脊髓损伤后呼吸肌训练的研究进展
虎良吉娜 王文丽
【摘要】 呼吸肌训练(respiratory muscle training,RMT)作为肺康复的重要组成部分,能帮助脊髓损伤(spinal cord injury,SCI)患者提高肺功能,改善活动能力,降低肺部并发症发生率和死亡率,提高患者生活质量。近年来,多项研究不仅提出了更详细、更全面的SCI后呼吸肌的评估内容,还提出了新的抗阻呼吸训练方案,以及新的RMT方法,如声乐呼吸训练、居家高强度训练、腹部牵拉(abdominal drawing in maneuver,ADIM)配合RMT法、高频脊髓刺激法,这能最大程度激活SCI患者的呼吸肌,大幅改善患者的肺功能,并满足患者居家肺康复的需求。
【关键词】 脊髓损伤 呼吸肌训练 抗阻呼吸训练 肺康复
Research Progress of Respiratory Muscle Training after Spinal Cord Injury/HU Liangji'na, WANG Wenli. //Medical Innovation of China, 2023, 20(10): -168
[Abstract] Respiratory muscle training (RMT), as an important part of pulmonary rehabilitation, can help patients with spinal cord injury (SCI) improve pulmonary function, improve mobility, reduce the incidence of pulmonary complications and mortality, and improve the quality of life of patients. In recent years, many studies have not only proposed more detailed and comprehensive assessment of respiratory muscle after SCI, but also proposed new anti-resistance respiratory training scheme and new RMT methods, such as vocal respiratory training, home-based high-intensity training, abdominal drawing in maneuver (ADIM) combined with RMT and high-frequency spinal cord stimulation, which can maximize the activation of respiratory muscle in SCI patients and significantly improve lung function, and meet the needs of patients' home-based lung rehabilitation.
[Key words] SCI RMT Anti-resistance respiratory training Lung rehabilitation
First-author's address: The Second Affiliated Hospital of Kunming Medical University, Kunming 650106, China
doi:10.3969/j.issn.1674-4985.2023.10.039
脊髓损伤(SCI)是指由于各种因素如创伤、畸形、感染或医源性因素等导致脊髓的结构和功能受损,导致患者生活自理能力、功能活动能力、生活质量下降的一类疾病[1-4]。SCI患者普遍存在肺功能下降的问题,损伤平面越高,肺功能下降得越多[5-6]。其中,发生在颈段和上胸段的SCI会影响到呼气肌和吸气肌的功能[7],从而影响肺功能。急性颈椎SCI患者入院时存在限制性通气障碍[8-10]。研究显示,严重呼吸功能障碍是SCI急性期和慢性期患者死亡的主要因素,而36%~83%的SCI患者存在严重的呼吸功能障碍[11]。SCI后呼吸功能障碍可能会带来更多的肺部并发症,增加患者死亡率,延长住院时间[12-16]。1967年,Imamura[17]的研究首次提出呼吸肌训练(RMT)能够帮助颈段SCI患者改善肺功能。RMT旨在通过使用阻抗负荷和阈值压力负荷等方法来提高呼吸肌的力量和耐力[18],包括使用阻力训练器和阈值训练器,以及有效和同步地刺激吸气和呼气肌肉的歌唱训练等。近年来,新的呼吸肌训练技术、作用机制和应用创新层出不穷,也有越来越多研究指出RMT對改善SCI患者的呼吸功能具有积极意义,但对其总结归纳的信息却相对较少。因此,本文将论述和总结该领域国内外的最新研究进展。
1 SCI对呼吸肌的影响
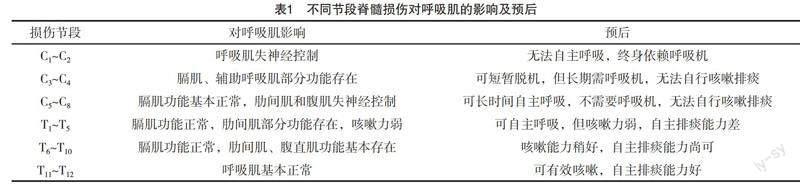
颈段、胸段、腰段脊髓包含支配吸气肌、呼气肌、辅助呼吸肌的运动神经元[19]。吸气肌包括膈肌、肋间外肌、斜角肌,呼气肌主要包括腹直肌、肋间内肌、腹内斜肌,辅助呼吸肌包括胸锁乳突肌、斜角肌、斜方肌[20],具体如表1所示。研究显示,SCI患者膈肌血管供应发生改变,限制氧气弥散功能。膈肌活动的恢复可以逆转这些变化,恢复对组织的氧气供应,并使肌肉功能特性得以恢复[21]。
