Clinical analysis of Wernicke encephalopathy after liver transplantation
Li-Min Ding , Li-Shan Deng , Jun-Jie Qian , Gang Liu , Lin Zhou ,Shu-Sen Zheng
a Division of Hepatobiliary Pancreatic Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou 310 0 03, China
b NHFPC Key Laboratory of Combined Multi-organ Transplantation, Hangzhou 310 0 03, China
c Key Laboratory of the Diagnosis and Treatment of Organ Transplantation, Chinese Academy of Medical Sciences, Hangzhou 310 0 03, China
d Key Laboratory of Organ Transplantation, Research Center for Diagnosis and Treatment of Hepatobiliary Diseases, Hangzhou 310 0 03, China
e Culture and Sports Center for the Disabled of Jiangxi Province, Nanchang 330 0 0 0, China
f Department of Transplantation, Jiangxi Provincial People’s Hospital, Nanchang 330 0 0 0, China
g Collaborative Innovation Center for Diagnosis Treatment of Infectious Diseases, Hangzhou 310 0 03, China
Keywords: Liver transplantation Wernicke encephalopathy Vitamin B1 Clinical presentations Imaging features Diagnosis Treatment Prognosis
ABSTRACT Background: Wernicke encephalopathy (WE) is an acute neurological disease resulting from vitamin B1 deficiency, and there are only very few case reports of WE after liver transplantation.The present study aimed to investigate the clinical characteristics, etiology, magnetic resonance imaging (MRI) features,treatment and prognosis of patients with WE after liver transplantation.Methods: Twenty-three patients with WE after liver transplantation from the First Affiliated Hospital,Zhejiang University School of Medicine and Jiangxi Provincial People’s Hospital between January 2011 and December 2021 were retrospectively analyzed.Results: Among the 23 patients diagnosed with WE after liver transplantation, 6 (26%) had a classic triad of impaired consciousness, oculomotor palsy and ataxia, and 17 (74%) had two features.The misdiagnosis rate was 65%.After treatment with high-dose vitamin B1, 19 (83%) patients showed improvement,whereas 4 (17%) showed no improvement, including 3 with residual short-term memory impairments and 1 with residual spatial and temporal disorientation and ataxia.Conclusions: The misdiagnosis rate is high in the early stage of WE, and the prognosis is closely associated with whether WE is diagnosed early and treated timely.High-dose glucose or glucocorticoids can trigger WE and cannot be administered before vitamin B1 treatment.Vitamin B1 is suggested to be used as a prophylactic treatment for patients with WE after liver transplantation.
Introduction
Wernicke encephalopathy (WE) is an acute neurological disorder caused by vitamin B1 deficiency [1].WE and vitamin B1 deficiency are often associated with chronic alcoholism.With the indepth development of liver transplantation technology in China,liver transplantation has become an effective life-saving treatment for patients with end-stage liver disease.To the best of our knowledge, there are only very few case reports of WE after liver transplantation [2-4].The prognosis for patients is better when WE is diagnosed early and treated timely after liver transplantation,while delayed diagnosis and treatment lead to irreversible neurological damage or even death [5].In the present study, we systematically retrospectively analyzed the clinical data of 23 patients with WE after liver transplantation and aimed to raise awareness of WE after liver transplantation among transplant surgeons.
Methods
Twenty-three patients with WE after liver transplantation from the First Affiliated Hospital, Zhejiang University School of Medicine and Jiangxi Provincial People’s Hospital between January 2011 andDecember 2021 were included.The inclusion criteria were patients diagnosed with WE according to the Caine’s criteria [6], which included: 1) history of malnutrition or alcoholism; 2) impaired consciousness; 3) oculomotor abnormalities; and 4) ataxia.The diagnosis of WE was made when 2 of the abovementioned 4 features were met.Patients with central nervous system damage due to other causes were excluded.The general data, clinical presentations, imaging features, treatment and prognosis were analyzed.
