,928) had other comorbidities (Fig. 7 a).We ranked the incidence of bronchiolitis-related complications (Fig. 7 b),with myocardial damage ranking the highest at 3.59% (1540/42,928),followed by abnormal liver function at 2.71% (1163/42,928).The incidences of diarrhea,neutropenia,and sepsis were 2.48% (1064/42,928),2.09%(897/42,928) and 1.11% (478/42,928),respectively.Moreover,we performed a statistical analysis of the sociodemographic information of patients with the top five complications and those without complications.We observed differences in complication rates by sex,age group,and region.Overall,male patients were more likely to experience complications than female patients;patients in the 1–2 years group had the highest incidence of complications.The incidences of myocardial injury,diarrhea,and sepsis in hospitalized children in Central China were higher than those in other regions,and liver function abnormalities and neutropenia mainly occurred in hospitalized patients in East China (Supplementary Table 3).
Length of stay and hospitalization expenditures
In this study,the LOS and hospitalization expenditures of children with bronchiolitis were statistically analyzed(Table 2).The results revealed significant differences in LOS and hospitalization expenses of patients stratified by sex,region and hospitalization years (P<0.001).Specifically,males had a longer LOS (Z=23.408,P<0.001) and higher hospitalization expenses (Z=69.65,P<0.001).A significant difference in the median LOS was not observed among age groups.The highest median hospitalization expense was incurred by patients aged 0–28 days,and the difference was statistically significant in each age group (Z=37.157,P<0.001).Hospitalized children in Northeast and Southwest China had the longest LOS,while children in South China had the lowest hospitalization expenses.Significant differences were observed in the LOS of children with different places of residence but not in the median LOS,and the hospitalization expenditures for children in urban areas were lower than those in rural areas.No significant difference in median LOS was observed among years;the hospitalization expenses were lower in 2017 and 2018,while the expenses were the highest in 2020.
Regarding the association between complications and LOS or hospitalization expenses (Fig. 8),we noted no difference in LOS between patients with and without complications (Fig. 8 a),but children without complications incurred lower hospitalization expenses.Furthermore,patients complicated with abnormal liver function had the longest LOS and the highest hospitalization expenses,while children with other complications exhibited no obvious difference in LOS or expenditures (Fig. 8 b).