2 呼吸肌功能的评估
通过球海绵体反射结果,确定患者不处于脊休克期后可根据美国脊髓损伤协会(American Spinal Cord Injury Association,ASIA)分级标准评估患者感觉和运动,确定损伤平面[22]。然后,评估患者呼吸模式、呼吸动度、咳嗽能力,同时使用改进的Borg量表评估患者平静状态和不同活动期间呼吸困难的严重程度,量表从0分(没有呼吸困难)至10分(无法忍受的呼吸困难)评估[23]。此外,通过肺通气功能测试,可获得结果包括肺总量(total lung capacity,TCL)、肺活量(vital capacity,VC)、深吸气量(inspiratory capacity,IC)、最大吸气压(maximal inspiration pressure,MIP)、最大呼气压(maximal expiration pressure,MEP)、最大自主通气量(maximal voluntary ventilation,MVV)、用力肺活量(forced vital capacity,FVC)、第一秒用力肺活量(forced expiratory volume in the first second,FEV1)等。
3 呼吸肌训练
3.1 抗阻呼吸训练 研究表明,呼吸肌训练对于增加SCI患者的呼吸肌力量和肺容量是有效的[24-27]。治疗师可通过阈值训练器训练患者吸气肌,嘱患者用手捏住鼻翼,用嘴呼吸,缓慢吐气后尽可能快而多地吸气,起始阻力为60% MIP,每周5次,每次训练包括7组呼吸,其中每组包括2 min的阈值训练器抗阻吸气和1 min无阻力呼吸。为让患者更好地适应,第一周可以从3组呼吸开始,慢慢增加到7组[28]。
3.2 居家高强度训练 患者可通过使用Dofin呼吸训练器(台北GaleMed公司)进行呼吸肌训练。该设备允许患者训练吸气和呼气肌肉并独立调节负荷,可将负荷调节至10~70 cmH2O[29-30]。使用该设备进行为期10周的呼吸肌训练,每天2次,每次4组4 min的呼吸训练,每组之间休息1 min,初始训练负荷为50% MIP/MEP,每周请治疗师评估一次,评估后再将训练负荷调整为新测MIP/MEP的50%。研究表明,该训练方案能够改善肺功能和耐力,并减少呼吸肌无力的SCI患者的呼吸困难[31-32]。时间是肺功能恢复的关键因素,而RMT在肺功能改善与时间中有显著的交互作用。
3.3 声乐呼吸训练(VRT) VRT是一种与声带肌肉相关的治疗,通常是音乐疗法(music therapy,MT)的一个组成部分,侧重于加强呼吸肌肉和改善肺功能。每个30 min的VRT培训课程包含以下部分:前10 min,治疗师带领患者唱一首短曲,然后引导患者用断音唱法唱短旋律增强腹肌力量。在接下来的10 min内,治疗师指导患者唱元音不同的音调旋律线。在最后10 min,患者被要求唱具体歌曲,歌曲是根据等级选择的中国音乐家协会声乐考试1-3(徐和龚,2014)。每次训练30 min,每周5次,共12周。研究发现12周后,患者的肺功能指标显著提高,其机制可能为基于MT的VRT不仅能够改善呼吸肌功能,还能使延髓呼吸中枢神经纤维束数量、长度、厚度、密度增加,从而影响神经可塑性[33]。
3.4 腹部牵拉(ADIM)配合呼吸肌训练 腹部肌肉是主要的用力呼气肌,包括腹直肌、腹斜肌、腹横肌等。ADIM的目的在于牵拉腹部肌群,通过本体感觉刺激,使呼气肌收缩,尤其是腹横肌。此时配合呼吸肌训练,可以使膈肌收缩,产生向下的活动,与此同时,腹横肌向内收缩,两者共同运动使得腹内压增加,脊柱稳定性增加,呼吸肌效能提高,患者的呼吸功能得以改善[34]。具体做法是,患者取俯卧位,将压力生物反馈装置放置在患者下腹部和垫子之间,使压力值达到50 mmHg。根据模拟压力计的视觉反馈,要求受试者在俯卧位保持低于6~10 mmHg的压力,然后进行5 s的等长收缩。在保持5 s后,允许患者休息2~3 s。该练习共进行五组(每组重复 10 次),组间患者可以休息1次。
3.5 高频脊髓刺激法 在最近一项针对SCI受试者的人体临床试验中,证明了较低频的胸椎脊髓刺激(SCS,50 Hz)会激活呼气肌,并产生正常咳嗽所特有的大气道正压和高峰值气流速率[35]。恢复有效咳嗽可以更轻松地增加分泌物,降低呼吸道感染的发生率,并提高生活质量。不幸的是,通过这种技术激活呼吸肌需要高刺激幅度(30~40 V),因此不能应用于感觉完整的患者,因為刺激会由于感觉纤维激活而导致明显的不适。而近期研究表明,高频SCS (HFSCS)可以提供相同水平的呼气肌激活,但刺激感更弱,因此更适合应用于改善SCI患者的呼吸肌功能[36]。
4 小结与展望
越来越多的研究证明,RMT能够有效改善SCI患者肺功能,降低肺部并发症的发生率,降低SCI可能带来的死亡率,提高患者生活质量,减少医疗负担。但是不同步的经济发展和医疗资源分配不均匀,也使得偏远地区的SCI患者难以受到最早期、最及时的治疗,而往往偏远地区的SCI患者比例更高。这既是对资源管理的挑战,也是对医务者本身的挑战。如何在环境、经费、条件有限的情况下,制订出最适合患者的RMT计划,如何让患者能够做正确、做好、能长期坚持下去,这是值得每个医务者深思的问题。本文总结了目前SCI患者RMT相关的评估、治疗相关发展现状,但仍缺乏更多证据更高、样本量更大、观点更新颖的优质文章,这些仍是我们需要去攻克的方向。
参考文献