Results
Baseline characteristics of enrolled patients with WE after livertransplantation
There were 14 males and 9 females, with age ranging from 35 to 58 years.The primary diseases were hepatocellular carcinoma(primary liver cancer) in 8 cases, decompensated cirrhosis due to hepatitis in 9 cases, and decompensated alcoholic cirrhosis in 6 cases.Preoperative liver function assessed by Child-Pugh classification showed that 2, 3, and 18 patients were classified as grades A,B, and C, respectively.The preoperative nutritional status assessed by subjective global assessment (SGA) showed that 6 patients had moderate malnutrition, and 17 had severe malnutrition.Ten patients received piggyback liver transplantation, and 13 received classical orthotopic liver transplantation.The bile duct was reconstructed using end-to-end continuous sutures.The routine postoperative medicine administration regimens included anti-infection,acid suppression, liver protection, anticoagulation, anti-hepatitis B virus (HBV), and nutritional support therapies.The immunosuppressive regimens were tacrolimus (FK506) and mycophenolate mofetil (MMF) for recipients with hepatocellular carcinoma, and FK506, MMF and steroids for recipients with non-hepatocellular carcinoma.Anti-HBV treatment included hepatitis B immune globulin and anti-HBV drugs after discharge.For those who were confirmed or suspected resistance to lamivudine, entecavir or telbivudine, tenofovir was administered.The HBV-DNA after liver transplantation was monitored.
