Risk factors for chronic ankle instability after first episode of lateral ankle sprain:A retrospective analysis of 362 cases
Jieyuan Zhang,Kai Yang,Cheng Wang,Wenqi Gu,Xueqian Li,Shaoling Fu,Guoxun Song,Jiazheng Wang,Chenglin Wu,Hongyi Zhu,d,,Zhongmin Shi,
a National Center for Orthopaedics,Shanghai Sixth People’s Hospital,Shanghai 200233,China
b Department of Orthopedic Surgery,Shanghai Sixth People’s Hospital,Shanghai 200233,China
c Department of Radiology,Shanghai Sixth People’s Hospital,Shanghai 200233,China
d Institute of Clinical Research,National Center for Orthopaedics,Shanghai Sixth People’s Hospital,Shanghai 200233,China
Abstract Background: Chronic ankle instability (CAI) is a common sequela following an acute lateral ankle sprain (LAS).To treat an acute LAS more effectively and efficiently,it is important to identify patients at substantial risk for developing CAI.This study identifies magnetic resonance imaging (MRI) manifestations for predicting CAI development after a first episode of LAS and explores appropriate clinical indications for ordering MRI scans for these patients.Methods: All patients with a first-episode LAS who received plain radiograph and MRI scanning within the first 2 weeks after LAS from December 1,2017 to December 1,2019 were identified.Data were collected using the Cumberland Ankle Instability Tool at final follow-up.Demographic and other related clinical variables,including age,sex,body mass index,and treatment were also recorded.Univariable and multivariable analyses were performed successively to identify risk factors for CAI after first-episode LAS.Results:A total 131 out of 362 patients with a mean follow-up of 3.0§0.6 years(mean§SD;2.0-4.1 years)developed CAI after first-episode LAS.According to multivariable regression,development of CAI after first-episode LAS was associated with 5 prognostic factors: age (odds ratio(OR)=0.96,95%confidence interval(95%CI):0.93-1.00,p=0.032);body mass index(OR=1.09,95%CI:1.02-1.17,p=0.009);posterior talofibular ligament injury(OR=2.17,95%CI:1.05-4.48,p=0.035);large bone marrow lesion of the talus(OR=2.69,95%CI:1.30-5.58,p=0.008),and Grade 2 effusion of the tibiotalar joint(OR=2.61,95%CI:1.39-4.89,p=0.003).When patients had at least 1 positive clinical finding in the 10-m walk test,anterior drawer test,or inversion tilt test,they had a 90.2%sensitivity and 77.4%specificity in terms of detecting at least 1 prognostic factor by MRI.Conclusion:MRI scanning is valuable in predicting CAI after first-episode LAS for those patients with at least 1 positive clinical finding in the 10-m walk test,anterior drawer test,and inversion tilt test.Further prospective and large-scale studies are necessary for validation.
Keywords: Chronic ankle instability;Lateral ankle sprain;MRI;Risk factors
1.Introduction
Lateral ankle sprains (LAS) have been reported as one of the most common musculoskeletal injuries in young and active individuals.1The prevalence of LAS among the general population is also common,with more than 40%of the general population experiencing it during their lifetime.2-4The high prevalence of LAS injuries causes a high social economic burden in terms of initial management and rehabilitation,and it also reduces labor productivity.5,6Despite initial treatment(taping/bracing) and physical rehabilitation,LAS may progress to chronic ankle instability (CAI) in 30%-40% of patients,7which implies that some important prognostic factors associated with the efficacy of rehabilitation remain unknown.The CAI-associated sequelae,including pain,persistent swelling,ankle “giving-way” phenomenon,risk of recurrent injury,and impaired joint function,contribute greatly to the overall social and economic costs.7,8Hence,assessing and reducing the risk of CAI development is a key priority after acute LAS.9Additionally,patients with severe CAI generally require surgical intervention to avoid repeated ankle sprains,which may cause osteoarthritis in the long term.10Early surgical interventions could achieve better functional outcomes than later surgical repair,especially when both ligaments rupture and when there is ligament laxity after firstepisode LAS.11Currently,there is no well-established tool to assess whether patients will develop CAI immediately after an acute LAS.12It is also important to determine which patients can benefit from early surgical intervention.Multiple factors,including demographic features,13severity of LAS,14anatomic configuration of foot and ankle,15,16neuromuscular factors,17and initial treatment,18have been studied for their potential contribution to CAI development.The main purpose of this study was to identify risk factors associated with the development of CAI after first-episode LAS.
