Emergency department approach to monkeypox
Catherine V.Levitt ,Quincy K.Tran ,Hashem Hraky ,Maryann Mazer-Amirshahi ,Ali Pourmand
1 Department of Emergency Medicine, George Washington University School of Medicine and Health Sciences, Washington DC 20037, USA
2 Department of Emergency Medicine, University of Maryland School of Medicine, Baltimore 21201, USA
3 Program in Trauma, The R Adams Cowley Shock Trauma Center, University of Maryland School of Medicine, Baltimore 21201, USA
4 Department of Emergency Medicine, MedStar Washington Hospital Center and Georgetown University School of Medicine, Washington DC 20037, USA
BACKGROUND: Monkeypox (mpox) is a viral infection that is primarily endemic to countries in Africa,but large outbreaks outside of Africa have been historically rare.In June 2022,mpox began to spread across Europe and North America,causing the World Health Organization (WHO) to declare mpox a public health emergency of international concern.This article aims to review clinical presentation,diagnosis,and prevention and treatment strategies on mpox,providing the basic knowledge for prevention and control for emergency providers.METHODS: We conducted a review of the literature using PubMed and SCOPUS databases from their beginnings to the end of July 2023.The inclusion criteria were studies on adult patients focusing on emerging infections that described an approach to a public health emergency of international concern,systematic reviews,clinical guidelines,and retrospective studies.Studies that were not published in English were excluded.RESULTS: We included 50 studies in this review.The initial symptoms of mpox are non-specific:fever,malaise,myalgias,and sore throat.Rash,a common presentation of mpox,usually occurs 2-4 weeks after the prodrome,but the presence of lymphadenopathy may distinguish mpox from other infections from the Poxviridae family.Life-threatening complications such as pneumonia,sepsis,encephalitis,myocarditis,and death can occur.There are documented co-occurrences of human immunodeficiency virus (HIV) and other sexually transmitted infections that can worsen morbidity.CONCLUSION: The initial presentation of mpox is non-specific.The preferred treatment included tecovirimat in patients with severe illness or at high risk of developing severe disease and vaccination with two doses of JYNNEOS.However,careful history and physical examination can raise the clinicians’ suspicion and point toward a prompt diagnosis.There are different modalities to prevent and treat mpox infection.
KEYWORDS: Monkeypox;Emergency medicine;Human immunodeficiency virus;Infection
INTRODUCTION
Monkeypox (mpox) is a zoonotic disease first identif ied in monkeys in Denmark in 1958.It is a viral infection caused by a double-stranded DNAOrthopoxvirus,[1]which is part of thePoxviridaefamily.[2]The first human case of mpox was reported in the Democratic Republic of Congo in 1970,[2]but large outbreaks outside of Africa have been historically rare.In May 2022,clusters of mpox cases were identified in the United Kingdom,which were ultimately traced back to an individual who had previously visited Nigeria.[3]Additional cases were reported as the disease was disseminated throughout Europe and the Americas.In late July 2022,the World Health Organization (WHO) declared mpox a public health emergency of international concern (PHEIC).[2]As of November 2022,the WHO began to use the term “mpox”in place of monkeypox.[4]By that time,the USA had 28,999 cases of conf irmed mpox,the highest of any country among all WHO members or states.[5]Current data,as of July 21,2023,show that the number of cases in the USA stands at 59,638.[6]Meanwhile,there are 89,687 cases and 152 deaths to date across 113 WHO member states.[6]
In non-endemic areas such Europe and the Americas during the most recent outbreak,mpox primarily affected those who identify as bisexual,gay,or men who have sex with men (MSM) and those aged between 18-44 years.However,this is not the case in areas in Africa where mpox is endemic.[6]In these endemic areas,there are a growing number of reported cases in women and children.[7]In addition,there are two different types,or clades,of mpox: the West African clade and the Central African (Congo Basin)clade,which is more infective and virulent.[8]Mortality rates are estimated to be less than 1% in cases involving the West African clade,but may exceed 10% in cases infected by the Central African clade.
This article aims to review clinical presentation,diagnosis,and prevention and treatment strategies on mpox,providing the basic knowledge for prevention and control for emergency providers.
