The management of the long head of the biceps in rotator cuff repair:A comparative study of high vs.subpectoral tenodesis
Edordo Frneshetti ,Edordo Giovnnetti de Sntis ,Alessio Plumo ,Mihele Piotti ,Lu L Verde ,Niol Mffulli,Frneso Frneshi
a Department of Orthopaedic and Trauma Surgery,Campus Biomedico University of Rome,Via Alvaro del Portillo 200,00100 Rome,Italy
b Department of Orthopaedics and Traumatology,Catholic University,Agostino Gemelli Hospital,00100 Rome,Italy
c Anca Surgical Center,Via Francesco Maidalchini 20,Roma,00152,Rome,Italy
d Department of Musculoskeletal Disorders,Via Salvador Allende,43,84081 Baronissi,Salerno,Italy
e Centre for Sports and Exercise Medicine,Barts and The London School of Medicine and Dentistry,Mile End Hospital,275 Bancroft Road,London E1 4DG,England,UK
f School of Pharmacy and Bioengineering,Keele University School of Medicine,Thornburrow Drive,Stoke on Trent ST4,England,UK
Abstract Background:Tenodesis of the long head of the biceps(LHB)is commonly undertaken during arthroscopic rotator cuff repair.We assessed the clinical and structural outcomes after high arthroscopic tenodesis(HAT)or mini-open subpectoral tenodesis(ST).We hypothesized that the clinical and structural results after HAT and ST are similar.Methods:We included 40 patients with rotator cuff tear and LHB tendinopathy.Twenty patients(7 women and 13 men;mean age:57.9 years;range: 56−63 years) were treated using HAT,and 20 patients (8 women and 12 men;mean age: 58.5 years;range: 55−64 years) were treated using ST.Functional evaluation was performed preoperatively and at 6 weeks,6 months,and 1 year after surgery,using the Constant Murley Score and Simple Shoulder Test scores;the LHB was evaluated using the LHB score.A Visual Analogue Scale was administered to all patients preoperatively and 2 days after surgery.Results: The postoperative total and pain subscale’s Constant scores were significantly higher in the ST group.Moreover,2 LHB score values were significantly different between the groups.The postoperative LHB total score in the ST and HAT groups averaged 86.9§4.1(mean§SD)points and 73.3 § 6.4 points,respectively.The Pain/Cramps subscale in the ST and HAT groups averaged 47.1 § 5.9 and 33.2 § 4.6 points,respectively.The 2 groups showed no difference in Visual Analogue Scale values(5.5 in the HAT group;5.8 in the ST group)postoperatively.One patient in the HAT group reported a secondary onset of Popeye deformity.Conclusion:Both high arthroscopic and mini-open ST of the LHB tendon produced reliably good functional results,but the ST group was associated with better postoperative clinical outcomes.
Keywords: Long head of the biceps;Shoulder;Shoulder arthroscopy;Subpectoral;Tenodesis
1.Introduction
Tendinopathy and lesions of the tendon of the long head of the biceps(LHB)are common causes of pre-and postoperative pain in patients undergoing arthroscopic rotator cuff (RC)repair.The surgical management of the LHB tendon is still debated,and currently both tenotomy and tenodesis are commonly undertaken.1Tenotomy of the LHB tendon is a reliable option for specifically selected individuals,particularly because of its decreased incidence of postoperative discomfort;it is a quick procedure,not requiring additional fixation,but it might lead to distal migration of the LHB.On the other hand,LHB tenodesis is generally performed in younger people,active patients (athletes and labourers),and people who want to avoid cosmetic deformity and cramping.2A tenodesis of the LHB has potential advantages over tenotomy because it preserves the length/tension relationship of the biceps muscle,preventing muscle atrophy and Popeye deformity.1A tenodesis of the LHB may be performed as an arthroscopic,open,or mini-open procedure3,4in several locations,including the upper portion of the bicipital groove,the proximal or distal portion of the bicipital groove,or the subpectoral 1 cm proximally to the inferior border of the pectoralis major tendon.5−8Residual pain after surgical treatment can lead to failure of the proximal tenodesis,which could be generated by the neural receptors placed in the biceps groove synovium.Only a very few recently published prospective comparative studies have investigated this topic.The present study prospectively assessed and compared clinical outcomes of patients after high arthroscopic tenodesis (HAT)vs.subpectoral tenodesis(ST).