Classically,magnetic resonance imaging (MRI) scans are only recommended in cases where there is suspicion of highgrade ligament injuries,osteochondral defects,syndesmotic injuries,or occult fractures.19Although several studies have investigated ligamentous and bony injuries after acute LAS in athletes,20,21no previous studies have focused on the association between incidence of CAI and MRI characteristics after LAS,especially in the general population.As the difference between plain radiograph and MRI scanning in China is only USD 50,22many patients prefer to do plain radiograph and MRI scanning simultaneously following acute LAS injury.Our data can thus provide a unique insight into LAS and the pathogenesis of CAI.To address the existing knowledge gaps,we conducted a retrospective analysis and asked the following questions: (a) Is MRI scanning a valuable tool for predicting CAI development after first-episode LAS? and (b) What are the correct indications for ordering MRI scanning in patients with LAS?
2.Methods
2.1.Study design
This is a single-center,retrospective cohort study enrolling patients visiting the emergency department and reporting a first-episode ankle inversion injury in their lifetime.Participants received plain radiograph and MRI scanning of the injured ankle within 2 weeks of the injury.Data were collected using the Cumberland Ankle Instability Tool (CAIT) at the last follow-up to determine the development of CAI.Demographic and other related clinical variables,including age,sex,body mass index(BMI),and treatment,were all recorded.The study was designed and executed in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Shanghai Sixth People’s Hospital (ref No.2020-136).All participants provided written informed consent.
2.2.Participants
All patients who visited the Emergency Department or Outpatient Department for a first-episode LAS and received MRI scanning during the acute phase of injury (defined as within 2 weeks of initial injury)between December 1,2017 and December 1,2019 were screened for eligibility.Patients were excluded if:they were under 18 or over 40 years old(n=234);they did not complete at least a 2-year follow up(n=67);there were no available anteroposterior or lateral radiographs of the ankle (n=35);fractures,including avulsion fractures,were present (n=26);there were any scarred ligaments of the ankle defined as thinned or thickened ligaments without discontinuity or peri-ligamentous edema(n=4);there were any bone or softtissue tumors in the foot or ankle (n=3);there were previous ankle surgeries(n=4)or open trauma(n=5);or they refused to participate (n=32).We also excluded those patients who did not receive standard care(n=62),which was defined according to previously published consensus.19Briefly,rest,ice,compression,elevation was not recommended,and nonsteroidal antiinflammatory drugs were used to reduce pain and swelling.Functional support was recommended and the choice between tape and brace was based on patient preference.We advised patients to start exercise therapy as soon as could be tolerated after the initial LAS.Exercise therapy programs mainly consisted of neuromuscular and proprioceptive exercises.