METHODS
The PubMed and SCOPUS databases were searched from their beginnings to the end of July 2023.The references of the included studies were also examined to identify additional sources.The initial search identif ied 387 articles,of which 50 were included in this narrative review.Additional references were added at the author’s discretion.The inclusion criteria were studies on adult patients focusing on emerging infections that described an approach to a PHEIC,systematic reviews,clinical guidelines,and retrospective studies.Studies that were not published in English were excluded.
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
RESULTS
General clinical presentation
The typical mpox presentation in humans starts with a febrile prodrome,with 2-3 d of vague symptoms,and develops into a monomorphic rash,often umbilicated with pustules (Table 1).Skin lesions can involve the face and the palms and soles of hands and feet.[5,9]Temperatures peak during the second day of illness and usually range from 38.5 to 40.5 ℃ with additional prodromal symptoms of extreme weakness,fatigue and back ache.[5,9]
The prevalence of symptoms,as reported by patients who were diagnosed with mpox,are rash (97%),fever(85%),chills (71%),adenopathy (71%),headache (65%),and myalgias (56%).[5,9]The non-specific systemic features during the prodromal phase are present approximately 3 d before the eruption of the skin rash.[9-11]Regional lymph node enlargement may help differentiate human mpox from smallpox and chickenpox and other orthopoxviruses.[5]Genital skin lesions are a dominant symptom,with up to 95% of patients reporting a genital rash.[9,11]Approximately 68% of patients had a monomorphic rash,whereas 29% exhibited a pleomorphic rash.Monomorphic pustules or crusting lesions seen at the same time on a patient are more suggestive of mpox,and can also help differentiate it from smallpox,in which these lesions are usually not seen together.[9,12,13]In male patients,genital lesions affect the penis,scrotum and pubis.[9,12,13]Rashes of the genitals are occasionally accompanied by surrounding edema,leading to paraphimosis(severe swelling of the penile glans or foreskin).[9,12,13]
In the perianal region,lesions can involve the buttocks,anal margin,or anorectal mucosa,and lead to rectal pain,pain on defecation,tenesmus,serosanguineous discharge,or bleeding.[9,12,13]Fifteen percent of patients had only anal or rectal pain (or both).[14]A total of 14%-36% of patients presented with anorectal pain,tenesmus,constipation,purulent discharge or bleeding.If rectal perforation is suspected (intense pain or signs of sepsis),it is preferable to perform an magnetic resonance imaging (MRI).[15]
The typical eruption of the rash progresses from macules to papules (days 1-2),papules to vesicles (days 3-4),vesicles to pustules (days 5-6),pustules to umbilicated lesions (day 7),and finally to a crusted lesion (days 8-14) (Table 1).Lesions are generally 2-5 mm in diameter,although some have been documented as reaching 1 cm.[9,11,12,15,16]Once in the desquamation phase,the patients can be considered noninfectious.[9,15]
As mentioned before,the most common site is theanogenital area,followed by the trunk and limbs (65%) and face (25%).[9,11,15,17]Lesions of the oral mucosa are described as ulcerative or crusted,whereas lesions on the tongue are usually circular,white,and umbilicated.Tonsillar lesions are noted to be painful and can cause difficulty with swallowing.[9,12,13]Between 10% and 21% of patients present with odynophagia and dysphagia associated with non-specific ulcerative plaques on the palatine tonsils or pharynx and generally with associated painful cervical adenopathy.[15]Studies focusing on otolaryngology manifestations found that in some patients with odynophagia,the pathognomonic rash of mpox had not yet developed,suggesting that mucosal lesions and oropharyngeal symptoms can develop prior to other systemic symptoms of mpox infection.[17,18]
Most symptoms of ocular involvement include pain,redness,watering,photophobia,discharge,swelling around the eyes,and diminished vision.In unvaccinated patients,ophthalmic manifestations of mpox include periorbital vesicular rash (25%),conjunctivitis (30%),ulcerative keratitis (4%-8%),and blepharitis (30%).[11,19,20]Most visual complications occur more commonly in unvaccinated(74%) than in vaccinated (39.5%) individuals.[11,19,20]Corneal involvement is the most severe complication of ocular mpox,as it can result in permanent vision loss and corneal scarring.[11,19,20]Conjunctivitis due to mpox infection may manifest as conjunctival ulcers,blistering or papular conjunctival lesions,and patients with mpox and conjunctivitis report more frequent systemic symptoms.Immunocompromised patients,such as children,tend to be more susceptible to conjunctivitis.