Death events
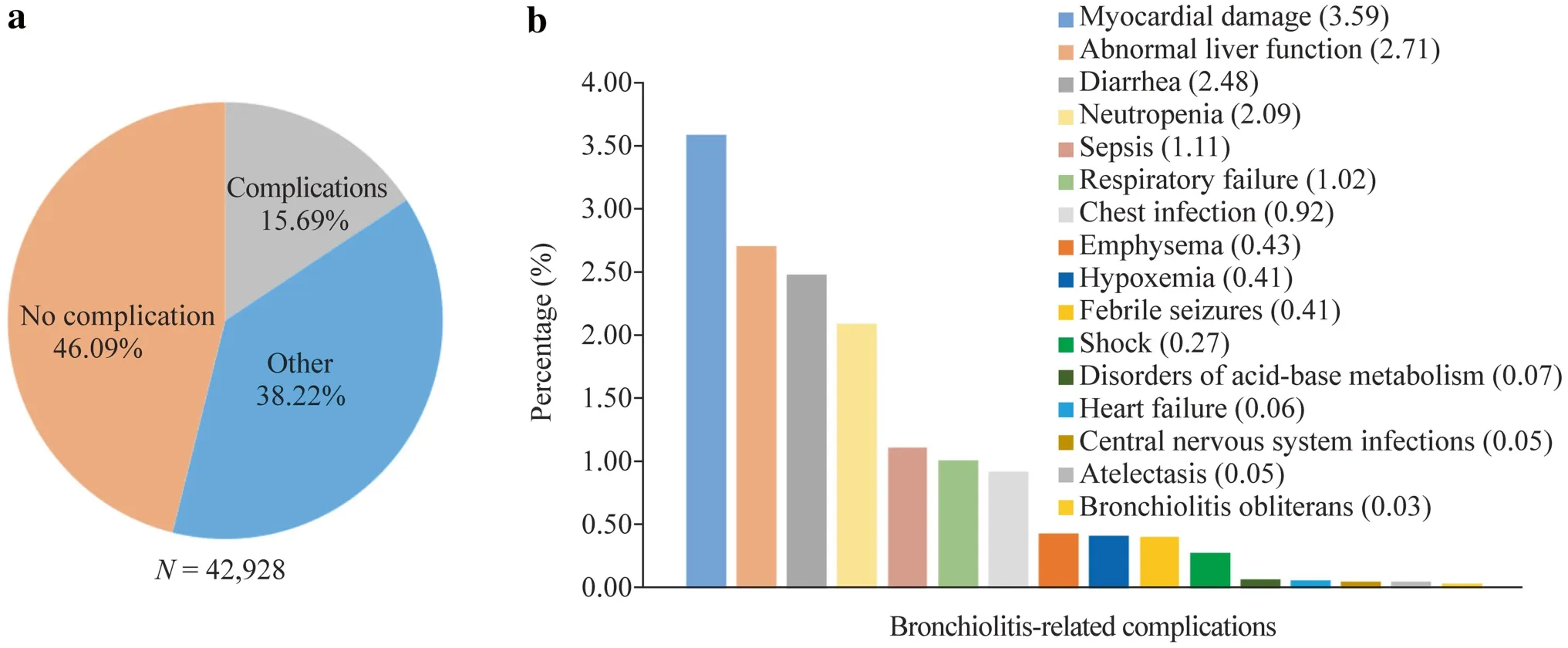
Fig.7 Complications and comorbidities of bronchiolitis.Overview of complications in children hospitalized with bronchiolitis (a) and the distribution of bronchiolitis-related complications (b)
Of the 42,928 children with bronchiolitis included in this study,eight died during hospitalization,accounting for 0.02% (8/42,928,Supplementary Table 4),including six boys and two girls.In terms of age,three patients were under 1 year,four patients were 1 year,and one was 2 years.Regionally,three patients each from East and South China died,and one patient each from Central and North China died.Five Han patients and three non-Han patients died.Shock and respiratory failure occurred in five patients,one dead child was immunocompromised,and no complications occurred in two patients.
Discussion
Bronchiolitis is a common ALRTI in infants and young children and is mainly caused by RSV infections.The disease typically occurs in children less than 3 years old and is one of the most substantial health burdens for infants worldwide.This study summarized and analyzed FSMR data from children hospitalized with bronchiolitis in mainland China from 2016 to 2020.
According to our results for the bronchiolitis hospitalization rate,among children under 3 years,1500 children per 100,000 total hospitalizations and 5310 children per 100,000 ALRTI hospitalizations were hospitalized for bronchiolitis,suggesting a large group in China.Furthermore,since bronchiolitis is a self-limited disease requiring hospitalization in only 2%–3% of patients,its morbidity rate is much higher than its hospitalization rate.Hence,the burden of bronchiolitis is concerning and warrants further attention.
Our results revealed that more boys than girls were hospitalized for bronchiolitis and that hospitalization varied by region,age,and year of hospitalization,consistent with the findings reported in previous studies.Tan et al.reported the epidemiological characteristics of bronchiolitis in Suzhou,China,where the hospitalization rate for boys was twice as high as that for girls [11].Similarly,Ghazaly et al.documented that males accounted for 63% of the children with bronchiolitis who were admitted to the pediatric intensive care unit of St.Mary’s Hospital in London,United Kingdom[12].The reason may be related to the differences in the development of the lung and respiratory tract between sexes and heredity [13,14],but the specific mechanism warrants further exploration.