Patients were routinely followed up after surgery.Routine hematological, biochemistry and coagulation tests were performed daily within 1 week after surgery.Pathogen detection was performed at day 3 after surgery.Immunosuppressant blood levels were measured twice a week.Patients underwent ultrasound every 3 days, or bedside chest radiography if necessary.Lung and abdominal computed tomography (CT) scans were performed at week 2 after surgery, and CT angiography (CTA) of the liver was performed 1 month after surgery.Patients also received regular brain MRI re-examination after liver transplantation.The clinical characteristics of patients with WE after liver transplantation are shown in Table 1.
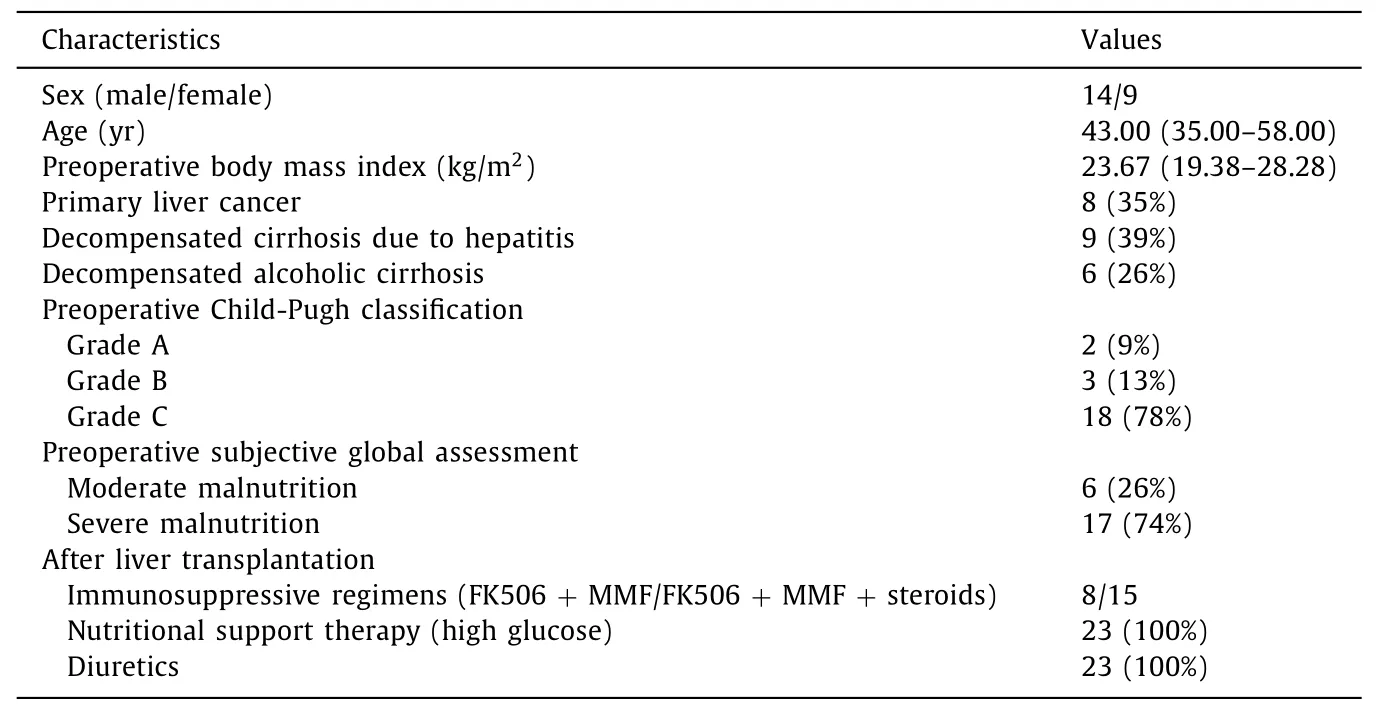
Table 1Clinical characteristics of patients with Wernicke encephalopathy (WE) after liver transplantation ( n = 23).
Clinical presentations, laboratory tests and imaging
After liver transplantation, 19 (83%) patients developed onset of acute WE, and 4 (17%) patients developed onset of subacute WE.Among these 23 patients, 6 (26%) had a classic triad of impaired consciousness, oculomotor palsy and ataxia, and all these 6 patients had decompensated alcoholic cirrhosis; 17 (74%) had two features.Other non-specific symptoms included memory loss and numbness in the extremities.The liver function, blood ammonia,and blood sodium levels in these 23 patients