Novel symptomology,such as solitary lesions,penile edema resulting in both paraphimosis and phimosis,oropharyngeal lesions,secondary bacterial infections with purulent penile discharge,rectal perforation,and abscesses,may further differentiate mpox from other orthopoxviruses or rashes.[21]Severe complications of mpox include encephalitis,septicemia,bronchopneumonia,and ocular lesions resulting in corneal scarring and permanent vision loss.[18]Among those vaccinated,the most reported signs and symptoms were rash (96.5%),pruritis (33.5%),and enlarged lymph nodes (31.6%).Among unvaccinated persons,they were rash (97.3%),fever (46.5%),and malaise (43.0%).[22]
Diagnosis
History taking should include recent travel,exposure to individuals with conf irmed or suspected mpox infection,the onset of symptoms,sexual history,and history of smallpox vaccination.Full skin examination,with the stage of rashes noted and inspection of the oral mucosa,should be performed.Thorough ocular,pulmonary,and neurological examinations can help clinicians to assess severe disease manifestations.[23]
Definitive diagnosis of mpox is conducted with polymerase chain reaction (PCR) testing on fluid isolated from skin lesions or with electron microscopy and immunohistochemistry on biopsy samples.Serum IgG or IgM can detect past/present infection.[5]Laboratory specimens can be lesion surface swabs and/or exudate,collected from more than one lesion,or lesion crusts.[9]In one study,among the 1,754 confirmed mpox patients,skin samples were taken from 1,698,and 1,616 patients had mpox viral positivity in the skin samples.[1]As a result,this metaanalysis reported that the pooled prevalence was 98.77%(95% conf idence interval [95%CI] 94.74%-99.72%) using a random-effects model.
Viral load is an important indicator of the severity of infection,and higher viral loads of mpox are associated with more severe disease.[10]The value of the cycle threshold (Ct)has been used as a representative for viral loads and infectivity among patients.The Ct is defined as the PCR Ct that is necessary to multiply the viral genetic material to a detectable limit.The pooled mean value of Ct for mpox viral DNA in mpox-positive samples was 21.71 (95%CI20.68-22.75),and this value did not vary with age,sex distribution or sample size.[10,24]The majority of mpox DNA is collected from lesions in the genital area;however,33% is found in extragenital areas,including the abdomen,mouth,face,rectum,thorax,back,and extremities.[24]Mpox viral DNA has been detected in seminal fluid,rectal swab specimens,respiratory secretions,and the blood of patients tested.[25]The immunocompetent patients’viral DNA load would be detectable by quantitative PCR for a median time of 25 d from samples in the skin,16 d in the pharynx,16 d in the rectum,13 d in semen,and 1 d for blood samples.[13]Mpox virus DNA can be detected in approximately 60%-70% of anus and throat samples,50% of semen samples,and 20% of blood and urine samples.Direct swab of a skin lesion has a viral load higher by about two orders of magnitude compared with that in other body locations with Ct values approximately 22 vs.28.[12]
One report found mpox DNA in a patient’s eyelid and conjunctival swabs using standardized PCR testing.[20]Another case report focused on 5 immunocompetent young adult males who required hospitalization for neurologic symptoms found cerebrospinal fluid (CSF) lymphocytic pleocytosis and elevated CSF protein but negative CSF mpox PCR and/or serology.On brain MRI,there were subcortical,deep gray matter,cerebellum,and/or brainstem lesions.[26]While DNA was not isolated from CSF,lumbar puncture and MRI testing can help diagnose mpox in patients with neurologic symptoms.
Treatment
Currently,there are five drugs considered for the treatment of mpox: tecovirimat,brincidofovir (BCV),cidofovir (CDV),trif luridine,and intravenous (IV) vaccinia immune globulin (VIG) (Table 2).[27]In one study comparing usages of topical CDV 1%,patients who received the topical treatment saw resolution of their lesions within a median of 12 d.Only 10% of patients who used topical CDV 1% for 2 weeks had PCR-positive skin lesions,compared to 62.5%of patients who did not use CDV 1%.[9]
The only current Food and Drug Administration(FDA)-approved drug for the treatment of smallpox is tecovirimat.[5,9]Tecovirimat is the preferred agent for mpox treatment and is recommended in patients with severe illness,such as infection of the eye/cornea,encephalitis,severe proctitis,or pharyngitis.Patients at risk of developing severe illness (immunocompromised patients,children younger than 8 years,pregnant and nursing mothers) are also recommended to receive tecovirimat treatment.[12]According to Shamim et al,[27]tecovirimat demonstrated proven benefits in severe cases of mpox with no major safety concerns.A systematic review by Fox et al,[28]which included mostly nonrandomized studies,showed very low-certainty evidence that suggested no serious safety signals with the use of tecovirimat in people with mpox infection.They also found very low-certainty evidence that BCV may cause liver injury.
