Thrombocytopenia in chronic liver disease: Physiopathology and new therapeutic strategies before invasive procedures
Paolo Gallo, Francesca Terracciani, Giulia Di Pasquale, Matteo Esposito,Antonio Picardi, Umberto Vespasiani-Gentilucci
Abstract Chronic liver disease is characterized by several hematological derangements resulting in a complex and barely rebalanced haemostatic environment. Thrombocytopenia is the most common abnormality observed in these patients and recent advances have led to researchers focus the attention on the multifactorial origin of thrombocytopenia and on the key role of thrombopoietin (TPO) in its physiopathology. Severe thrombocytopenia (platelet count < 50000/μL) complicates the management of patients with chronic liver disease by increasing the potential risk of bleeding for invasive procedures, which may be therefore delayed or canceled even if lifesaving. In the very last years, the development of new drugs which exceed the limits of the current standard of care (platelet transfusions, either immediately before or during the procedure) paves the way to a new scenario in the management of this population of patients. Novel agents, such as the TPOreceptor agonists avatrombopag and lusutrombopag, have been developed in order to increase platelet production as an alternative to platelet transfusions.These agents have demonstrated a good profile in terms of efficacy and safety and will hopefully allow reducing limitations and risks associated with platelet transfusion, without any delay in scheduled interventions. Altogether, it is expected that patients with chronic liver disease will be able to face invasive procedures with one more string in their bow.
Key Words: Thrombocytopenia; Chronic liver disease; Thrombopoietin agonists; Platelet transfusions; Avatrombopag; Lusutrombopag
lNTRODUCTlON
Thrombocytopenia, usually defined as any decrease in platelet count below the lower normal limit of 150000/μL, is the most common haematological abnormality in patients with chronic liver disease[1].Current data report a prevalence ranging from 6% to 78%, which progressively increases from patients with compensated to those with decompensated cirrhosis[2]. The clinical significance of mild(100000/μL-150000/μL) and moderate (50000/μL-100000/μL) thrombocytopenia is minimal and does not interfere with the regular clinical practice. Otherwise, severe thrombocytopenia (< 50000/μL) can be associated with many sequelae and could have a negative impact on the management of patients with advanced chronic liver disease.
PHYSlOPATHOLOGY OF THROMBOCYTOPENlA lN CHRONlC LlVER DlSEASE
In chronic liver disease, thrombocytopenia has been classically attributed to hypersplenism[1,3]. Over the last decades, however, advances in the understanding of thrombopoiesis have led to a wider and better understanding of its physiopathology. As a result, thrombocytopenia is considered a more complex and multifactorial process involving multiple different mechanisms. These are generically divided into those leading to decreased production or increased destruction of thrombocytes and splenic sequestration[1] (Figure 1).
Decreased platelet production
Decreased platelet production is a consequence of decreased production of thrombopoietin (TPO) and direct bone marrow suppression. Currently, the production of TPO is believed to play a pivotal role in thrombopoiesis. TPO is primarily produced in the liver and, after being secreted into the circulation, it binds to the surface of platelets and megakaryocytes through the c-MPL receptor[4]. TPO-receptor ligation activates a number of intracellular signalling pathwaysviaJanus kinase type 2 and tyrosine kinase 2[5], which ultimately lead to the differentiation of bone marrow stem cells into mature megakaryocytes and to the production of platelets which are released into the peripheral circulation[6]. Of note,after binding to its receptor, TPO is internalized and destroyed in order to reduce further platelet and megakaryocyte exposure[4]. Platelet production is therefore mainly regulated by platelet levels in the blood through a negative feedback circuit[1]. The role of a decreased hepatic production of TPO in the development of thrombocytopenia in chronic liver disease is supported by the immediate increase in TPO levels and platelet production after liver transplantation[7]. Animal models and human clinical studies have confirmed decreased expression ofTPOmRNA in liver tissue with the progression of cirrhosis[8], which is probably associated with specific regulatory mechanisms for the expression ofTPOgene and is not regulated by bone marrow[9]. Moreover, a correlation between reduced c-MPL expression and the progression of liver cirrhosis has been demonstrated and may play an additional role in the development of thrombocytopenia[10]. Some chronic liver diseases may also cause decreased platelet production through direct bone marrow suppression or toxicity, as observed during viral infection (particularly hepatitis C virus (HCV) infection[11], alcohol abuse[12], iron overload[12], and drug consumption[1,13]).