2.3.Baseline characteristics
All demographic information,including age,sex,and BMI,was recorded.Delayed physical examination (4-7 days after initial LAS),which included the anterior drawer test for anterior talofibular ligament (ATFL) function and inversion tilt test for both ATFL and calcaneofibular ligament (CFL) function,was performed to assess the severity of the ligament damage.Ankle swelling was assessed using the figure-of-eight method.23Ankle joint arthrokinematics were assessed via the posterior talar glide test.24For patient-reported outcomes,we adopted CAIT,25a well-validated self-report instrument for assessing CAI.CAIT is a 9-item 30-point scale for measuring the severity of functional ankle instability.25,26
2.4.Radiographic assessment
A single independent researcher identified all patient information prior to MRI assessment.The following structures,including ligament and bone marrow,were assessed using previously reported definitions.20,21The ligaments under evaluation in this study were the ATFL,CFL,posterior talofibular ligament(PTFL),medial collateral ligament complex,syndesmotic ligaments,interosseous membrane,the spring ligament complex,and the sinus tarsi ligaments.ATFL and CFL injuries were common,and they were graded as normal(Grade 0),lowgrade sprain (Grade 1=peri-ligamentous edema only and no discontinuity of fibers),partial disruption (Grade 2=partial discontinuity with preserved remnant fibers),and complete disruption (Grade 3=complete discontinuity).27,28Injuries to other ligamentous structures were relatively rare and thus graded as 0=normal or 1=present.Acute bone marrow lesions(BMLs)were defined as adjacent edema to subchondral plate with or without cartilage surface damage.BMLs in the tibia,fibula,calcaneus,and navicular bone were simplified and graded 0=normal,1=present.BMLs of the talus were assessed mainly as an ordinal variable,according to a previously published classification:290=normal,1=small subchondral edema only,and 2=large subchondral edema only.Small subchondral edema of the talus was defined as being restricted to only 1 part of the talus (the body,neck,or head).Large subchondral edema of the talus was defined as that involving 2 or 3 parts of the talus.Simple bone contusion was defined as edema without involving subchondral areas.Finally,the effusion of the tibiotalar and talocalcaneal joints were graded separately: Grade 0=minimal physiological amounts of intra-articular fluid (normal);Grade 1=effusion with less than 50% of maximum capsular distension;and Grade 2=effusion with -50% of maximum capsular distension.21All final outcomes were the mean or majority of 3 readouts from 3 respective evaluators.
2.5.Definition of CAI and patient-reported outcomes
Because the definitive diagnosis of CAI remains controversial,30,31we used a widely accepted definition of CAI in this study.The diagnosis of CAI was defined in the current study as(a)CAIT<24;(b)CAIT -24 with the perception of ankle “giving-way”;and (c) CAIT <26 with a history of recurrent ankle sprain and at least 1 persistent symptom(pain,swelling,and weakness) at the 24-month follow-up.7,12,30-33The final outcome of CAI diagnosis was determined by majority consensus among 3 independent evaluators.A “coper” is defined as an individual who is more than 12 months removed from the index ankle sprain,has incurred no recurrent ankle sprains,reports no or very minimal symptoms or deficits in self-reported function,and perceives a full recovery.
2.6.Statistical analysis
All statistical analyses were performed in 2-sided fashion and at the 0.05 level of significance.All statistical analysis was conducted using SPSS Version 26.0 (IBM,Armonk,NY,USA) with any necessary extensions.Continuous variables were represented as mean§SD,and ordinal/categorical variables were presented as number (%).For each categorical/ordinal variable,statistical significance was assessed using a Pearson x2test or Fisher exact test (if the expected count was<5 for any contingency cell).For each continuous variable,the statistical significance was assessed using Mann-WhitneyUtest.A receiver operating characteristic analysis was used to determine the cut-off for converting continuous variables into categorical ones when the area under the curve was >0.5.When the yieldedpvalue was less than 0.2 in univariable analysis,the variable was further included in the logistic regression for multivariable analysis.For a prognostic model,at least 20 incident events per variable are needed to optimize reliability and to avoid bias in regression coefficients.34,35
3.Results
A total of 362 patients were included for final analysis in this study.The mean age was 27.5 § 6.5 years old (mean §SD),and 40.3% were female (n=146).The mean time from injury to MRI scanning was 3.1§3.9 days.The mean followup was 3.0§0.6 years(2.0-4.1 years).
3.1.Univariable and multivariable analysis on the incidence of CAI
The number of patients who had incidence of CAI after first-episode LAS was 131 (36.2%).The univariable analysis of demographic and clinical characteristics is summarized in Table 1.According to the pre-defined criteria on statistical analysis,age,BMI,CFL injury,PTFL injury,effusion of the tibiotalar joint,and BML of the talus yieldedp<0.2;thus,these variables were included in the multivariable analysis(Table 1).In the multivariable analysis(Table 2),incident CAI was associated with age (odds ratio (OR)=0.96,95% confidence interval (95%CI): 0.93-1.00,p=0.032);BMI(OR=1.09,95%CI: 1.02-1.17,p=0.009);PTFL injury(OR=2.17,95%CI: 1.05-4.48,p=0.035);large BML of the talus (OR=2.69,95%CI: 1.30-5.58,p=0.008),and Grade 2 effusion of the tibiotalar joint(OR=2.61,95%CI:1.39-4.89,p=0.003).