2.Methods
This randomized prospective comparative study focused on analyzing clinical outcomes of 2 groups of patients undergoing arthroscopic RC repair and LHB tenodesis.The RC was repaired in all patients.Patients were placed preoperatively into 2 groups—the HAT group and the ST group—depending on the procedure they received.Surgical procedures were performed between 2015 and 2017.
Inclusion criteria included (1) having RC tears associated with LHB tendinopathy diagnosed clinically and observed on magnetic resonance imaging;(2)having symptoms for at least 6 months that were unresponsive to conservative management(nonsteroidal anti-inflammatory drugs,physical therapy,rest,and 1 local corticosteroid injection);(3)being between 55 and 65 years of age;and(4)having the RC tear classified as small,medium,or large.
Patients with histories of tobacco use and those who had metabolic or endocrine disorders,such as diabetes,hypercholesterolemia,obesity(body mass index>30 kg/m2),or thyroid diseases,were excluded from the study in order to minimize the role of these conditions in the results and to ensure similar baseline characteristics.Patients who had massive RC tears,episodes of shoulder instability,RC muscle fatty degeneration≥III according to the Goutallier classification,9presence of a subscapularis tear,radiographic signs of glenoid or greater/lesser tuberosity fractures,glenohumeral osteoarthritis,history of inflammatory joint disease,prior surgery affecting the relevant shoulder,inability to complete questionnaires,or cognitive disorders were excluded.
Patients were randomized preoperatively to 1 of the 2 groups—those who would receive HAT or those who would receive ST.We used a random-number table to allocate subjects.The table,which did not allow duplicate entries,was composed of 40 numbers with a minimum and maximum value of 1 and 40,respectively.The first 20 numbers were assigned to the high arthroscopic LHB tenodesis(HAT)group,and the next 20 were assigned to the subpectoral LHB tenodesis (ST) group.These assignments were then arranged in ascending order.This procedure produced a random sequence of consecutive treatment allocations.The study was approved by the Ethics Committee of the Campus Biomedico University of Rome.Written informed consent was obtained from all patients.
2.1.Surgery
After induction of general anaesthesia and peripheral interscalene nerve block,a standard posterior portal was used for the diagnostic arthroscopy.The biceps tendon was evaluated with no pump pressure (dry) because the intra-articular pressure of the fluid might compress vessels,causing the inflamed synovium to look normal.Because biceps tendinopathy is usually located at the intertubercular groove portion,the biceps tendon was pulled with a probe through the anterior portal into the glenohumeral joint to evaluate its mobility and structural lesions.
After decortication of the greater tuberosity with a motorized bur,a 5.0 mm single-loaded Corkscrew suture anchor(Arthrex Inc.,Naples,FL,USA) was inserted.The biceps tendon was adequately secured with 6 reversed post halfhitches.After fixation of the tendon,an electrocautery device was used to transect the biceps tendon proximal to the suture and to remove its intra-articular portion.The transverse humeral ligament was left intact.
ST was performed according to the technique previously described by Mazzocca et al.10At the beginning of this procedure,the biceps tenotomy was carried out at its insertion.The inferior border of the pectoralis major tendon was then palpated,with the arm abducted and internally rotated.On the medial aspect of the arm,a longitudinal,3 cm incision was made starting 1 cm proximal to the inferior border of the pectoralis.
After a careful dissection,the LHB tendon was pulled down,delivering it into the wound.To ensure appropriate tension and good cosmesis results,the biceps tendon was resected 20−25 mm proximally to the musculotendinous portion.Using a Krackow or whip-stitch configuration,No.2 Fiberwire (Arthrex Inc.) nonabsorbable sutures were woven into the proximal 15 mm of tendon.In this manner,the musculotendinous portion beneath the inferior border of the pectoralis major was positioned,and adequate interference fixation within bone was reached.The tendon was then fixed through a 15 mm-deep bone tunnel with an interference screw.