gradually returned to normal after liver transplantation ( Table 2 ).In order to confirm the diagnosis of WE, all 23 patients underwent cerebrospinal fluid (CSF) examination; 6 showed mildly elevated CSF protein levels, while no positive results were found in the remaining patients.All 23 patients underwent electroencephalogram (EEG) examination, and mild abnormal EEG was found in 4 patients.Brain MRI revealed varying degrees of T2-weighted and fluid-attenuated inversion-recovery (FLAIR) hyperintensity in the thalamus, third and fourth ventricles, and periaqueductal region in 23 patients before receiving treatment for WE ( Fig.1 ).After treatment with highdose vitamin B1, the abnormal signal in the corresponding brain regions was obviously improved ( Fig.2 ).
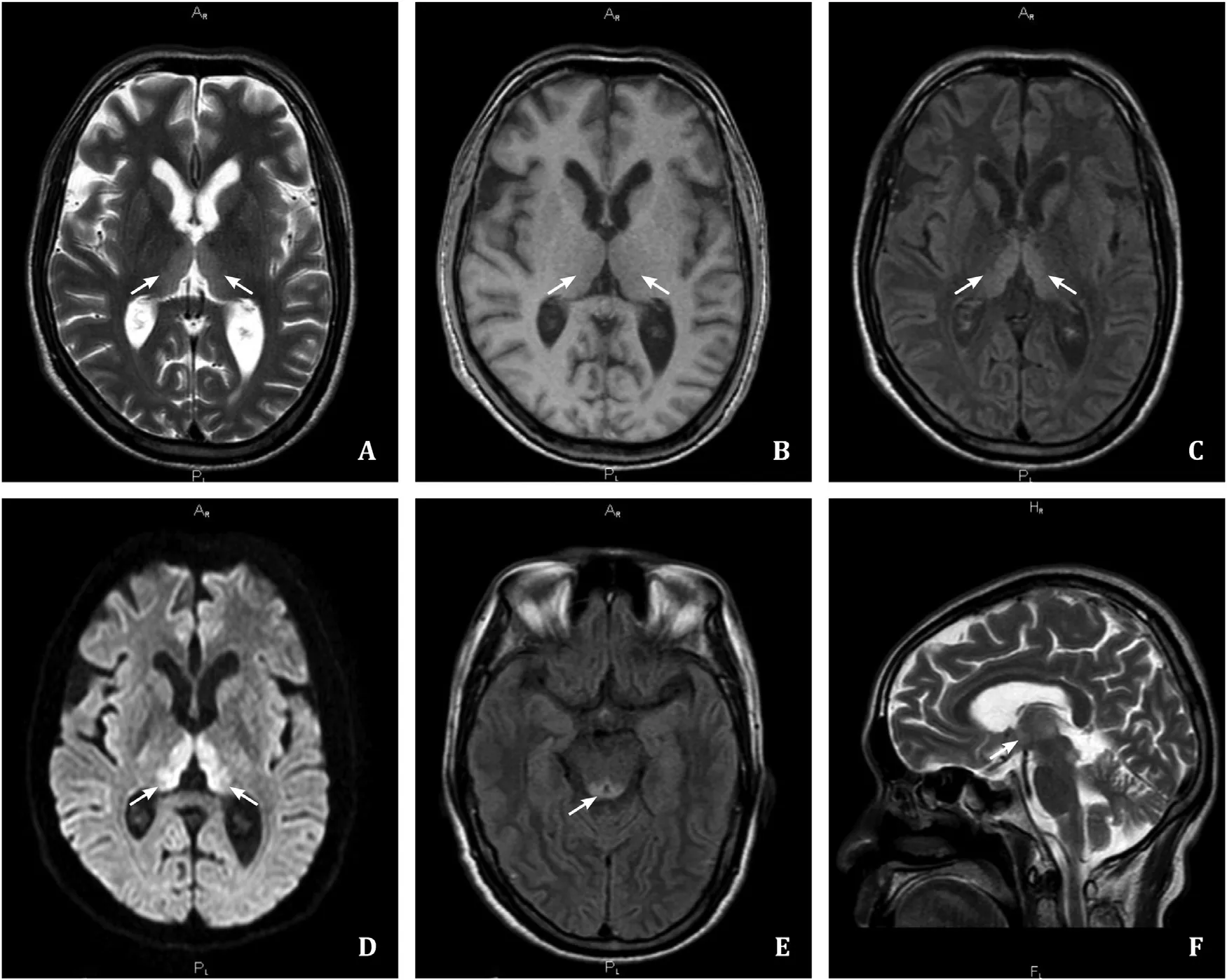
Fig.1.Brain MRI showed symmetric T1 hypointensity, slight T2, FLAIR, and DWI hyperintensity in the bilateral thalami, third and fourth ventricles and midbrain periaqueductal region.A: T2WI showed bilateral thalamic hyperintensity; B: T1WI showed bilateral thalamic hypointense; C: FLAIR showed bilateral thalamic hyperintensity; D: DWI showed bilateral thalamic hyperintensity; E: FLAIR showed high signal in the midbrain aqueduct; F: T2WI showed high signal intensity in the third ventricle.MRI: magnetic resonance imaging; FLAIR: fluid attenuated inversion recovery; DWI: diffusion weighted imaging; T1WI: T1 weighted imaging; T2WI: T2 weighted imaging.