Tecovirimat is the first-line antiviral treatment for pregnant women with severe illness,and CDV and BCV should not be used in the first trimester of pregnancy.[29]Post-exposure prophylaxis for pregnant women with the JYNNEOS vaccine might prevent a poor fetal outcome.[29]The optimal time for post-exposure vaccination is within 4 d,although it can be considered up to 14 d after mpox exposure.[23]
Symptomatic pain management is recommended when treating mpox patients,as pain is a frequent and often severe symptom,prompting some patients to be hospitalized for pain management.Patients are encouraged to rinse their mouth with salt water for mouth lesions and can use viscous lidocaine for pain.For headache,muscle aches,pain from lesions,lymphadenopathy pain,and rectal pain,acetaminophen and ibuprofen are recommended as initial first-line pain management solutions.Pain from proctitis may require treatment with opioids.[9]
Self-inoculation can occur;therefore,patients are encouraged not to touch or scratch their rash.For patients with rash,topical preparations such as benzocaine,lidocaine gels,calamine lotion,or petroleum jelly can provide temporary relief.Oral antihistamines and a warm bath can also help patients with itching sensations.Patients with genital or anal rashes may also try sitz baths.[9]Ocular mpox can be treated with trifluridine 1% eyedrops every 2 h and should continue until all periocular lesions are healed but should not exceed 21 d to avoid ocular toxicity.[11,19]As previously mentioned,ocular involvement of mpox is considered a sign of serious illness and is an indication for tecovirimat therapy.[19]
Vaccine/prevention
Individuals who received the smallpox vaccine had some baseline protection against mpox infection,with an approximately 85% effective rate against the current mpox viral outbreak.[5,9]Two smallpox vaccines,JYNNEOS,ACAM2000,are being used as prophylaxis against mpox infection (Table 2).However,JYNNEOS possesses fewer adverse effects with no difference in effectiveness and is therefore the preferred agent for vaccination.[9]The JYNNEOS vaccine is administered in 2 doses,28 d (4weeks) apart between each shot.Deputy et al[30]reported that the adjusted vaccine efficacy (VE) for individuals receiving 2 doses (complete vaccination) was estimated to be 66.0%,and in patients receiving one dose (partial vaccination),it was 35.8%.A New York-based study reported that the adjusted VE of 1 dose of JYNNEOS (received ≥14 d earlier)or 2 doses combined was 75.7%,with the VE for 1 dose estimated to be 68.1% and that for 2 doses 88.5%.[31]
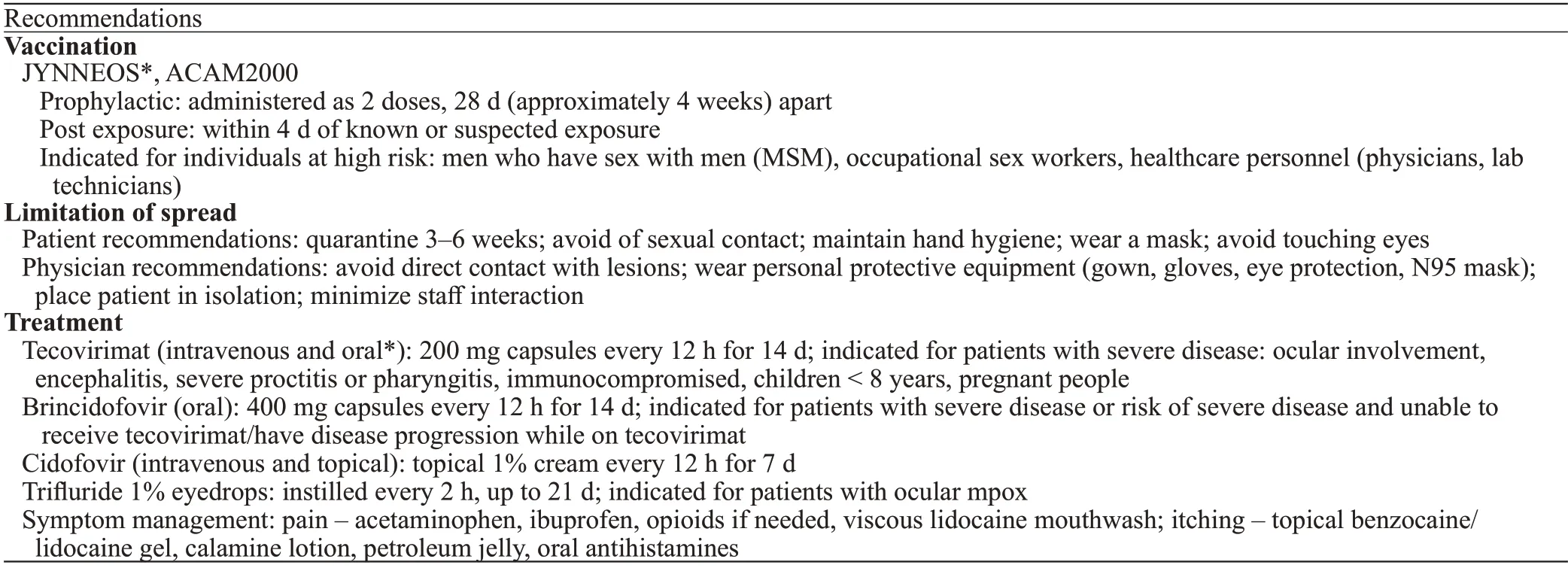
Table 2.A summary of recommendations for vaccination,limitation of spread,and treatment of mpox
