Progressive eschar-like wound and peripheral neurological dysfunction with severe inf lammatory status: infection or unnatural immune response?
Hanghui Cen ,Pengqin Xu ,Hong Zou ,Jialiang Wang ,Xingang Wang ,Chunmao Han
1 Department of Burns &Wound Care Center, the Second Affiliated Hospital of Zhejiang University School of Medicine,Hangzhou 310009, China
2 Department of Pathology, the Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310009, China
The immune system plays an essential role in maintaining health,protecting humans from pathogens and preventing the majority of tumors.Immunocompromised individuals are more likely to encounter infectious and neoplastic diseases.Excessive immune responses,which are also involved in the pathogenesis of many diseases,have drawn increasing attention in recent years.[1]Blood and nervous system manifestations have been reported to be related to some specific viruses,and potential associations of these viruses with autoimmune diseases have come into the spotlight.Certain infections might arouse immune overreaction in susceptible individuals or even cytokine storms that are harmful to organs and tissues.
CASE
A 53-year-old male patient came to our emergency department with high fever and an eschar-like wound on the right chest,who had been recently hospitalized due to paralysis of the right upper limb. The diagnosis was tentatively considered necrotizing soft tissue infection(NSTI) and peripheral neuropathy.The lesion initially appeared as a fingernail-sized phyma,which became blistered and ulcerated. The application of external liniments (Woodlock Medicated Balm [in Chinese:Huoluo You]) had little effect,and the skin lesion rapidly spread out and darkened like an eschar.On admission,the physical examination indicated aggravated muscle weakness,including a significant asymmetrical decrease in the strength of the bilateral upper limbs (2/5) and aref lexia of the right lower extremity.The results of the electromyography (EMG) of bilateral upper limbs were summarized as multiple motor and sensory peripheral neuropathy,predominantly axonopathy and secondary sensory demyelination,with a sural-sparing pattern(supplementary Tables 1-3).This man was in good fitness despite a history of heavy smoking (approximately 40 packyears).He denied any noticeable bite,suspicious animal contact or radioactive exposure.Since admission,the patient suffered persistent fever and prominently elevated inflammatory markers (supplementary Figure 1).Clinical immunology tests showed that the humoral immune response dominated,as presented in supplementary Tables 4-5.He also had mild hepatic and renal insufficiency,with a reduced albumin/globulin ratio (0.74) but no hepatitis virus infection(supplementary Tables 6-8).The wound presented as anthraconecrosis without suppuration and f luctuation,which had been expanding rapidly (Figure 1).Cutaneous anthrax and scrub typhus (Orientia tsutsugamushi) were ruled out by pathogenic and serological tests.Fortunately,his vit al signs remained stable,and his condition did not progress into septic shock.