Increased platelet destruction

Figure 1 Pathophysiology of thrombocytopenia. TPO: Thrombopoietin.
Increased platelet destruction is a multifactorial process that may involve decreased levels of A disintegrin-like and metalloprotease with thrombospondin type 1 motif 13 (ADAMTS13), immunologically mediated platelet destruction, and bacterial activity. ADAMTS13 is a metalloproteinase produced by hepatic stellate cells, whose physiological role is to cleave large von Willebrand factor(vWF) multimers[14]. In cirrhosis, decreased levels and activity of ADAMTS13 drive the accumulation of vWF multimers, which mediates an enhancement of shear-stress induced platelet aggregation[14].Additionally, anti-platelet antibodies are a frequent finding in patients with liver cirrhosis, being detectable in up to 64% of cases[15]. The inverse relationship between platelet-associated immunoglobulin G (IgG) levels and platelet count evidences that immunologic destruction contributes to the genesis of thrombocytopenia at least in some chronic liver diseases[16]. Immune-mediated thrombocytopenia is most likely to occur in the course of autoimmune liver diseases (particularly primary biliary cholangitis) and HCV infection[1,17].
HCV can cause immune-mediated thrombocytopenia through multiple mechanisms[1]. First, it can be associated with idiopathic thrombocytopenic purpura (ITP), as supported by a prevalence of anti-HCV antibodies of approximately 10% in patients with ITP[18]. The virus can also directly bind to platelets interacting with multiple surface receptors, leading to the attachment of anti-HCV antibodies to platelets. This will ultimately determine either platelet phagocytosis by the reticuloendothelial system or alterations in the platelet membrane epitopes that induce the production of anti-platelet antibodies[19].Finally, HCV infection can be associated with the production of cryoglobulins, which can accelerate platelet clearance by the reticuloendothelial system[20]. Thrombocytopenia can be found in about 48%of patients with bacterial infection and sepsis[21], confirming that the inflammatory cascade plays a role in the development of thrombocytopenia. This is confirmed in the hospitalized cirrhotic population[22].In sepsis, thrombocytopenia is mainly dependent on the increased activation of the coagulative system,resulting in clot formation and platelet consumption[23].
Splenic sequestration
Hypersplenism has been classically considered the main determinant of thrombocytopenia during chronic liver disease[1,3], even after that many other physiopathologic mechanisms have been progressively identified. During chronic liver disease, the inception of portal hypertension causes a redistribution of splanchnic venous blood flow, ultimately responsible for congestion of the spleen and consequent enlargement of the organ, leading to a significant increase of the splenic pool of platelets[24]. Actually, hypersplenism is the clinical syndrome in which splenomegaly is associated with splenic hyperactivity,i.e.,a reduction in one or more peripheral blood cell types, in patients with an appropriate proliferative bone marrow response. This syndrome can be reverted with splenectomy[1,24].