The current recommendation is to prioritize vaccinations for individuals at high risk of exposure to mpox,which include MSM with multiple sexual partners,occupational sex workers,and health workers at high risk for exposure to mpox patients (emergency medicine personnel,primary care physicians,and laboratory personnel performing diagnostic tests).[29]Post-exposure administration of the vaccine within 4 d is recommended.[1]Transmission of mpox has been demonstrated to occur primarily as a result of skinto-skin contact;however,respiratory particles and surfaces or fomites have also been indicated.Multiple studies have shown high amounts of detectable virus on surfaces directly touched by a person with mpox.[12,15,32]To reduce the risk of infection and spread,individuals who test positive or are suspected to be positive should isolate and limit contact with others for 3-6 weeks.Providers should encourage avoidance of intimate contact and educate patients on using condoms,practicing safe sex,and having fewer sexual partners until all skin lesions have crusted,scabbed,and a fresh layer of skin has developed underneath.[1,33]Individuals should abstain from sex with anyone having a history of exposure for at least 21 d.Condom usage alone is not enough to safeguard against transmission of mpox virus because of alternative routes of transmission,such as droplets and fomites.[33]Patients who test positive or are suspected to test positive for mpox should maintain good hand hygiene,wear a fitted mask and cover their coughs and sneezes.
Individuals should disinfect high-touch areas in their homes to help reduce mpox spread.[9]To decrease the risk of autoinoculation of the ocular surface,patients with mpox should avoid touching their eyes and not use contact lenses.[19]To minimize the infection risk for healthcare professionals,they should avoid direct contact with skin lesions or materials used by mpox patients by wearing personal protective equipment (PPE),including a gown,gloves,eye protection,and a fitted N95 mask.Additional interventions include masking the patient,keeping their skin lesions covered and placing the patient in isolation.[9,23,32,33]
Gender/Ethnicity
During this current outbreak,96.4% of patients were male,with a median age of 34 years.In 84.2%of cases,patients identified their sexual orientation as MSM.Among the patients who disclosed their human immunodeficiency virus (HIV) status,approximately 48.4% were HIV-positive.[9]In large urban areas,95.7%and 2.3% of cases were in males and females,respectively,and in rural areas,94.7% and 4.6% of cases were in males and females,respectively.[34]In both urban and rural areas,the incidence among Black or African American and Hispanic or Latino persons was consistently higher than that among non-Hispanic White persons.[34]According to Zelaya et al,[34]the relative difference in incidence between Black and White persons was 7.2 in rural areas,and the absolute difference in large central urban areas in Black persons was 52.3 and in White persons was 19.7.