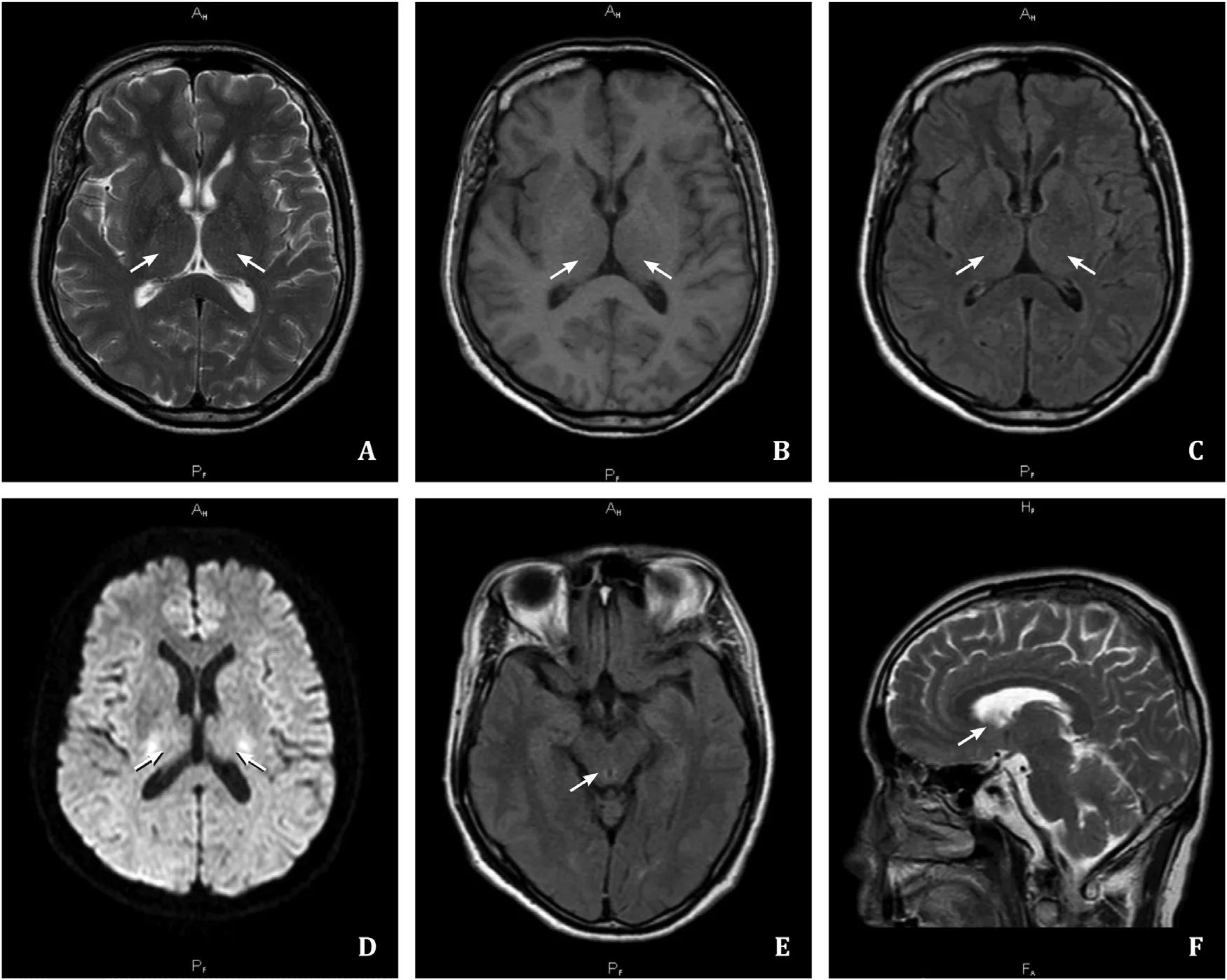
Fig.2.Brain MRI after vitamin B1 treatment.The abnormal signal in the corresponding brain regions was obviously improved after vitamin B1 treatment than before treatment.MRI: magnetic resonance imaging.
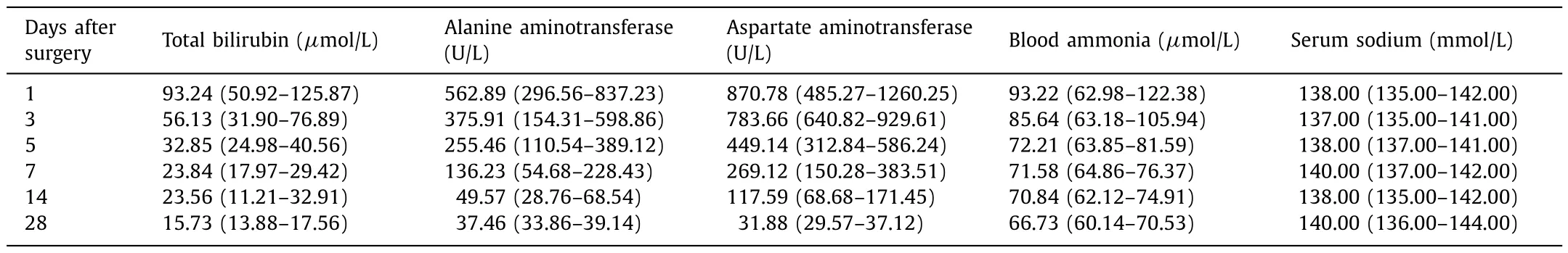
Table 2Liver function and blood ammonia levels in 23 patients with Wernicke encephalopathy after liver transplantation.