COAGULOPATHY AND HAEMORRHAGlC RlSK ASSESSMENT lN CHRONlC LlVER DlSEASE
Chronic liver disease is characterized by alterations of the entire hemostatic system[25]. Thrombocytopenia is just one face of a wider coagulation disorder whose relevance is mirrored by the inclusion of coagulation indices in all functional and prognostic scores of liver disease[26]. Traditionally,coagulopathy in cirrhosis was considered as a bleeding diathesis disorder[27], alongside the well-known thrombocytopenia, and the impaired coagulation tests were perceived as indicators of hemorrhagic risk[28]. In the last decades, several studies led to significant changes in knowledge, with a renewed vision concerning the coagulopathy of liver cirrhosis. A new paradigm of a balanced,albeitprecarious,hemostatic state has emerged and the net effect is a rebalanced equilibrium[26,27], which can be easily disturbed by many different clinical events, alternatively leading to hemorrhagic as well as to thrombotic manifestations, with the latter being even more frequent indeed[27] (Figure 2).
It has been shown that the reduction in liver-derived pro-coagulant factors is counteracted by the concomitant decrease of the liver-derived anti-coagulant ones, especially protein C[28,29]. Thrombocytopenia and platelet abnormal function are offset by increased vWF and decreased ADAMTS13 levels. In cirrhosis, even if diminished in number, platelets are able to support normal thrombin generation at least until they are in the range 50-60000/mL, therefore assuring a normal primary hemostasis. This is possible thanks to the compensatory action of vWF and to the upregulation of intracellular activating signalling pathways[27], leading to an enhanced thrombocyte response. Furthermore, decreased clearance of tissue plasminogen activator and plasminogen activator inhibitor, and decreased synthesis of alpha 2-antiplasmin and thrombin activable fibrinolysis inhibitor are all factors contributing to hyperfibrinolysis. The latter is observed in up to 30% of patients with advanced liver disease[1],confirming a re-arrangement of the whole hemostatic system.
In cirrhotic patients, even though reduced in number, platelets are still able to ensure an adequate haemostatic function. Consequently, the sole platelet count is not able to predict bleeding risk in liver cirrhosis. Actually, for patients with cirrhosis undergoing invasive diagnostic or therapeutic procedures,the risk of procedure-related bleeding remains a clinical issue[30], and risk stratification is a great challenge. This is mainly due to the inaccuracy, in the context of cirrhosis, of the laboratory tests that are routinely used for the assessment of the hemocoagulative system[25,27,30]. Indeed, it is now well established that the standard clotting tests do not reflect the actual bleeding risk[30-32], and current evidence does not support prothrombin time (PT)/international normalized ratio (INR) as clinical targets[25,33]. Conversely, assessing platelet count and fibrinogen levels before high-risk procedures is recommended, as well as it is the pre-procedural correction of these parameters, having these laboratory parameters been proposed as more reliable indicators of the bleeding risk in patients with cirrhosis[34].
Moreover, many studies have shown that cirrhotic portal hypertension and kidney injury are more essential in determining the risk of bleeding[25,35]. As a matter of fact, renal failure can lead to platelet impairment resulting from reduced adhesive and aggregative capacitiesviaalterations of serotonin concentration, of calcium flow and of thromboxane metabolism[25]. Patient with cirrhosis can also develop accelerated intravascular coagulation and fibrinolysis, described as a bleeding entity similar to disseminated intravascular coagulation, but different for the imbalance between pro- and antifibrinolytic factors, resulting in hyper-fibrinolysis with an increased bleeding risk[35]. Despite all such evidence, most current guidelines still recommend correcting elevated PT/INR values through plasma transfusions, while tests capable of better capturing the hemostatic function of cirrhotic patients(thrombin generation tests, thromboelastography,etc.) are not readily available in everyday clinical practice[25].
NON-PHARMACOLOGlCAL TREATMENT OPTlONS FOR MANAGEMENT OF THROMBOCYTOPENlA
The management of thrombocytopenia in chronic liver disease has been a primary and challenging endpoint for decades. In the 1960s, surgical splenorenal shunts were performed with this purpose, but they were soon abandoned due to high mortality rates and the risk of liver decompensation[36]. Total and partial splenectomy were therefore developed. They gained popularity in the 1990s thanks to limited complication rates, mainly after the introduction of the laparoscopic technique. Later, less invasive techniques, namely, splenic artery embolization or spleen radiofrequency ablation, opened new scenarios[36].