Our results showed that the main age group of hospitalized children with bronchiolitis in Chinese mainland is mainly the 29 days–6 months age group,and infants aged 29 days–6 months constituted the highest proportion of ALRTI hospitalizations,confirming that this age group is prone to bronchiolitis.Although different,hospitalization rates and morbidity rates have been somewhat comparable in clinical epidemiological evaluations.This finding is similar to those reported in other countries.Hall et al.[15]reported that 58% of children hospitalized with bronchiolitis in the US are infants aged 0–5 months.A cohort study in Spain indicated that among children younger than 2 years hospitalized with bronchiolitis,86.2% of cases occur within 5 months,11.1% occur in 6–11 months,and only 2.7% of cases occur in 1–2 years.The occurrence of bronchiolitis in infants within 6 months of age may be related to the gradual decrease in the titers of maternally transmitted neutralizing antibodies against RSV in the first few months after birth,and it may also be related to the incomplete development of infant airway structure.For example,the smooth muscles of the capillary bronchus of infants are thin and few in number before 5 months after birth,and poor ciliary motor function also leads to incomplete clearance function,which increases the chance of respiratory tract infection.
Our data also revealed that the hospitalization rate for bronchiolitis decreased over time between 2017 and 2020,with the most significant decreases observed in 2019 and 2020.This result was slightly different from the data reported in a previous study conducted in China [16].Gao et al.analyzed the clinical data of 2998 children hospitalized for bronchiolitis from the First Hospital of Jilin University from 2005 to 2014 and concluded that the annual number of hospitalizations due to bronchiolitis was largely the same[16].However,several studies conducted in the US have shown a decreasing trend in the hospitalization rate for bronchiolitis in recent years [3,17].A cohort study in California showed that the rate of hospitalizations for bronchiolitis decreased from 12.9 cases per 100 infants per year to 9.3 cases per 100 infants per year in 1997–2011 [17].Hasegawa et al.reported that the hospitalization rate for bronchiolitis in children under 2 years old in the US decreased from 17.9% in 2000 to 14.9% in 2009 [3].We suspect that coronavirus disease 2019 (COVID-19) may be responsible for the significant reduction in hospitalization rates in 2019 and 2020.Recent studies have suggested that significantly fewer children are being hospitalized with bronchiolitis than before the COVID-19 pandemic,which is correlated with protective measures against COVID-19 [18–20].Friedrich et al.showed that the number of children under 1 year of age hospitalized for bronchiolitis decreased by more than 70% in Brazil during the COVID-19 pandemic [20].
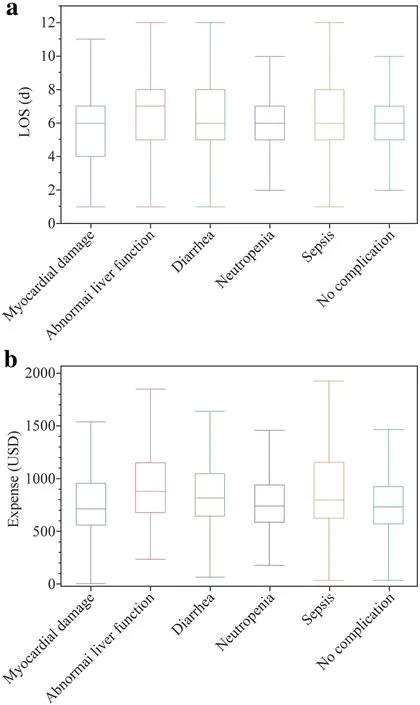
Fig.8 Length of stay (LOS) and hospitalization expenses for a range of complications.LOS for different complications (a) and hospitalization expenses for different complications (b)
The incidence of bronchiolitis exhibits obvious seasonality.Our data indicated that hospitalizations for bronchiolitis begin to increase in autumn,peak in winter,and then gradually decrease,consistent with data from 2016 to 2020.Additionally,seasonal differences in bronchiolitis were also observed in northern and southern China,consistent with the prevalence of RSV.The epidemic season of RSV in northern China is usually winter,while in southern China,it is spring or summer,consistent with the results of previous studies.Yu et al.analyzed the RSV epidemic season in Beijing (North China) and indicated that the RSV epidemic cycle starts from mid-October and lasts until mid-May of the following year [21].Chen et al.confirmed that the peak of RSV-associated bronchiolitis in Foshan,Guangdong (South China),occurs from April to May each year,and the peak period ofM.pneumoniae-associated bronchiolitis is from June to August,suggesting that,unlike northern and highlatitude regions,bronchiolitis is mainly prevalent in summer in southern China [22].Similar to China,the prevalence of bronchiolitis in the US begins in late December and peaks in early February [23].Meteorological conditions,including rainfall,ambient temperature and humidity,were reported to be related to RSV activity,while altitude,wind speed and dew point were reported to be associated with bronchiolitis-related hospitalization in children [24].This result may partly explain the difference in the proportion of children hospitalized with bronchiolitis in different geographical regions of China.