[1] CHOI E H, GATTAS S, BROWN N J,et al.Epidural electrical stimulation for spinal cord injury[J].Neural Regen Res,2021,16(12):2367-2375.
[2]魏卫兵,周祥兴,周宾宾,等.构建不同脊髓损伤节段模型大鼠下肢功能恢复的评价[J].中国组织工程研究,2019,23(7):1073-1077.
[3] KRASSIOUKOV A.Autonomic function following cervical spinal cord injury[J].Respir Physiol Neurobiol,2009,169(2):157-164.
[4] BACH J R.Prevention of respiratory complications of spinal cord injury: a challenge to "model" spinal cord injury units[J].J Spinal Cord Med,2006,29(1):3-4.
[5]徐基民,李建军,魏鹏绪,等.脊髓损伤患者的肺功能变化[J].中华物理医学与康复杂志,2007,29(12):811-814.
[6]余凤立,敖丽娟,刘芳,等.不同平面脊髓损伤患者膈肌运动和肺功能的相关分析[J].中国康复,2019,34(1):12-14.
[7] SPUNGEN A M,GRIMM D R,LESSER M,et al.Self-reported prevalence of pulmonary symptoms in subjects with spinal cord injury[J].Spinal Cord, 1997,35(10):652-657.
[8] WANG H C,CHEN K Y,LIN Y T,et al.Factors associated with prolonged mechanical ventilation and re-ventilation in acute cervical spinal cord injury patients[J/OL].Spine (Phila Pa 1976),2020,45(9):E515-E524.https://pubmed.ncbi.nlm.nih.gov/32282654/.
[9] USHIKU C,SUDA K, MATSUMOTO S,et al.Time course of respiratory dysfunction and motor paralysis for 12 weeks in cervical spinal cord injury without bone injury[J].Spine Surg Relat Res,2018,3(1):37-42.
[10] SCHILERO G J,SPUNGEN A M,BAUMAN W A,et al.
Pulmonary function and spinal cord injury[J].Respir Physiol Neurobiol,2009,166(3):129-141.
[11]郭佳寶,朱毅.吸气肌训练的临床研究进展[J].中国康复医学杂志,2014,29(9):888-892.
[12] DRAGHICI A E,TAYLOR J A.Baroreflex autonomic control in human spinal cord injury: physiology, measurement, and potential alterations[J].Auton Neurosci,2018,209:37-42.
[13] GARSHICK E,KELLEY A,COHEN S A,et al.A prospective assessment of mortality in chronic spinal cord injury[J].Spinal Cord,2005,43(7):408-416.
[14] MIDDLETON J W,DAYTON A,WALSH J,et al.Life expectancy after spinal cord injury: a 50-year study[J].Spinal Cord,2012,50(11):803-811.
[15] BROWN R,DIMARCO A F,HOIT J D,et al.Respiratory dysfunction and management in spinal cord injury[J].Respir Care,2006,51(8):853-868.
[16] AARABI B,HARROP J S,TATOR C H,et al.Predictors of pulmonary complications in blunt traumatic spinal cord injury[J].J Neurosurg Spine,2012,17(1):38-45.
[17] IMAMURA T.The effect of auxiliary respiratory muscular training on breathing exercise in cervical cord injuries[J].Kumamoto Igakkai Zasshi,1967,41(2):130-151.