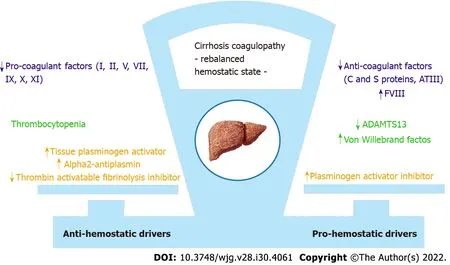
Figure 2 Pathophysiology of coagulopathy. ATIII: Antithrombin III; FVIII: Coagulation factor VIII; ADAMTS13: A disintegrin-like and metalloprotease with thrombospondin type 1 motif 13.
Splenectomy
In the past, open splenectomy has been considered among the strategies for treating thrombocytopenia.Actually, this procedure was associated with a high risk of bleeding and consequent hepatic decompensation, particularly following the open technique. For these reasons, subsequent studies supported the laparoscopic technique over open surgical splenectomy or the shunt techniques over splenectomy[37,38]. Overall, also with less invasive procedures, the rate of complications range from 2.5% to 17%, and the risk of portal and splenic vein thrombosis is elevated (about 10%)[39]. Altogether,due to their invasive nature and to the high risk of complications, these strategies are restricted to rare and specific cases, while they have been virtually abandoned in the ordinary clinical practice.
Splenic artery embolization
Splenic artery embolization has been introduced since the 1970s as an alternative to splenectomy in surgically unfit patients. For the increased risk of developing splenic abscesses after total embolization,partial splenic embolization has become the preferred option for candidate patients[40], with a lower risk of complications, sepsis and mortality compared to total splenectomy[36,41]. Unfortunately, the extent of the beneficial effect on platelet count depends on the amount of the splenic mass embolized,which is proportional to the complications observed.
Radiofrequency ablation of the spleen
Radiofrequency ablation of the spleen is a minimally invasive procedure with promising results in patients with cirrhosis and severe thrombocytopenia[36]. The main benefits of this minimally invasive procedure are cost-effectiveness and lower complication rates over other invasive procedures. The major side effects are hemorrhagic shock and intra-abdominal bleeding, while complications such as splenic abscess or rupture are not a concern with this procedure[42]. Besides, to date, more clinical trials with longer follow-up would be needed to estimate the effectiveness of this strategy.
Shunt procedures
Shunt procedures [portocaval shunt, splenorenal shunt, and transjugular intrahepatic portosystemic shunt (TIPS)] are other possible techniques which have been experimented in chronic liver disease. They are aimed at decreasing splenic congestion and, therefore, platelet sequestration[36]. To date, however,these approaches are not supported by available studies; indeed, there is an absence of clear benefits on the platelet number and well-known complications. Actually, the use of these procedures, in particular TIPS, is currently restricted to selected cases where the aim is not to increase platelet levels, but to control bleeding from oesophageal varices or to manage refractory ascites[43].
Platelet transfusion
Platelet transfusion has become the mainstay of treatment in patients with chronic liver disease and severe thrombocytopenia who require an invasive procedure[44]. The choice to transfuse platelets is variable and controversial, depending upon patient comorbidities and the risk of bleeding. Most data suggest that invasive procedures may be performed without a significantly increased risk of bleeding in patients with more than 50000/μL platelets, while there is less consensus about the risk in patients with a lower count, as reflected also in the latest guidelines and a recent retrospective study[45,46]. In a subanalysis of 2740 liver biopsies from the Hepatitis C Antiviral Long-term Treatment against Cirrhosis trial, there were only 16 bleeding events (0.6%), and the highest bleeding risk (5.3%) was recognized for platelet counts less than 60000/μL[47]. Conversely, in another study evaluating the safety of liver biopsies (177 patients), the frequency of bleeding in patients with a platelet count lower than 50000/μL was not significantly different from that in those with a normal platelet count, and the only independent risk factor for bleeding was an underlying malignancy[32].