2.2.Clinical outcomes
Clinical and functional evaluation was performed preoperatively and at 6 weeks,6 months,and 1 year by a trained examiner not involved in the clinical management of these patients.To focus on pain perioperatively,a Visual Analogue Scale(VAS)questionnaire was administered to all patients preoperatively and 2 days after surgery to evaluate differences between mini-open and arthroscopic techniques.Functional outcomes were assessed using the Constant Murley11and Simple Shoulder Test (SST)12scores;a more specific evaluation of the tendon was performed using the LHB score.13The Constant Murley score (maximum 100 points) comprises 4 sections: pain,activities of daily living (ADLs),active range of motion,and strength.11The SST was developed to assess the affected shoulder during the patients’ ADLs.The SST consists of 12 questions with yes (1) or no (0) response options.Each question asks the patient to determine whether the injury affects his or her ability to perform a physical function.14The LHB score13(maximum 100 points) evaluates the following categories: biceps pain and muscle cramps,cosmesis,and flexion strength at the elbow.Flexion strength at the elbow was measured using an isometric dynamometer at 90˚ of elbow flexion and was repeated 3 times.No significant differences were observed between the dominant and nondominant side of healthy volunteers.15Therefore,the normal contralateral upper extremity was used in the evaluation of postoperative biceps strength measurement.
The postoperative protocol included a sling for 6 weeks with the elbow flexed 90˚and in neutral rotation to protect the LHB.Passive range of motion was initiated from Day 2 after surgery until the 6th week.Patients were clearly told to avoid elbow flexion and supination maneuvers against resistance for 6 weeks.
After assessment of the distribution by the Kolmogorov-Smirnov test,unpairedttests and Mann-WhitneyUtests were used to compare parametric and nonparametric variables,respectively.Mean,SD,and 95% confidence intervals(95%CIs)were calculated.Apvalue of<0.05 was considered statistically significant.SPSS Version 17.0 (SPSS,Chicago,IL,USA) was used to analyze the data.Prior power analysis was conducted to determine the minimum number of patients needed to power our study adequately.Power analysis showed that a total sample size of 40 patients (20 patients in each group) would provide a statistical power of 90%,with a 2-sided level of 0.05 to detect significant differences.
3.Results
Of the patients,35 did not meet the inclusion criteria and did not participate in the study.A total of 20 patients (7 women and 13 men;aged 57.9 § 3.2 years;ranged 56−63 years)were treated using HAT,and 20 patients(8 women and 12 men;aged 58.5 § 3.5 years;ranges 55−64 years) were treated using ST (Fig.1).Data regarding the patients’demographic characteristics are summarized in Table 1.In all patients,tenotomy with removal of the pathological portion of the LHB was performed.No patient was lost to follow-up,as shown in Fig.1.Data regarding the intraoperative findings are summarized in Table 2.
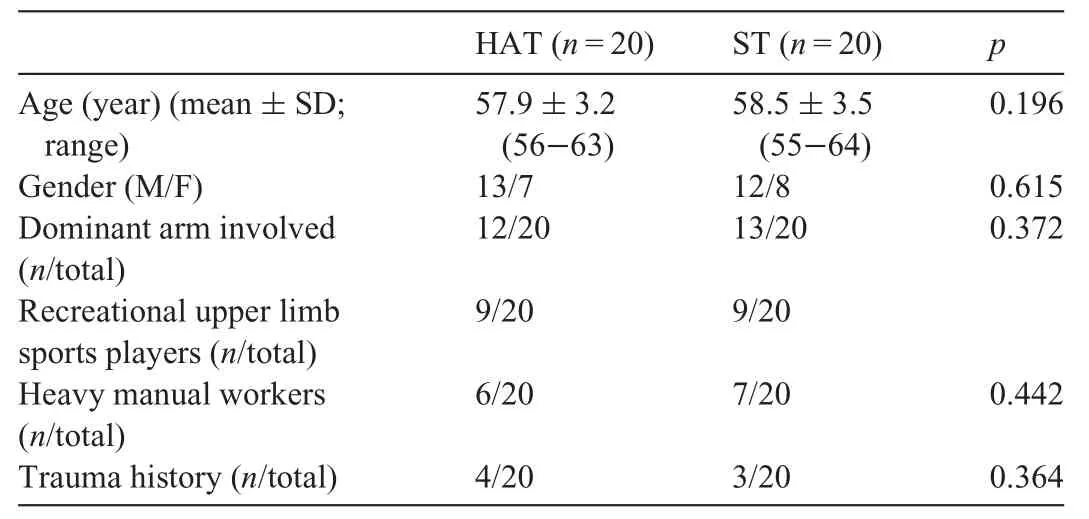
Table 1Demographic data of the 2 groups of patients.