[18] MARKOV G,SPENGLER C M,KN?PFLI-LENZIN C,et al.
Respiratory muscle training increases cycling endurance without affecting cardiovascular responses to exercise[J].Eur J Appl Physiol,2001,85(3-4):233-239.
[19] LANE M A.Spinal respiratory motoneurons and interneurons[J].Respir Physiol Neurobiol,2011,179(1):3-13.
[20] TERSON DE PALEVILLE D G,MCKAY W B,FOLZ R J,et al.Respiratory motor control disrupted by spinal cord injury: mechanisms,evaluation,and restoration[J].Transl Stroke Res,2011,2(4),463-473.
[21] WARREN P M,KISSANE R W P,EGGINTON S,et al.
Oxygen transport kinetics underpin rapid and robust diaphragm recovery following chronic spinal cord injury[J].J Physiol,2021,599(4):1199-1224.
[22] DUDLEY-JAVOROSKI S,SHIELDS R K.Muscle and bone plasticity after spinal cord injury: review of adaptations to disuse and to electrical muscle stimulation[J].J Rehabil Res Dev,2008,45(2):283-296.
[23] JOHNSON M J,CLOSE L,GILLON S C,et al.Use of the modified borg scale and numerical rating scale to measure chronic breathlessness: a pooled data analysis[J].Eur Respir J,2016,47(6):1861-1864.
[24] LEGG DITTERLINE B E,ASLAN S C,RANDALL D C,et al.
Effects of respiratory training onheart rate variability and baroreflex sensitivity in individuals with chronic spinal cord injury[J].Arch Phys Med Rehabil,2018,99(3):423-432.
[25] BERLOWITZ D J,TAMPLIN J.Respiratory muscle training for cervical spinal cord injury[J].Cochrane Database Syst Rev,2013,23(7):CD008507.
[26] KARADALL M N,BOSNAK-GUCLU M,CAMCIOGLU B,
et al.Effects of inspiratory muscle training in subjects with sarcoidosis: a randomized controlled clinical trial[J].Respir Care,2016,61(4):483-494.
[27] BERLOWITZ D J,WADSWORTH B,ROSS J.Respiratory problems and management in people with spinal cord injury[J].Breathe (Sheff),2016,12(4):328-340.
[28] POSTMA K,HAISMA J A,HOPMAN M T E,et al.Resistive inspiratory muscle training in people with spinal cord injury during inpatient rehabilitation:a randomized controlled trial[J].Physical Therapy,2014,94(12):1709-1719.
[29] PARREIRAS D E,MENEZES K K,NASCIMENTO L R,et al.
High-intensity respiratory muscle training improves strength and dyspnea poststroke: a double-blind randomized trial[J].Arch Phys Med Rehabil,2019,100(2):205-212.
[30] MARCO E,RAMIREZ-SARMIENTO A L,COLOMA A,et al.
High-intensity vs. sham inspiratory muscle training in patients with chronic heart failure: a prospective randomized trial[J].Eur J Heart Fail,2013,15(8):892-901.
[31] MENEZES K K P,NASCIMENTO L R,POLESE J C,et al.
Effect of high-intensity home-based respiratory muscle training on strength of respiratory muscles following a stroke: a protocol for a randomized controlled trial[J].Braz J Phys Ther,2017,21(5):372-377.
[32] WANG H C,LIN Y T,HUANG C C,et al.Effects of Respiratory Muscle Training on Baroreflex Sensitivity,Respiratory Function, and Serum Oxidative Stress in Acute Cervical Spinal Cord Injury[J].J Pers Med,2021,11(5):377.
[33] ZHANG X Y,YU W Y,TENG W J,et al.Effect of vocal respiratory training on respiratory function and respiratory neural plasticity in patients with cervical spinal cord injury: a randomized controlled trial[J].Neural Regeneration Research,2022,17(5):1065-1071.
[34] KIM C Y,LEE J S,KIM H D,et al.Short-term effects of respiratory muscle training combined with the abdominal drawing-in maneuver on the decreased pulmonary function of individuals with chronic spinal cord injury: a pilot randomized controlled trial[J].Spinal Cord Med,2017,40(1):17-25.
[35] DIMARCO A F,KOWALSKI K E.High frequency spinal cord stimulation of inspiratory muscles in dogs: a new method of inspiratory muscle pacing[J].J Appl Physiol,2009,107(3):662-669.
[36] KOWALSKI K E,ROMANIUK J R,BROSE S W,et al.High frequency spinal cord stimulation new method to restore cough[J].Respir Physiol Neurobiol,2016,232:54-56.
(收稿日期:2022-10-31) (本文編辑:陈韵)