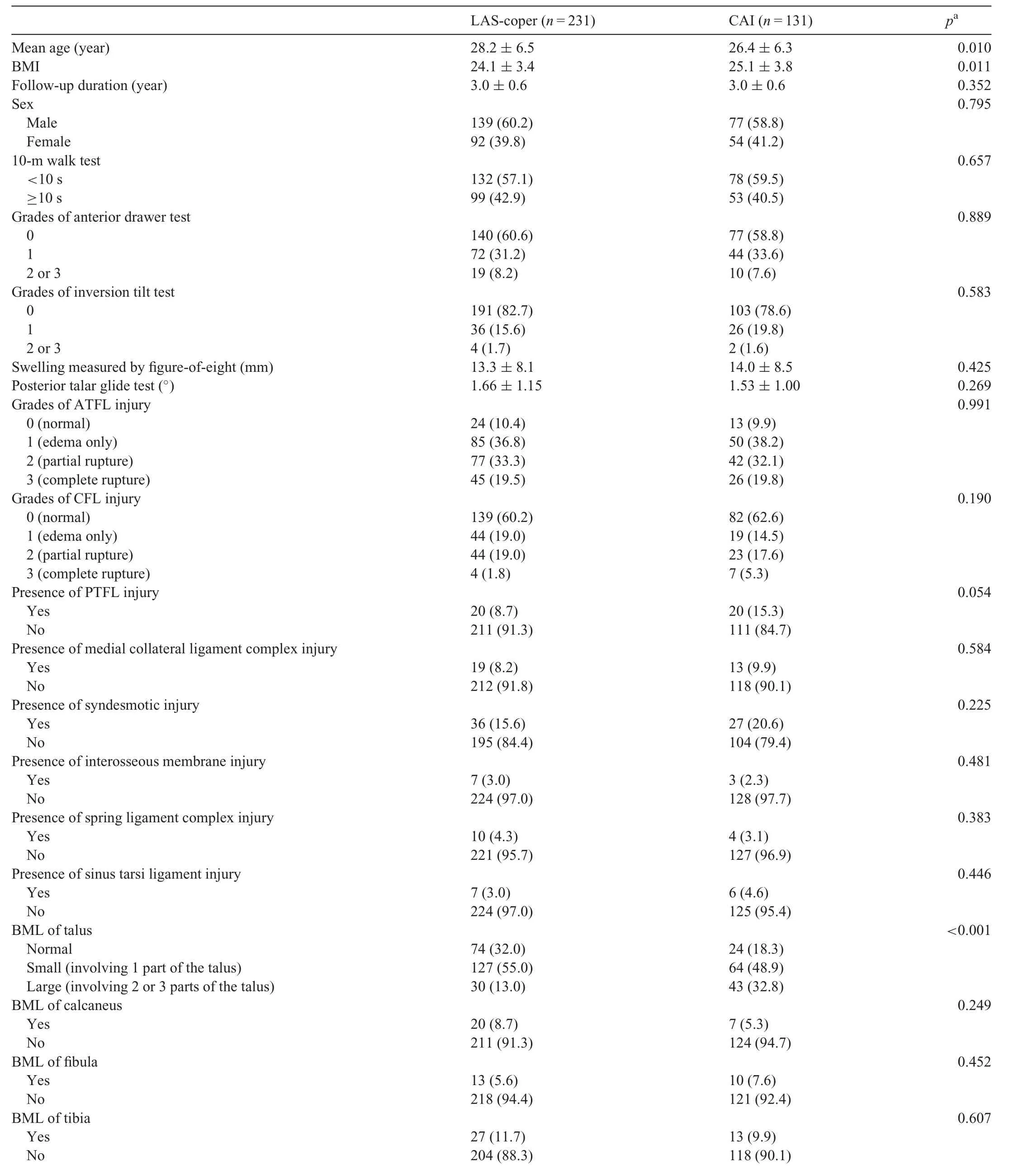
Table 1Univariable comparison of baseline demographic and clinical characteristics of CAI and LAS-coper cohorts.