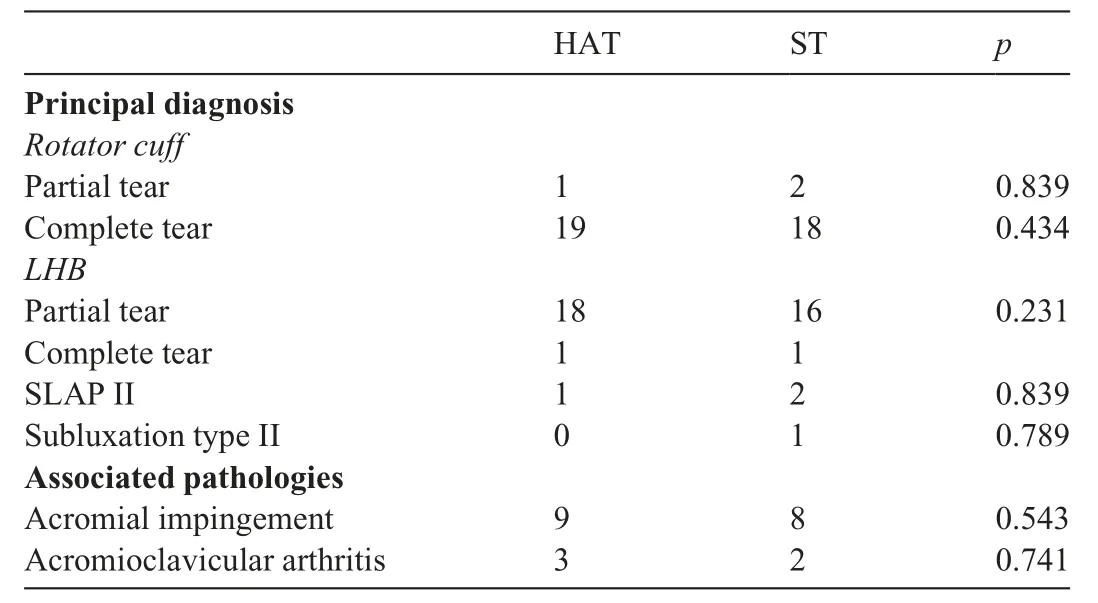
Table 2Intraoperative findings.
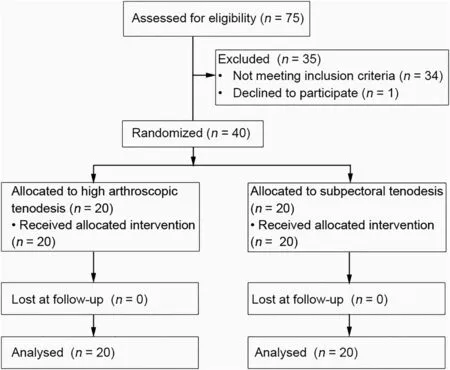
Fig.1.Flow diagram.
In the HAT group,there were 18 partial tears of the LHB tendon,1 superior labrum anterior and posterior (SLAP) II lesion,and 1 complete tear of the LHB tendon.There were 19 complete RC tears and 1 partial RC tear.Complete tears were treated by arthroscopic RC repair,whereas the partial tear was debrided.In the 9 patients with impingement,an acromionplasty was performed.An arthroscopic Mumford procedure16was performed in 3 patients with acromioclavicular osteoarthritis.
In the ST group,there were 16 LHB partial tears,2 SLAP II lesions,1 complete tear of the LHB tendon,and 1 subluxation type II.The principal diagnoses were 18 complete rotator cuff tears and 2 partial rotator cuff tears.Complete and partial tears were treated arthroscopically,as previously described.An acromionplasty was performed in 8 patients with impingement.An arthroscopic Mumford16procedure was performed in 2 patients with acromioclavicular arthritis.There were no statistical differences between the 2 groups regarding biceps pathology and associated lesions.The baseline characteristics of the 2 groups were comparable.