Treatment and prognosis of patients with WE after liver transplantation
Among these 23 patients, 15 were misdiagnosed with other neurological diseases such as hepatic encephalopathy, intracranial infection, and cerebral infarction.The misdiagnosis rate was as high as 65%.After the diagnosis of WE was made, these 23 patients were treated with intramuscular high-dose vitamin B1 (100 mg)three times a day.Nineteen (83%) patients showed improvement after treatment, while 4 (17%) showed no improvement, including 3 presenting with residual short-term memory impairment, and 1 with spatial and temporal disorientation and ataxia.After hospital discharge, patients were required to receive rehabilitation treatment, and underwent outpatient follow-up examination.Oral vitamin B1 treatment was continued (3 times a day, 100 mg once).
Discussion
WE was first described in 1881 by Carl Wernicke as an acute neurological disease resulting from vitamin B1 deficiency.Vitamin B1 is also known as thiamine.Thiamine pyrophosphate is the biologically active form of vitamin B1, which is an essential coenzyme in several biochemical pathways in the brain [7].Vitamin B1 deficiency leads to impaired glucose, lipid, and amino acid metabolism, decreased adenosine triphosphate (ATP) synthesis in the brain, excitotoxicity, oxidative stress, inflammatory responses, blood-brain barrier disruption, impairment of neurotransmitter synthesis and transport, resulting in myelin damage and neuronal apoptosis.Brain regions commonly affected by vitamin B1 deficiency are the mediodorsal thalamic nucleus, mammillary bodies, periaqueductal region, and third and fourth ventricles.The cranial nerve nucleus, cerebellum, brainstem and cerebral cortex can also be involved [8].The body can store 30 mg of thiamine.The thiamine requirement for healthy individuals is 1 mg per day,which can be maintained for 18-20 days under conditions with increased metabolic demands [9].The main cause of WE is vitamin B1 deficiency; all factors that can cause insufficient intake and absorption of vitamin B1 or metabolic disturbance, and increased metabolic consumption of vitamin B1 in the body can both lead to WE [10].The most common cause of WE is chronic alcoholism,while non-alcoholic WE is mainly associated with long-term intravenous hyperalimentation, malnutrition, improper feeding of infants and children, recurrent vomiting, diarrhea, and poor appetite caused by severe disorders of liver, stomach, bile ducts, and pancreas in the digestive system.Vomiting during pregnancy, anorexia nervosa, replacement therapy for liver and renal failure, malignant tumors, disseminated tuberculosis, and bone marrow transplantation can both cause insufficient intake or increased consumption of vitamin B1, thus leading to WE [11-13].