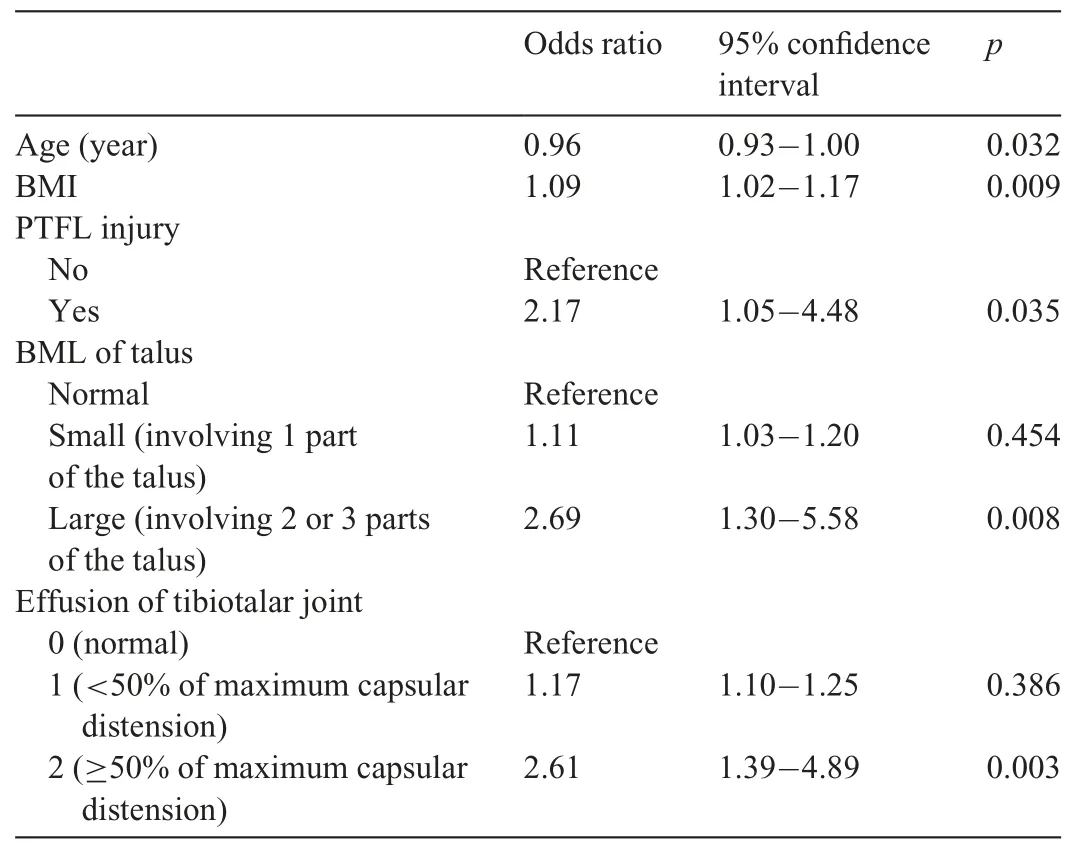
Table 2Multivariable logistic regression analysis.
3.2.Exploring the appropriate indications for ordering MRI after acute LAS
Clearly,it is impossible and inappropriate to order MRI scanning for every patient who sustains LAS.This reality prompted us to investigate the appropriate indications for ordering MRI after acute LAS.Here,we defined PTFL injury,large BML of the talus,and Grade 2 effusion of the tibiotalar joint on MRI scans as positive findings.In this study,163 out of 362 patients(45.0%)had at least 1 positive finding.We also explored the relationships between clinical tests and “at least 1 positive finding”.When patients had at least 1 positive finding in the 10-m walk test,anterior drawer test,or inversion tilt test,there was a 90.2% sensitivity and 77.4% specificity in terms of detecting at least 1 prognostic factor(Table 3).