Clinical and functional outcomes are summarized in Table 3.In the ST group,at the last follow-up,the postoperative mean Constant score averaged 76.4 § 8.2 points.Regarding the postoperative subscales,an average of 13.9 §1.4 points was achieved for pain,17.4§2.0 points for ADLs,35.6 § 7.6 points for range of motion,and 9.3 § 2.8 points for strength.In the HAT group,at the last follow-up the postoperative Constant score averaged 69.2 § 6.7 points.Regarding the postoperative subscales,an average of 7.1§1.9 points was achieved for pain,17.3§2.3 points for ADLs,35.5§ 7.6 points for range of motion,and 9.3 § 2.8 points for strength.The postoperative total and pain subscale Constant scores were significantly higher in the ST group.No statistical difference in the SST was detected between the 2 groups.
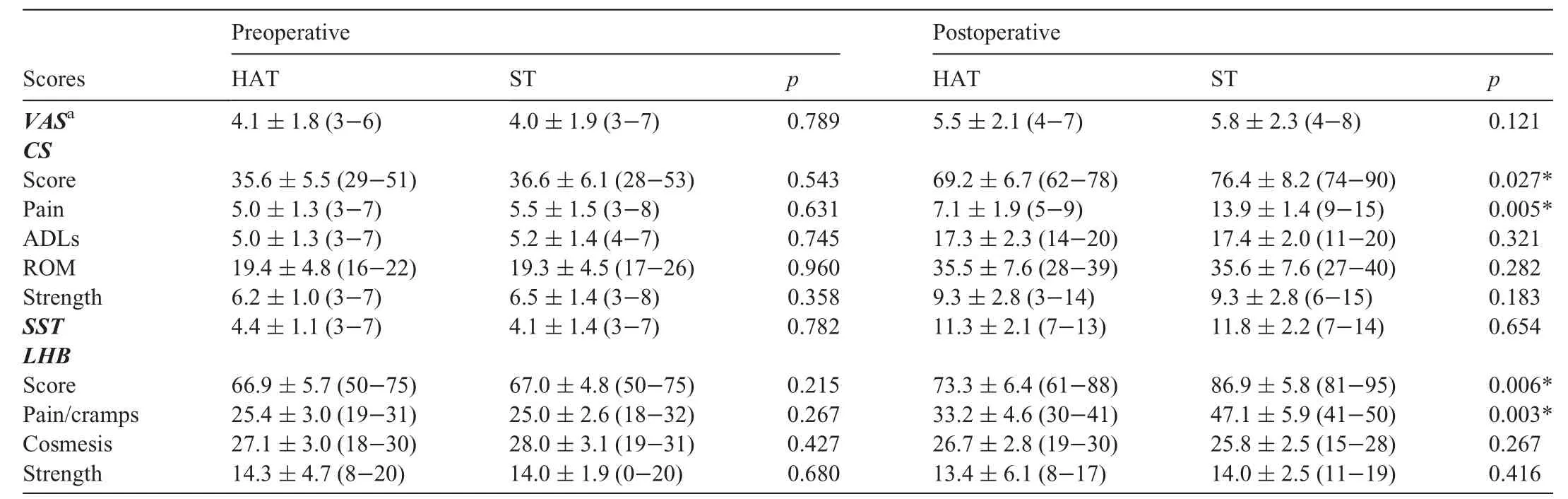
Table 3Clinical outcomes before treatment and at last follow-up(12 months).
In an evaluation of the LHB scores,the ST group averaged 86.9 § 5.8 points postoperatively.For the subcategories,an average of 47.1 § 5.9 points was achieved for pain and cramps,25.8 § 2.5 points for cosmesis,and 14.0 § 2.5 points for strength.The HAT group showed a mean LHB score of 73.3§ 6.4 points postoperatively.For the subcategories,an average of 33.2§ 4.6 points was achieved for pain and cramps,26.7§2.8 points for cosmesis,and 13.4 § 6.1 points for strength.For both the overall postoperative LHB score and the pain and cramps sections,there were significant differences between the ST group and the HAT group.Regarding VAS values,carried out on the 2nd postoperative day,there were no statistically significant differences between the 2 groups,with an average of 5.5 § 2.1 points and 5.8 § 2.3 points for the HAT and ST groups,respectively.In regard to complications,1 patient in the HAT group reported a secondary onset of Popeye deformity.