Complications from mpox infections are more common in children (<8 years old) and immunocompromised individuals,with an increased risk of secondary bacterial infection,sepsis,keratitis,encephalitis,pneumonia,or respiratory involvement.Vertical virus transmission has been shown to occur via the placenta from mother to fetus or through close contact during and after birth.Limited data suggest that mpox infection during pregnancy may lead to adverse outcomes for the fetus,and there is an increased risk of fetal loss and increased morbidity and mortality in the third trimester.[33]Some fetuses born of mpox-positive mothers have lesions,and mpox virus DNA has been detected in fetal tissue,umbilical cord,and placenta.[12,15,29,35]No current data exist regarding the risk of transmission via breastmilk,although there was one documented case of spread by breastfeeding due to the location and proximity of the lesions on the mother’s breast.[36]
HIV and other sexually transmitted diseases (STDs)
Mpox has predominantly affected the lesbian,gay,bisexual,transsexual,and queer/questioning (LGBTQ)+community,specifically young (aged 18-44 years) MSM.There are documented co-occurrences of associated sexually transmitted infections,including HIV,hepatitis,gonorrhea,chlamydia,syphilis,and pubic lice.[33]Patients co-infected with HIV are more likely to have larger skin rashes ≥2 cm,genital ulcers,secondary bacterial skin infections,and a longer duration of illness.[23]Previous studies in Africa stated that patients with untreated HIV infection had more extensive and longer-lasting lesions,more complications and an overall worse outcome.Co-infection with acquired immunodeficiency virus (AIDS) is reported in up to 41%of current cases.[11,37]In patients with AIDS,some atypical findings include more than 100 cutaneous lesions,necrotic or treatment-resistant lesions,hemodynamic instability,or secondary sepsis.[19]There is a high prevalence of concurrent STDs (17%-29%),with gonorrhea,chlamydia,and syphilis being the most common infections among patients with mpox.One study involving samples that were tested but found negative for mpox reported positive results for herpes simplex virus (HSV1,HSV2),varicella(VZV),andT.pallidum.Among the mpox-positive DNA samples,23% demonstrated co-infection with HSV2 and HSV1.[24]Between 84% and 100% of patients reported a new sex partner prior to the onset of symptoms.Recent receptive anal intercourse was associated with a >5-fold increased risk of proctitis due to mpox,and receptive oral intercourse was reported in the days preceding the diagnosis of 95% of patients who presented with tonsilitis due to mpox.[12,25]The odds ratio of being hospitalized either due to being HIV positive and immunosuppressed and having mpox is 2-fold.[38]
Deaths from mpox patients have been mostly connected to viral encephalitis,brain edema,and underlying immunocompromising disorders and comorbidities.[33]Most reports from the United States have identif ied that approximately 40% of individuals with mpox infection are persons who were HIV positive and were more likely to identify as Black or African American or as Hispanic or Latino.Viral hepatitis,anal or rectal abscesses,phimosis,and pneumonia were also more common in individuals living with HIV and positive for mpox.[39-41]
The clinical presentation of mpox as reported in New Zealand is similar and consistent with other literature documenting the clinical course and presentations from mpox elsewhere.It occurs in MSM,with transmission occurring from sexual contact and lesions documented in the perineal and anal areas.Severe complications that have been documented from these geographic regions include superinfected skin lesions,paronychia,cellulitis,anal and digestive involvement,angina with dysphagia,and ocular involvement (Table 3).[42,43]In Peru,reports of patients who tested positive for mpox were 96% male,56% MSM,and 55% with known HIV infection,re-affirming that there is a high co-infection rate between HIV and mpox.[43]
Societal knowledge and beliefs