Guidelines vary as to the threshold below which periprocedural bleeding risk justifies intervening to treat thrombocytopenia; however, transfusions are more frequently indicated with a platelet threshold <50000/μL[48]. Although platelet transfusion has been the standard of care for correcting thrombocytopenia for a long time, relevant side effects limit its use. The most common issues include febrile or allergic reactions, risk of infection (even if very low), hemolysis, transfusion-related graft-versus-host disease, and alloimmunization[41,49]. Even the procedure of transfusion itself may be critical. Potential risks include errors in patient identification, in blood typing, and in cross-matching[50]. Concerning efficacy, platelet transfusions determine an overall modest increase in platelet count, without a significant impact on the risk of bleeding[51], and treatment effect has a limited duration. Moreover, up to 70% of patients receiving repeated platelet transfusions become refractory to subsequent ones.Finally, platelet transfusions are limited by donor supply, and the reduced availability may have a great impact on the management and clinical outcomes of these patients.
NEW THERAPEUTlC OPTlONS FOR THRMBOCYTOPENlA lN CHRONlC LlVER DlSEASE
Recent advances in understanding the physiopathology of thrombocytopenia in chronic liver disease,with the discovery of the central role of TPO in thrombocytopoiesis, has led to the development of many drugs with TPO activity.
Recombinant TPO and human cytokines
Two recombinant TPOs that stimulate platelet production in humans and showed potential promise were recombinant human TPO and pegylated recombinant megakaryocyte growth and development factor[52,53]. They have shown clinical benefits in clinical trials of haematological patients without safety concerns, but have been withdrawn from clinical development for the induction of neutralizing antibodies[53]. Similarly, the use of recombinant human cytokines was limited because of side effects and the occurrence of toxicities as observed after the subcutaneous injection of the recombinant human interleukin-1, approved by the Food and Drug Administration (FDA) for the treatment of the thrombocytopenia induced by chemotherapy for solid tumors, which can cause cardiovascular side effects and flu-like symptoms[54].
TPO agonists
Activation of thrombopoiesis through TPO receptor agonists is an alternative method to stimulate platelet production with the use of drugs, which are not homologous to endogenous TPO but activate the same receptor working on a different site. These drugs have been primarily investigated in patients with chronic ITP and subsequently in chronic liver disease for treating thrombocytopenia before invasive procedures. The effect of TPO agonists is mediated by the interaction with TPO receptors on megakaryocytes, specifically c-MPL ligand-mediated activation of Janus kinases and signal transducer and activator of transcription proteins and mitogen-activated protein kinase pathways[55].
Romiplostin: Romiplostin is a polypeptide linked to an IgG heavy-chain Fc molecule and has no amino acid sequence homology to endogenous TPO. It acts by competing with the same site of the TPOreceptor and activating intracellular transcriptional pathways aimed to increase platelet production[55].Due to a different molecular structure, its use has not been associated with antibodies reacting against endogenous TPO. This drug is administered subcutaneously once a week, but it is currently approved only for treatment of ITP when refractory to other drugs[54,56].
Indeed, most of the experience with romiplostin was derived from clinical studies in patients with refractory ITP[57], while only anecdotal case reports and small series involved patients with chronic liver disease[58-61]. A single-centre study in Egypt involved 35 patients with HCV-related cirrhosis and severe thrombocytopenia who required elective surgery[60]. Patients received romiplostin once weekly for a maximum of 4 wk. The primary endpoint - achieving a threshold of platelet count of 70000/μL -was reached in 94% of patients, and 20% of them had maintained a count > 50000/μL 3 mo after the last injection. Headache was reported as the only adverse event. In another single centre, prospective,randomized, double-blind study, 65 subjects with chronic liver disease and thrombocytopenia (less than 60000/μL) undergoing percutaneous liver biopsy received a TPO agonist or platelet transfusion[61].Romiplostin determined significantly higher pre-biopsy and post-biopsy platelet counts compared to eltrombopag and platelet transfusion, and it was cost-effective and safe.