After liver transplantation, many factors can trigger vitamin B1 deficiency or aggravate the existing vitamin B1 deficiency [ 14 , 15 ].The pathophysiological characteristics of vitamin B1 deficiency in liver transplant recipients are manifested in many ways: preoperative chronic liver disease leading to a decrease in vitamin B1 storage, and a decrease in the ability of biological activation [16].Among 23 patients with WE after liver transplantation included in the present study, 18 were classified as Child-Pugh grade C before surgery, accounting for 78% of all patients, and 17 had preoperative severe malnutrition, accounting for 74% of all patients.In addition, the high metabolic consumption states after liver transplantation and postoperative rehabilitation increased the requirements for vitamin B1.Total parenteral nutrition with high glucose or high-carbohydrate diets was administered due to short-term inadequate food intake and gastrointestinal disturbances (vomiting,nausea and diarrhea), which increased the consumption of vitamin B1 [17-19].In the present study, all 23 patients were supplemented with high glucose to strengthen nutritional support after surgery, which promoted the development of WE.Diuretics were used to treat ascites, which can also increase the excretion of vitamin B1 and hypomagnesemia that is also related to vitamin B1 deficiency.Magnesium is an essential cofactor for the conversion of thiamine to its active diphosphate and triphosphate forms.Magnesium deficiency can reduce the effect of thiamine, and affect its absorption [20].In the present study, all 23 patients were treated with different doses of diuretics after surgery.Furthermore, immunosuppressive therapy is routinely used after liver transplantation.Currently, the commonly used immunosuppressants include calcineurin inhibitors and steroids.Calcineurin inhibitors can induce neurotoxicity, and have an increased vitamin B1 requirement due to detoxification processes, mitochondrial uncoupling and oxidative stress [21].In the present study, all patients received immunosuppressive therapy with tacrolimus after surgery.The application of steroids after liver transplantation, the increase in endogenous cortisol production due to surgical stress and anesthetic drugs, and the obvious effect of steroids on glucose metabolism aggravate pyruvate accumulation, which are important triggers for the development of WE [22].In the present study, 15 patients with benign liver disease received different doses of steroids in order to prevent rejection after surgery.
WE after liver transplantation can present as acute or subacute onset, which is characterized by a triad of altered consciousness,oculomotor palsy and ataxia [23], but only 16% patients with WE exhibit all these three features, while most recipients have atypical symptoms [24], which makes early diagnosis of WE difficult.In the present study, only 26% patients had the complete triad, and these patients had decompensated alcoholic cirrhosis.This may be due to the presence of pre-transplant severe vitamin B1 deficiency.At present, due to technical difficulties and higher costs, the diagnosis of WE by detecting erythrocyte transketolase activity or serum thiamine and thiamine pyrophosphate concentrations cannot be widespread.In the early stage of WE, CSF examination occasionally shows mildly elevated CSF protein levels, and the EEG isusually normal.In the late stage of WE, EEG may show non-specific and diffuse slow waves.The abovementioned examinations are not specific.Brain magnetic resonance imaging (MRI) is currently considered the most valuable method for diagnosing WE, with a sensitivity of 53% and a specificity of 93% [25].Brain MRI has been used as the first choice in patients with WE, but normal MRI findings cannot rule out WE.The typical MRI features of WE are T2 and FLAIR hyperintensity in the thalamus, third and fourth ventricles,and periaqueductal region [26].The MRI features of patients with WE after liver transplantation observed in this study are consistent with the abovementioned findings.Although laboratory tests and neuroimaging are useful in the diagnosis of WE, the diagnosis of WE relies primarily on clinical symptoms.According to the Caine’s criteria, diagnosis of WE should be considered if patients have at least two of the following features: 1) history of malnutrition or alcoholism; 2) impaired consciousness; 3) oculomotor abnormalities;and 4) ataxia.Although the Caine’s criteria is more sensitive for the diagnosis of WE, the classic triad of impaired consciousness,oculomotor palsy and ataxia, is more specific, and the diagnosis by classic triad can also be confirmed by the positive response of neurological signs to vitamin B1 supplementation [6].