There are multiple global studies focusing on the knowledge and societal beliefs regarding mpox.One Brazilian study focused on the MSM population and explored their willingness and interest in vaccination.Most participants (84.4%) agreed or strongly agreed that “LGBTQIA+individuals are being discriminated and stigmatized due to mpox.” Up to 96.9% of the population in the study were aware of what mpox was,and 95.1% were willing to get vaccinated for mpox.[3]In Bangladesh,higher vaccine intention was statistically significantly observed in individuals who had graduate-level education or above,but vaccine intention was significantly lower if participants self-identified as having high socioeconomic status.[44]Most Nepalese healthcare workers had a higher knowledge regarding mpox but insufficient critical awareness and perception,with 6% of respondents reporting that they had never heard about mpox.Similarly,8% of Indonesian healthcare workers had not heard about mpox until the surveyors approached them.[45]In China,77.9% of survey participants had ever heard of mpox,and 65.3% were aware of the global outbreak of mpox.However,only approximately half of them had a high level of knowledge regarding mpox (56.5%) and related symptoms (49.7%),and 68%-85% of people were willing to adopt precautions.[46,47]Japanese researchers performed a content analysis of tweets on Twitter in Japan and found that 56% of citizens wanted neutral information regarding basic facts about infectious diseases,treatment,vaccines,and other prevention methods.[48]Another USA-based study performed Twitter mapping before and after the WHO declared a public health emergency,and the results showed that after the WHO declared an emergency,accurate topics related to mpox and mitigation strategies emerged and spread effectively on Twitter.[49]As previously discussed,vaccines are encouraged for high-risk individuals and have been shown to be effective at minimizing symptoms and controlling the spread of mpox;however,the majority of available vaccines have been distributed to countries such as the USA and the United Kingdom,despite a global need.Although the mpox virus is native to African countries,vaccines and treatments have mostly been out of reach of African nations.[50]This mpox outbreak has again highlighted global inequities and emphasizes the need to address barriers to care to prevent vulnerable populations from having delays to care.[37]
CONCLUSION
Mpox outbreaks represent a new PHEIC.The symptoms are mostly non-specific,but rash and lymphadenopathy could distinguish mpox infection from others.Thorough history taking and physical examinations would helpclinicians make clinical diagnoses,although PCR tests of skin lesions are confirmatory.The preferred treatment included tecovirimat in patients with severe illness or at high risk of developing severe disease and vaccination with two doses of JYNNEOS.Certain patient populations are more vulnerable,for which clinicians should maintain a high index suspicion for diagnosis and treatment.
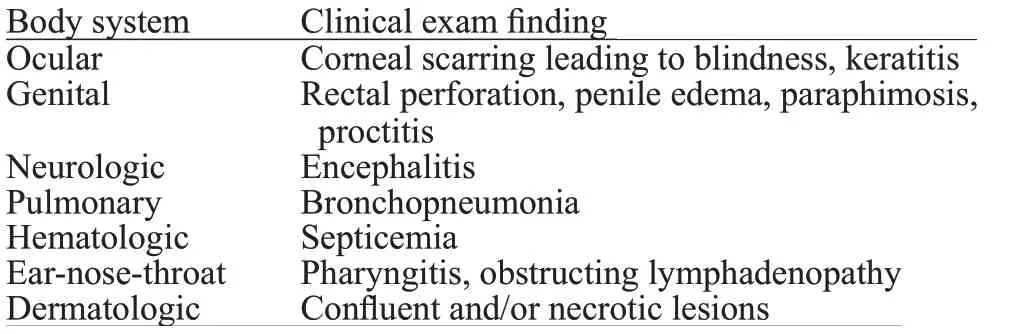
Table 3.Serious manifestations and complications of monkeypox by the body system
Funding:This is a non-funded study,with no compensation or honoraria for conducting the study.
Ethical approval:Not needed.
Conf licts of interest:The authors do not have a financial interest or relationship to disclose regarding this research project.
Contributors:Conceptualization: AP,QKT;data curation:CVL,AP,QKT;formal analysis: CVL,AP,QKT,MM;project administration: AP,QKT;writing -original draft: CVL,AP,QKT,MM,HH;writing -review &editing: CVL,AP,QKT,MM,HH.
 World journal of emergency medicine2023年5期
World journal of emergency medicine2023年5期
- World journal of emergency medicine的其它文章
- The neuro-prognostic value of the ion shift index in cardiac arrest patients following extracorporeal cardiopulmonary resuscitation
- A prospective cohort study on serum A20 as a prognostic biomarker of aneurysmal subarachnoid hemorrhage
- Mendelian randomization study to investigate the causal relationship between plasma homocysteine and chronic obstructive pulmonary disease
- Cardiopulmonary prognosis of prophylactic endotracheal intubation in patients with upper gastrointestinal bleeding undergoing endoscopy
- Effects of mesencephalic astrocyte-derived neurotrophic factor on sepsis-associated acute kidney injury
- Synchronized ventilation during resuscitation in pigs does not necessitate high inspiratory pressures to provide adequate oxygenation