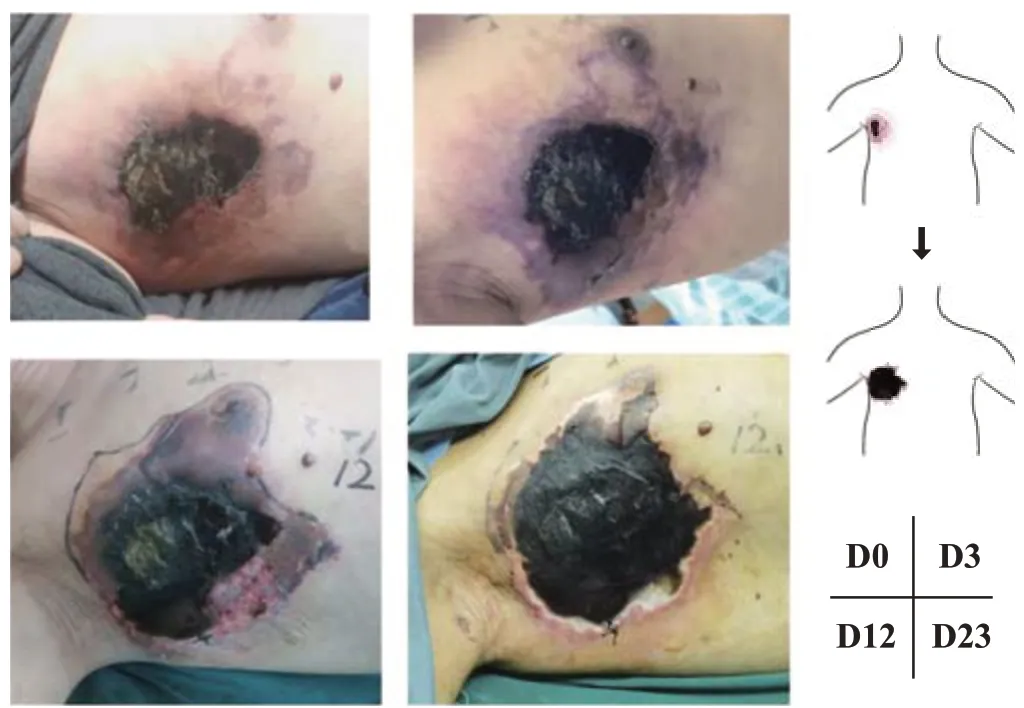
Figure 1.The eschar-like wound was in the right upper chest,close to the axilla,and the wound extended swiftly with v iolet a reola.
His symptoms appeared to respond well to empirical antibiotics and short-term use of low-dose immunoglobulin.However,the white blood cell (WBC)count continued to drop when we received critical values(WBC count at 1.5×109/L,neutrophil count at 0.13×109/L).Infection-induced myelosuppression was the primary consideration.We made an emergency excision and extended debridement of the chest lesion,covering the remaining wound with silver ion and vaseline dressing.Postoperative pathological analyses are depicted in supplementary Figure 2.Pathology experts acknowledged that there was insufficient evidence for tumor-related diseases.
The patient had an elevated level of prostate-specific antigen (PSA) at 10.9 (normally <4) ng/mL,but he had no abnormal prostatic imaging results.Positron emission tomography (PET)/computed tomography (CT) showed right chest infection and inflammatory hyperplasia of the lymph nodes.Autoimmune antibody tests only found mild abnormality of anti-proteinase 3 (PR3) IgG at 29.2(normally <20.0) AU/mL,which lacked evidence for most rheumatoid diseases (supplementary Tables 9-13).Metagenomics next-generation sequencing (mNGS) and cultures of separate sources for several times showed nothing specific.
This patient underwent a secondary mild debridement and vacuum sealing drainage one week later,while the scheduled skin graft was delayed due to the unsatisfactory base.Around the perioperative period,he underwent diagnostic bone marrow aspiration and bilateral thoracocentesis and drainage for pleural effusion.Bone marrow examination d emonstrated diminished hematopoiesis,widespread macrophages and infrequent h emophagocytosis.After that,his condition worsened before it momentarily stabilized.The patient experienced acute heart failure and respiratory failure and was transferred to the intensive care unit (ICU).He also suffered successive symptoms of hematochezia and hemoptysis.Contrast-enhanced CT did not reveal any bleeding point but found tiny splenic infarction and mesenteric artery microthrombosis.Before things got better,multiple intestinal obstructions tormented the man.Inflammatory indicators were severely elevated,especially interleukin-6 (IL-6) (788 pg/mL) and procalcitonin (PCT,>100 ng/mL).The patient was given methylprednisolone (40 mg,Q12h) for approximately one week with infections under control,and the dose was then reduced by half.However,the patient’s co ndition deteriorated,and eventually,he did not recover from a massive gastrointestinal hemorrhage episode.