Hepatic encephalopathy or neurological diseases such as neurological infections, cerebrovascular accidents, and demyelination syndrome should be excluded in patients after liver transplantation.The early symptoms of WE are often masked by the severity of the primary disease symptoms, leading to misdiagnosis and underdiagnosis [ 27 , 28 ].In the present study, the liver function and blood ammonia levels in patients gradually returned to normal after surgery, but the misdiagnosis rate of WE in the early stage was as high as 65%.This may be due to the following reasons: 1)transplant physicians mainly consider diseases such as hepatic encephalopathy, central nervous system infections, and cerebrovascular accidents, but have insufficient awareness of WE.They neglect to apply vitamin B1 supplementation in patients with chronic liver disease or patients who were fasted for prolonged time.2) Despite of the wasting diseases and the high metabolic state after liver transplantation, increased consumption of vitamin B1 is not considered, and vitamin B1 supplementation is therefore not considered.3) The effect of perioperative medicine administration (such as the use of calcineurin inhibitors, steroids and diuretics) on absorption and utilization of vitamin B1 is not adequately considered.The diagnosis of WE is not made early based on clinical symptoms and imaging findings, resulting in further delays in the treatment.WE can be improved or even cured by early diagnosis and timely treatment with vitamin B1.If diagnosis and treatment are delayed,WE can develop into Korsakoff’s syndrome which is also known as organic amnestic syndrome, and characterized by selective cognitive impairments, including short-term memory loss, and temporal and spatial disorientation.The persistence of this syndrome may eventually result in irreversible damage to the nervous system and even death [14].Administration of vitamin B1 (10 0-30 0 mg/d)before and after liver transplantation is considered a prophylactic treatment for WE.It is usually administered imtramuscularly for 2 weeks and then changed to oral vitamins, until the recipients can resume normal diet.The eye movement disorder begins to recover in about 3 to 7 days, while most patients recover completely within 1 to 2 months.For cases with a suspected or confirmed diagnosis of WE, high-dose vitamin B1 treatment should be adopted immediately to avoid progression to Korsakoff’s syndrome or death.If patients’ symptoms are severe with mania, convulsions or delusions, and cannot cooperate with the treatment, midazolam and habination mixture can be administered intravenously as appropriate to put the patient in a sleep or semi-sleep state in order to pass the critical phase.Vitamin B1 must be given prior to supplementation of glucose in parenteral nutrition support.When WE occurs, glucose infusion should be avoided until vitamin B1 treatment is applied in order to prevent further deterioration.In the present study, the symptoms in 19 (83%) patients with WE were improved, while no obvious improvement was found in 4 patients.Among these 4 patients, 3 had residual short-term memory impairments, 1 had residual spatial and temporal disorientation and ataxia, indicating that some recipients still had varying degrees of sequelae even after vitamin B1 treatment.
WE is a severe neurological complication after liver transplantation, which is commonly overlooked or neglected in clinical practice.At present, the number of liver transplant cases in China is increasing rapidly every year, and postoperative management is becoming more and more refined and sophisticated [29].Central nervous system complications have become growing concerns and pressing challenges.WE after liver transplantation can be treated and prevented timely, and vitamin B1 supplementation is required routinely for liver transplant recipients to prevent WE after liver transplantation.It is recommended to administer vitamin B1 before or during glucose infusion, especially in patients with decompensated alcoholic cirrhosis and preoperative severe malnutrition [30].Once one of the symptoms, neuropsychiatric symptoms, eye movement disorder or gait instability, is present,WE should be highly suspected, MRI should be performed as soon as possible, and vitamin B1 treatment should be commenced immediately.
Acknowledgments
None.
CRediT authorship contribution statement
Li-Min Ding:Data curation, Formal analysis, Writing - original draft.Li-Shan Deng:Data curation, Methodology, Writing - original draft.Jun-Jie Qian:Writing - original draft.Gang Liu:Writing - original draft.Lin Zhou:Methodology.Shu-Sen Zheng:Conceptualization, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
This study was approved by Jiangxi Provincial People’s Hospital and First Affiliated Hospital, Zhejiang University School of Medicine(2022068 and 2022370).Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年4期
Hepatobiliary & Pancreatic Diseases International2023年4期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Hypermethylation of thymosin β4 predicts a poor prognosis for patients with acute-on-chronic hepatitis B liver failure
- Novel re-intervention device for occluded multiple uncovered self-expandable metal stent (with video)
- The impact of metabolic dysfunction-associated fatty liver disease on the prognosis of patients with hepatocellular carcinoma after radical resection
- Laparoscopic liver resection for hepatocellular carcinoma complicated with significant portal hypertension: A propensity score-matched survival analysis
- Hepatobiliary&Pancreatic Diseases International
- Wnt/beta-catenin signaling and its modulators in nonalcoholic fatty liver diseases