4.Discussion
The purpose of the current study was to compare the clinical and structural outcomes after HATvs.ST.In our study,patients who had undergone HAT and open ST of the LHB tendon showed significant improvements in Constant,SST,and LHB scores at the final follow-up (12 months).Postoperative pain,evaluated by the Constant and LHB subscales and influencing those 2 overall value scores,was significantly lower in patients after ST.In our population,only 1(2.5%) patient (who was in the HAT group) reported a secondary postoperative onset of the Popeye deformity.This finding could be explained by the stronger fixation provided by the interference screw when compared to anchor fixation.17No further complications were reported.
The management of the LHB is a major point in shoulder arthroscopy because it may have a strong influence on the final outcome of surgery.18,19The most common procedures proposed are biceps tenotomy and tenodesis.1Biceps tenodesis is generally performed in younger,active patients (athletes and labourers) and in individuals who want to avoid cosmetic deformity.Even though tenotomy of the biceps tendon provides pain relief and high patient satisfaction,20musclebelly retraction is more common with this procedure.21Tenodesis has emerged as a more popular technique in the recent past,and despite the different techniques,its use has increased significantly in the past few years.22
The goal of tenodesis is to preserve the length/tension relationship of the biceps muscle,avoiding muscle atrophy,pain,cramps,and Popeye deformity.The tenodesis can be performed in the upper aspect of the bicipital groove,in the proximal portion of the bicipital groove,in the distal portion of the bicipital groove,or in a subpectoral position.5,6,23Thus,the ideal LHB tenodesis location is still controversial.An upper tenodesis may allow the inflammation,usually present within the biceps groove,to persist,causing residual pain after tenodesis.24Mazzocca et al.25suggested that a more distal tenodesis could remove pain generators located within the groove.The differing incidences of postoperative pain could be explained according to the anatomical observations by Depalma and Callery,26who suggested that the intra-articular tenosynovitis of the LHB could extend distally into the bicipital groove.
In 2015,Brady et al.27pooled the data of 1083 patients who underwent arthroscopic biceps tenodesis at the articular margin by interference screw fixation.They observed a low surgical revision rate,a low rate of residual pain,and significant improvement in objective shoulder outcome scores in all patients.However,this study was a therapeutic case series,and only a single tenodesis method was investigated.
Given the recent increasing interest in this topic,several authors have tested different LHB tenodesis techniques,both arthroscopic and mini-open.In a retrospective study of 17 patients undergoing arthroscopic biceps tenodesis,Lutton et al.28evaluated the clinical outcomes related to tenodesis location,comparing those in the upper half of the groove to those in the lower half of the groove or the humeral shaft.Two patients,both with a tenodesis in the upper half of the groove,experienced persistent pain at 12 months.The preliminary results of Lutton et al.28suggested that a more distal tenodesis location may decrease the incidence of persistent postoperative pain at the bicipital groove.Our findings confirmed these observations.In a recent retrospective study of 72 patients,Jeong et al.29compared arthroscopic intracuff tenodesis (33 patients) and open subpectoral tenodesis (39 patients).They reported persistent bicipital tenderness in 1 patient(2.6%)from the group with open subpectoral tenodesis and in 8 patients (24.2%) from the group with arthroscopic intracuff tenodesis(p=0.012).
A retrospective study of 127 biceps surgeries with a mean follow-up of 22 months recorded the rate of ongoing pain localized in the biceps groove that was severe enough to warrant revision surgery.30There was a statistically significant difference in the revision rate between the techniques that released the biceps sheath (6.8%,4/59) when compared to the techniques that did not release the biceps sheath (20.6%,14/68).In a recent case series,Savin et al.31treated,with a mini-open subpectoral technique,25 patients in whom a tenodesis or tenotomy had failed.In their case series,they found a high rate of patient satisfaction and significant improvement in functional outcomes.These data support our observations regarding reduced postoperative pain with mini-open LHB subpectoral tenodesis.Elements in the biceps groove generating residual pain may well cause failure of proximal tenodesis.Werner et al.32and Gombera et al.33compared the clinical outcomes of open subpectoral biceps tenodesis and arthroscopic suprapectoral biceps tenodesis.Patients undergoing an all-arthroscopic suprapectoral tenodesis or an open subpectoral tenodesis showed no significant differences in clinical outcomes between the 2 techniques at a minimum of 2 years postoperatively.No difference in perioperative pain was found between the arthroscopic and the mini-open technique in either of these studies.As in our population,the postoperative Visual Analog Score was similar for the 2 techniques.