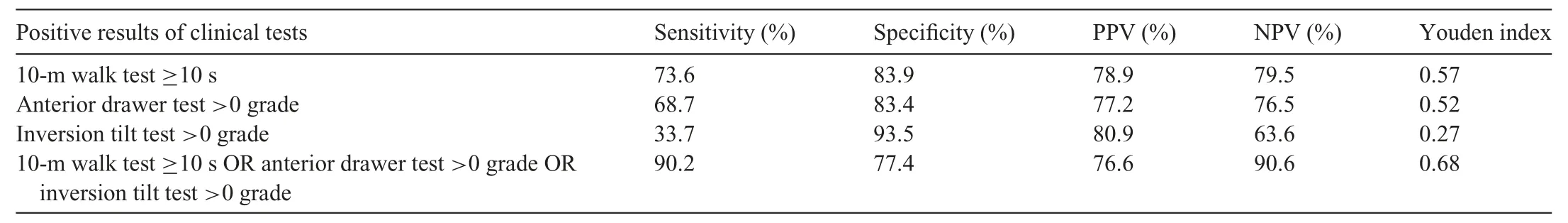
Table 3Findings from clinical tests for predicting positive findings on MRI.
4.Discussion
The long-term consequences of CAI,including chronic osteochondral lesion and osteoarthritis,may cause severe morbidities for patients.Despite standard care consisting of taping/bracing and physical rehabilitation,LAS could eventually progress to CAI in 30%-40% patients.7,19This fact suggests that many important factors contributing to the pathogenesis of CAI after LAS remain unknown.The current study is the largest study to date to investigate the association between MRI manifestations during the acute phase of LAS and CAI outcomes.We demonstrated that MRI scanning was valuable for those patients who presented at least 1 positive finding in the 10-m walk test,anterior drawer test,or inversion tilt test.Development of CAI after first-episode LAS was associated with 5 prognostic factors: age,BMI,PTFL injury,and Grade 2 effusion of the tibiotalar joint.It has been previously reported that BMI and age were associated with CAI outcomes after LAS.13,18Our study further verified these observations,finding that young age and increased BMI could contribute to the development of CAI after first-episode LAS.
To date,many studies have observed an association between deficiency in ankle joint proprioception (which commonly refers to position,stress,and vibration sensations)and CAI.17It is widely believed that the impaired proprioceptive nerve within the sprained ligaments contributes significantly to repeated ankle ligamentous injuries and subsequent development of CAI.36In support of this notion,previous studies have demonstrated that proprioception-targeted ankle rehabilitation strategies were effective in treating CAI.37,38As of now,it remains unclear which patients will see the proper function of proprioceptive nerves restored within the sprained ligaments after LAS.Previous studies have reported that the development of CAI has no correlation with the severity of ATFL/CFL injuries as assessed by clinical tests after LAS.39Thus,the initial severity of injury to proprioceptive nerves within the sprained ligaments might not be a determinant for ankle proprioception deficiency in CAI.
Our study further verified this observation that the severity of ATFL/CFL injuries was not directly relevant to CAI development after LAS.Interestingly,we found that PTFL injury was more closely related to CAI sequelae.It has been well established that PTFL contributes little to the overall stability of the ankle and that repair of ATFL alone is sufficient to restore the stability of unstable ankles.40-42Thus,it was highly possible that PTFL injury ranked as a prognostic factor due to the fact that PTFL injury is a sensitive sign for severe ligamentous injuries.Further investigation is needed to confirm this finding and determine underlying mechanisms.