Eltrombopag: Eltrombopag is an orally available, small non-peptide TPO mimetic molecule more largely studied for use in liver disease. Its binding to a specific human transmembrane domain of TPOreceptor induces proliferation and differentiation of megakaryocytes and precursor cells[62]. It is taken orally once daily and is approved for thrombocytopenia: (1) In chronic ITP refractory to other treatments; (2) In HCV chronic hepatitis candidates for treatment with interferon-based regimens; and(3) In patients with severe aplastic anaemia[63].
Eltrombopag safely increased platelet number in patients with cirrhosis and HCV infection[64]. In a phase II multicentre randomized trial, eltrombopag was effective in increasing platelet count to more than 100000/μL at week 4 in 75%-95% of patients, compared to 0% of patients in the placebo group.Consequently, these patients were significantly more likely to initiate and complete 12 wk of antiviral treatment with respect to those on placebo (36%-65%vs6%). In a phase II trial in Japan on 38 patients with chronic liver disease, eltrombopag increased platelet count in a dose-dependent manner[65].
The most recently published data in chronic liver disease are derived from the Eltrombopag Evaluated for Its Ability to Overcome Thrombocytopenia and Enable Procedures study, a phase 3 double-blind, placebo controlled trial that assessed the utility of this drug to increase platelet count and reduce the need for transfusion in patients undergoing elective procedures[66]. In this trial, 86% of patients recruited had liver cirrhosis with a platelet count less than 50000/μL. Patients were randomized to receive 75 mg eltrombopag daily or placebo in the 2 wk preceding the invasive procedure performed within 5 d from the last dose. Primary endpoint was the number of subjects who did not require a platelet transfusion before, during, and up to 7 d after the procedure. This was achieved in 72%(104/145) of subjects who received eltrombopag, compared to 19% (28/147) in the placebo group (P<0.001). However, this study was prematurely terminated since six patients in the treatment group developed thrombotic events (2 patients in placebo, odds ratio for eltrombopag 3.04, 95% confidence interval: 0.62-14.82).Post-hocanalysis suggested an association of platelet count > 200000/μL with the occurrence of portal vein thrombosis[66].
The other two international phase III trials included patients with chronic hepatitis C and platelet counts less than 75000/μL[67]. Eltrombopag to Initiate and Maintain Interferon Antiviral Treatment to Benefit Subjects with Hepatitic C-Related Liver Disease (ENABLE)-1 and ENABLE-2 assessed the ability of eltrombopag to increase platelet count and, so, allow subjects to initiate and maintain antiviral treatment with pegylated interferon and ribavirin. In both trials, significantly more patients on eltrombopag achieved a sustained virological response at 24 wk of antiviral therapy, with similar adverse events. However, the absolute benefit over placebo was less than 10% and the use of this drug was associated with an increased risk of hepatic decompensation (10%vs5% placebo) and thromboembolic events (3%vs1% placebo). The most frequent adverse events reported were anaemia,pyrexia, and neutropenia.
Avatrombopag: Avatrombopag is an orally available drug that has a similar mode of action to eltrombopag, and it does not compete with endogenous TPO for its receptor site-binding. It is taken once daily with food for 5 d a week, with the dose adjusted according to baseline platelet count.Differently from eltrombopag, it exhibits significant drug-drug interactions based on the cytochrome P4502C9 (CYP2C9) and CYP3A cytochrome systems[68]. In a phase II study, 130 patients with chronic liver disease and platelet count less than 60000/μL received two different formulations of the drug 1 wk prior to an elective invasive procedure, and both groups of avatrombopag-treated patients achieved the primary endpoint of an platelet increase of > 20000/μL from baseline, and to > 50000/μL, at least once during the treatment days 4-8.