Complications after subpectoral biceps tenodesis with interference screw fixation include failure of tenodesis,hematoma,seroma,infection,bioabsorbable screw reaction,persistent bicipital pain,neurovascular injury,and fracture.17,34In a case series study of 353 patients with 3-year follow-up,Nho et al.35reported an incidence of complications after subpectoral biceps tenodesis of 2.0%.Our patients did not report any postoperative complications,excluding a single case of delayed postoperative onset of Popeye deformity.
We are aware that a subpectoral LHB tenodesis is more technically demanding and requires a supplementary miniopen humeral access to be performed,but this technique should be considered so as to reduce postoperative pain.The heterogeneous nature of the type of RC tear that affected the patients included in our sample population is a potential weakness of our study.However,we aimed to make our population as homogeneous as possible by excluding patients with other medical comorbidities,by setting an age restriction,and by excluding patients with massive RC lesions.Also,no statistically significant differences were present at baseline.
The multiple concomitant surgical procedures performed in each of our patients could represent a potential confounding element.Therefore,as previously recommended by Kerschbaum et al.,36we evaluated patients with LHB pathologies using the LHB score because it provides LHB-related information and is a condition-specific and validated tool for assessing the clinical outcomes of surgery.
Another limitation of our study involves the small number of patients included and the relatively short follow-up time.In the past,we undertook intra-operative randomization to assign patients to one treatment or the other.23In the present study,however,we randomized patients before the procedure started.Because we carried out the arthroscopy and visualized and probed the LHB tendon inside the joint,we were able to intraoperatively assess which portion of the tendon was inflamed(i.e.,whether the portion close to the insertion or within the bicipital groove was inflamed).Given the possible differing locations of the lesions,we preferred,in this instance,to randomize patients pre-operatively so as to avoid possible biases linked to this particular aspect of the procedure.
The results of the present investigation are validated by its randomized prospective comparative design.Only a very few other prospective comparative studies have been published on this topic recently.Clearly,the outcomes of this series of single-surgeon RC repairs at one medical centre need to be confirmed by future prospective,multicentre research trials,with larger numbers of patients and longer follow-up periods.
5.Conclusion
Tenodesis is a reliable option for painful pathological abnormalities of the LHB.The choice between different LHB tenodesis techniques can significantly influence the overall results of the surgery.Both HAT and mini-open ST produced good functional results.However,open ST was associated with a significantly lower incidence of postoperative pain.These findings support the hypothesis that residual synovial tissue within the biceps groove might cause postoperative pain,leading to failure of proximal tenodesis methods and requiring a subsequent revision.
Authors’contributions
EF took care of the patients,supervised the smooth running of the study,and drafted the manuscript;EGdS,AP,MP,and LLV helped to run the study,to draft the manuscript,and to review the literature;NM supervised the work and the writing of the manuscript and advised on the technical aspects and the interpretation of the results;FF supervised the work and the interpretation of the results.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Supplementary materials
Supplementary materials associated with this article can be found in the online version at 10.1016/j.jshs.2020.08.004.
 Journal of Sport and Health Science2023年5期
Journal of Sport and Health Science2023年5期
- Journal of Sport and Health Science的其它文章
- Skeletal muscle atrophy,regeneration,and dysfunction in heart failure:Impact of exercise training
- Look into my eyes:What can eye-based measures tell us about the relationship between physical activity and cognitive performance?
- Ecological correlates of sport and exercise participation among Thai adolescents:A hierarchical examination of a cross-sectional population survey
- Risk factors for chronic ankle instability after first episode of lateral ankle sprain:A retrospective analysis of 362 cases
- Machine-learning-based head impact subtyping based on the spectral densities of the measurable head kinematics
- Exploring overweight and obesity beyond body mass index:A body composition analysis in people with and without patellofemoral pain