Bronchiolitis has a favorable prognosis with a lower rate of complications.Our data suggest that approximately half of children with bronchiolitis had no complications,approximately one-third had comorbidities related to other systems,and only one-sixth of children had bronchiolitis-related complications.Similar to other respiratory infectious diseases,children with bronchiolitis are prone to extrapulmonary complications,including gastrointestinal dysfunction and cardiovascular system and liver damage.In our report,the primary complications observed in children with bronchiolitis were myocardial damage,abnormal liver function and diarrhea,suggesting that these complications may be related to gastrointestinal dysfunction after respiratory tract infection,direct or indirect damage to related organs caused by viral infection,or hypoxia.Myocardial injury associated with bronchiolitis or RSV infection has been widely reported,ranging in incidence from 35% to 55% [25,26],most of which manifests as transient elevations of troponin levels and rarely occurs in children without underlying cardiac diseases.Meanwhile,abnormal liver function is the most frequent complication occurring in children under 6 months and is determined by evaluating alanine transaminase (ALT) and aspartate transaminase (AST) levels as commonly used indicators to evaluate liver function.Giordano et al.noted that children with bronchiolitis may experience transient transaminase elevations during hospitalization,which are associated with severe respiratory symptoms [27].Nonetheless,elevated ALT and AST levels are transient and generally return to normal within seven days of admission[28].Neutropenia and sepsis are also the more common complications of bronchiolitis,ranking among the top five complications.Transient neutropenia has been observed following infection with viruses,including RSV.Sepsis-like syndrome in RSV-infected patients was reported as early as the late 1980s [29].Wahab et al.estimated its incidence to be 7.8% [30],and it is associated with a younger age of onset [31].
The results for the mean LOS and hospitalization expenditure of patients with bronchiolitis showed that although LOS was comparable between children with and without complications,children without complications had lower hospitalization costs.As mentioned above,complications such as myocardial damage,abnormal liver function,and neutropenia are mostly transient and therefore do not prolong LOS [28,32].However,patients with abnormal liver function had the highest LOS and expenditures.Neonatal hospitalization costs are the highest among all age groups,possibly because younger patients generally experience more severe conditions.
The underlying reasons for the higher hospitalization expenses of children in rural areas compared with children in urban areas may be associated with medical conditions and economic status.Differences in socioeconomic status also lead to an increased number of children hospitalized with bronchiolitis in urban areas than in rural areas.The highest hospitalization expenses in 2020 may be related to the hospitalization of children with severe symptoms during the COVID-19 pandemic.
Bronchiolitis is a self-limited disease with a low mortality rate and a favorable prognosis in children without underlying diseases.In our study,eight children died,resulting in a fatality rate of 0.02%.In Western countries,deaths from bronchiolitis are also extremely rare.In Spain,the fatality rate of RSV-induced bronchiolitis in children under 2 years old is 0.14% [33].In developing countries,however,RSV infection constitutes the second leading cause of infant mortality [34].Boys are significantly more likely than girls to die from bronchiolitis,consistent with the sex profile of children hospitalized with bronchiolitis.Most deaths are attributed to shock and respiratory failure,corresponding to the view of Castillo et al.that deaths related to RSV infection are more frequent in children with sepsis or respiratory failure[35].Preterm birth,congenital heart disease,bronchopulmonary dysplasia,and immunodeficiency also contribute to an increased risk of death from bronchiolitis [36,37].