After that, avatrombopag was approved by the FDA in 2018 and the European Medicines Agency(EMA) in 2019 for the treatment of severe thrombocytopenia in patients with chronic liver disease undergoing invasive procedures, with the recommendation to take it 10-13 d before the procedure scheduled within 5-8 d from the last dose administration[69]. The safety and efficacy were evaluated in two pivotal randomized phase 3 studies[69]. ADAPT-1 and ADAPT-2 (Table 1) randomized 430 patients with cirrhosis and severe thrombocytopenia undergoing scheduled procedures to receive avatrombopag at different doses (according to platelet baseline count) or placebo for 5 d. The primary endpoint was the need for platelet transfusion or rescue procedures for bleeding in the 7 d after the procedures[70].Significantly more patients met this endpoint in avatrombopag groups: In ADAPT-1, 65.6% and 88.1%compared to 22.9% and 38.2% of patients receiving placebo; in ADAPT-2, 68.6% and 87.9% compared to 34.9% and 33.3% (P< 0.001 for both) (Figure 3). Overall, the safety profile was similar to placebo and the most frequent adverse events were nausea, fatigue, abdominal pain, pyrexia, and headache. Serious adverse events occurred in 16%-19% of patients with avatrombopag and 6%-14% of those with placebo,including one patient who developed portal vein thrombosis during post-treatment follow-up. Finally,the safety and efficacy of avatrombopag were recently confirmed in a real-world setting, where cirrhotic patients mainly undergoing esophageal varices band ligation received the drug without requiring platelet transfusion, and with a good profile of adverse events[71,72].
Lusutrombopag: Lusutrombopag is an orally administered synthetic small molecule that acts as an agonist of human TPO, activating the signal transduction pathways to upregulate platelet production.Earlier studies have demonstrated that lusutrombopag raises platelet count and is a manageable drugthat does not require food restrictions, and has no clinically significant drug-drug interactions[73,74].Furthermore, it has demonstrated a dose-proportional pharmacokinetic with no clinically significant differences in the pharmacokinetic grounded on age, liver function (Child-Pugh classes A and B), and renal function (creatinine clearance greater than 30 mL/min)[75]. It is primarily metabolized by CPY4 enzymes, including CYP4A11, and it is mainly excreted by the faecal route (83% of dose). Moreover, it has a low potential to inhibit or induce transporter systems and CYP enzymes[73]. The recommended dose of the drug is 3 mg once daily for 7 d, beginning 8-14 d prior to the scheduled procedure.

Table 1 ADAPT 1-2 key characteristics

Figure 3 Overview of primary endpoints of phase 3 studies (ADAPT-1, ADAPT-2, L-PLUS 1, and L-PLUS 2). aP ≤ 0.0001.
Lusutrombopag was approved in Japan in 2015 for use in patients with thrombocytopenia and chronic liver disease who needed invasive procedures and received a positive opinion from the EMA Committee for Medicinal Products for Human Use in 2018[76]. The approval of this drug was based on the results of Lusutrombopag for the Treatment of Thrombocytopenia in Patients with Chronic Liver Disease Undergoing Invasive Procedures trial (L-PLUS-1), a phase 3 double-blind study, carried out in Japan with 96 patients with chronic liver disease and severe thrombocytopenia (platelet count <50000/μL) undergoing invasive procedures[77] (Table 2). In this study, the proportion of patients that did not require pre-operative platelet transfusions was significantly greater in the lusutrombopag groupvsplacebo (79.2 %vs12.5%, respectively,P< 0.0001) (Figure 3). The median platelet count reached more than 50000/μL after 5 d in the drug group, with the greatest value observed after a mean of 13.4 d.Moreover, no significant concerns were raised in this study, and no significant adverse drug reactions were observed.