DISCUSSION
A progressive eschar-like wound with excessively high inf lammation and inchoate neurological impairment were major characteristics of this patient.Congenital malformation or traumatic injury were beyond consideration.There was neither evidence of acute poisoning nor c orrosion.T he presence of a systemic inflammatory state was confirmed,as PET/CT found hyperplasia of numerous lymph nodes throughout the body.T he chances of hematological malignancy seemed particularly slim,according to the bone marrow examinations,and there was no evidence of histiocytic disorders judging from the pathology results.[2,3]Unlike acute trauma or external infection,the chest wound necrotic processes seemed to develop from the deep tissues.A pathogenetic hypothesis might be described as follows.If there was a stimulus of an unknown origin,we would be i nclined to consider a single etiologic infection that triggered an exaggerated inflammatory response.The nervous system was first assaulted,and the endothelium was injured,which led to minor vasculitis and microvessel thrombosis.
After any invasive procedure,the patient always experienced activation of systemic inflammation,which could not be entirely attributable to common clinical infections.Macrophage activation syndrome(MAS),also identified as secondary hemophagocytic lymphohistiocytosis (sHLH),drew our attention because of the hemophagocytosis phenomenon in pathological examinations.MAS refers to an overwhelming inflammation status,mostly associated with rheumatic diseases,namely,systemic juvenile inflammatory arthritis (sJIA).[4-6]Certain viral infections,such as i nfections with Epstein-Barr virus (EBV) and c ytomegalovirus (CMV),complicated with MAS are occasionally reported.Since COVID-19,much more attention has been given to cytokine storm syndrome(CSS),a tough and lethal issue that viruses might cause.Various hyperinflammatory states associated with multiorgan system failure can be grouped under the branch of CSS as previously stated.[7,8]The patient had positive CMV IgG test results,which were considered to be due to previous infection.The recognition of MAS in this case was imprecise for atypical features and inadequate H score,[9-11]whereas an excessive immune response seemed more appropriate.
Relationships between the mechanisms of coagulation and inflammation have been shown.[12]T he progression of disease in this case depicted hazy distinctions among operative stress reaction,coagulation and inflammation.Systemic hyperinflammation and injury to the vascular endothelium also initiated coagulation reactions.Microvascular thrombosis might occur as a result of synergistic activation of coagulation and inf lammation.[12]
It is difficult to determine whether earlier interventions on chest wounds are beneficial in retarding progression.The stress of inf lammation,to some extent,comes from the exposed wounds.As wound repair and reconstructive surgeons,we emphasize the importance of avoiding wound deepening and sealing the wound at an early stage.[13,14]The lesions showed a bottom-up trend,and thus,the effect of skin grafting or f lap transplantation was unassured.Despite advice from consultants regarding the use of anti-inflammatory corticosteroids and immunosuppressants,the administration of these medications still lacks support from the guidelines and recommendations.
CONCLUSIONS
Immune-related health problems have become greater threats,and concerns have arisen.Herein,we present the development of this patient’s disease and train of corresponding thoughts of our medical team,q uesting for broader attention and inspiration to similar situations.
Funding:The study was supported by Zhejiang Basic Public Welfare Research Program (LGF20H190004).
Ethical approval:The study was approved by the Ethical Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine.
Conf licts of interest:The authors have no conf licts of interest.
Contributors:HHC proposed the case and wrote the first draft.All authors contributed to the design and interpretation of the study and to further drafts.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World journal of emergency medicine2023年5期
World journal of emergency medicine2023年5期
- World journal of emergency medicine的其它文章
- Emergency department approach to monkeypox
- The neuro-prognostic value of the ion shift index in cardiac arrest patients following extracorporeal cardiopulmonary resuscitation
- A prospective cohort study on serum A20 as a prognostic biomarker of aneurysmal subarachnoid hemorrhage
- Mendelian randomization study to investigate the causal relationship between plasma homocysteine and chronic obstructive pulmonary disease
- Cardiopulmonary prognosis of prophylactic endotracheal intubation in patients with upper gastrointestinal bleeding undergoing endoscopy
- Effects of mesencephalic astrocyte-derived neurotrophic factor on sepsis-associated acute kidney injury