This study has some limitations.First,the FUTURE database only includes data on hospitalized children,not outpatient data.Most patients are treated as outpatients because bronchiolitis is a self-limited disease,and this study only included data from a subset of hospitalized patients with bronchiolitis in China.Second,only basic medical information of the patients is included in the FSMRs,and the lack of clinical information and laboratory test results makes further analysis difficult.Third,a long-term outcome assessment of bronchiolitis cannot be achieved due to a lack of regular follow-up of patients.
In conclusion,bronchiolitis is an important disease affecting infant health,accounting for 1.5% and 5.31% of the total and ALRTI hospitalizations of patients under 3 years of age,respectively.Among them,the hospitalization rate of boys was higher than that of girls,and the annual hospitalization rate of bronchiolitis decreased annually from 2017 to 2020.This disease is seasonal because its prevalence begins in early autumn,peaks in winter,and then decreases gradually.Some differences in the seasonal features of bronchiolitis were still observed in northern and southern China.Half of the children with bronchiolitis had no complications,and a few patients had complications such as myocardial damage,abnormal liver function,and diarrhea.Bronchiolitis has a better prognosis,with a fatality rate of only 0.02%,and shock and respiratory failure are the major causes of death.The median LOS for bronchiolitis was approximately six days,and the median hospitalization expenditure was 758 USD.This study will facilitate a better understanding of the clinical epidemiological characteristics of bronchiolitis in mainland China,thereby helping us formulate targeted strategies and surveillance and optimize the allocation of medical resources.
Supplementary InformationThe online version contains supplementary material available at https:// doi.org/ 10.1007/ s12519-023-00688-9.
AcknowledgementsWe are grateful to investigators from members of the Futang Research Center of Pediatric Development (FRCPD).
Author contributionsTJ contributed to conceptualization,data curation,methodology,writing of original draft,reviewing and editing.WXY contributed to data curation,methodology,reviewing and editing.ZLL contributed to investigation,methodology,reviewing and editing.LMJ contributed to investigation,methodology,reviewing and editing.AJH contributed to investigation and editing.ZYP contributed to data curation,software,analysis and interpretation of data.FGS contributed to data curation,software,analysis and interpretation of data.WR contributed to conceptualization,data curation,funding acquisition,methodology,supervision,validation,visualization,writing of original draft,reviewing and editing.XZD contributed to conceptualization,data curation,funding acquisition,methodology,supervision,validation,visualization,writing of original draft,reviewing and editing.All the authors listed have made a substantial,direct,and intellectual contribution to the work,and approved it for publication.
FundingXZD was supported by the CAMS Innovation Fund for Medical Sciences (2019-I2M-5-026) and the National Major Science &Technology Project (2017ZX10103004-004).
Data availabilityThe data generated during the current study are available from the corresponding author on a reasonable request.
Declarations
Ethical approvalThis study was approved by the Ethics Committee of Beijing Children's Hospital,Capital Medical University (approval number: 2022-E-064-R).The requirement for informed consent from patients was waived because the analysis only involved a retrospective analysis of pooled data from medical records.Our data were completely deidentified and anonymized to protect privacy.
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.The authors have no conflict of interest to declare.
 World Journal of Pediatrics2023年9期
World Journal of Pediatrics2023年9期
- World Journal of Pediatrics的其它文章
- Fecal microbiota transplantation in childhood: past,present,and future
- Pediatric endocrinopathies related to COVID-19: an update
- Mapping the quality of prenatal and postnatal care and demographic differences on child mortality in 26 low to middle-income countries
- Serum levels of the novel adipokine isthmin-1 are associated with obesity in pubertal boys
- Effects of fentanyl and sucrose on pain in retinopathy examinations with pain scale,near-infrared spectroscopy,and ultrasonography:a randomized trial
- Maternal and neonatal blood vitamin D status and neurodevelopment at 24 months of age: a prospective birth cohort study