Strikingly,we observed that CAI development after LAS was significantly associated with large BML of the talus and Grade 2 effusion of the tibiotalar joint.BMLs are a common sign of inflammation in bone,which could be observed in patients with a number of diseases,including osteoarthritis,43bone malignancy,44and osteochondral lesions.45Likewise,effusion of the joint is another important manifestation of synovitis and joint inflammation.46,47Many preclinical and clinical investigations have revealed that an inflammatory environment could delay the repair of peripheral nerves after acute injury.48,49Thus,it is reasonable to predict that severe ankle inflammation might hinder the repair of proprioceptive nerves in sprained ligaments and,subsequently,contribute to the development of CAI.
Clinical examinations,including the anterior drawer test,inversion tilt test,figure-of-eight test,and posterior talar glide test,have limited predictive value for CAI when performed in the acute phase of a first-episode LAS.50,51This study once again demonstrated that clinical examinations were insufficient to predict CAI outcome after acute LAS.Nevertheless,we found clinical examinations to be valuable for determining whether an MRI scan should be performed in the acute phase of LAS.Based on our findings,the 10-m walk test,anterior drawer test,and inversion tilt test should be performed.When any patient had at least 1 positive finding among these 3 tests,MRI scanning was recommended.
The current study also had several limitations.First,multiple future prospective studies are still needed to validate our findings.Because of its retrospective nature,any therapies attempted by patients before they underwent treatment by a physician were unknown in this study.Second,the inevitable selection bias should be considered.According to positive Ottawa Ankle Rules,40the standard of care suggests that only plain radiograph should be considered in very small proportion of LAS patients.However,physicians in our institution hardly followed the Ottawa Ankle Rules and ordered plain radiographs for most patients with acute LAS,mainly because of the low cost of plains radiographs.As a result,we only excluded 35 cases due to non-availability of anteroposterior or lateral radiographs of the ankle.Many patients preferred to undergo MRI scanning during the acute phase after LAS because it only costs USD 60,which is more or less affordable for patients in China.22Thus,“severe” ankle sprains were more likely to be included since the intensity of symptoms would drive patients to request MRI scanning.Finally,because there is no consensus regarding the diagnostic criteria for CAI,we adopted criteria from recent high-quality publications.Extrapolation of our conclusions to real clinical practice should be done with caution,and future prospective studies are needed.
5.Conclusion
MRI scanning proved valuable in predicting CAI after firstepisode LAS with respect to 5 prognostic factors: age,BMI,PTFL injury,large BML of the talus,and Grade 2 effusion of the tibiotalar joint.For those patients with at least 1 positive finding in the 10-m walk test,anterior drawer test,or inversion tilt test,MRI scanning was recommended.Future prospective and large-scale studies are needed for further validation.
Acknowledgments
This work was supported by the Biomedicine Supporting Program of Shanghai “Science and Technology Innovation Plan” (19441902400);the Ningxia Hui Autonomous Region Key R&D program (2020BCH01001);the Shanghai “Science and Technology Innovation Action Plan” Domestic Science and Technology Cooperation Project (20025800200);and the Clinical Research Program of Shanghai Municipal Health Commission(201940367).
Authors’contributions
JZ and KY carried out the study design,data analysis and interpretation,and drafted the manuscript;CW,WG,XL,SF,GS,JW,and ClW carried out data collation and follow-up examination;ZS and HZ conceived the study,participated in its design and data interpretation,and helped to draft the manuscript.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
 Journal of Sport and Health Science2023年5期
Journal of Sport and Health Science2023年5期
- Journal of Sport and Health Science的其它文章
- Skeletal muscle atrophy,regeneration,and dysfunction in heart failure:Impact of exercise training
- Look into my eyes:What can eye-based measures tell us about the relationship between physical activity and cognitive performance?
- Ecological correlates of sport and exercise participation among Thai adolescents:A hierarchical examination of a cross-sectional population survey
- The management of the long head of the biceps in rotator cuff repair:A comparative study of high vs.subpectoral tenodesis
- Machine-learning-based head impact subtyping based on the spectral densities of the measurable head kinematics
- Exploring overweight and obesity beyond body mass index:A body composition analysis in people with and without patellofemoral pain