Table 2 Lusutrombopag for the Treatment of Thrombocytopenia in Patients with Chronic Liver Disease Undergoing lnvasive Procedures trial 1-2 key characteristics
The safety and efficacy of this drug were confirmed in a larger study, the L-PLUS-2[78]: 215 patients with chronic liver disease and a platelet count < 50000/μL were randomly assigned to once-daily lusutrombopag at a dosage of 3 mg or placebo for ≤ 7 d before an invasive procedure. The procedure was performed within 7 d after the last dose. In the intention to treat analysis, significantly more patients in the lusutrombopag group (64.8%) met this endpoint compared with placebo (29%,P< 0001).This percentage was greater in the per-protocol analysis, with the endpoint reached in 72.5% of patients in the active drug groupvs20% in the placebo group (P< 0.0001). The median duration of the achievement of a target of platelet count > 50000/μL was 19.2 d in the lusutrombopag groupvs0 d for the patients who received placebo. Moreover, the median maximum change in platelets from baseline was over 4 times higher for patients treated with the active drug, who did not receive platelet transfusions, compared with patients who did receive transfusions (45000vs11000/μL)[78]. Finally,47.7% of patients in the lusutrombopag group and 48.6% in the placebo group had at least one adverse event. These side effects were mainly mild or moderate in severity and the most common were headache, abdominal pain, fatigue, peripheral edema, and nausea. There were only three mild bleeding events in three patients in the lusutrombopag group (2.8%)vsseven bleeding events (4 moderate and 1 severe; 5.6%) with placebo. Only three thromboembolic events were recorded (1 in the lusutrombopag group), which were not related to platelet count.
The first real-life study in Japan enrolled 25 patients with cirrhosis, who were treated with lusutrombopag prior to invasive treatments (radiofrequency ablation, transarterial chemoembolization,and endoscopic variceal ligation)[79]. In this group, platelet count significantly increased compared with baseline (82000 ± 26000vs41000 ± 11000 /μL). The proportion of patients who needed platelet transfusions before procedures was very low (only 4, 16%) compared to those not treated with lusutrombopag (69 patients, 54%). Moreover, platelet counts after treatment and before invasive procedures were lower in patients with a count less than 30000/μL, and this cut-off, together with a spleen index > 40 cm2, was predictive of a lower response rate to the drug[80]. This was probably due to a larger number of platelets sequestered in the spleen in this subgroup of patients. No haemorrhagic complications were observed, and only a single case of recurrent portal vein thrombosis was observed and successfully treated.
Another real-life setting retrospective study was carried out in patients with chronic liver disease and severe thrombocytopenia. In this study[81], 74.2% of patients who received treatment did not require platelet transfusion before invasive procedures. This percentage increased to 82.1% of treatments if patients who repeated lusutrombopag use more times were included, thus demonstrating the efficacy of repeated use of the drug. Furthermore, only one serious adverse event was observed during/after treatment,i.e.,one case of portal thrombosis disappearing after anticoagulation. Notably, this study confirmed that a lower platelet count at baseline was a predictive factor for failure to reach the target of> 50000/μL platelets. Indeed, median basal platelet count was higher in respondersvsnon-responders(38000/μLvs12000/μL).
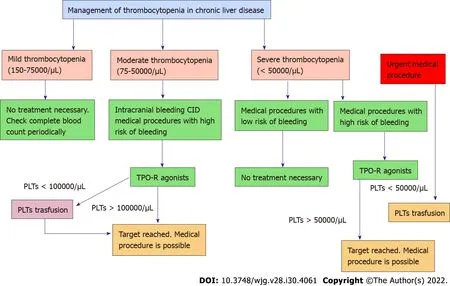
Figure 4 Operative flow chart for management of thrombocytopenia in chronic liver disease. TPO-R: Thrombopoietin receptor; PLTs: Platelets;CID: Disseminated intravascular coagulation.
Moreover, the safety and efficacy of repeated use of lusutrombopag have been confirmed also in 66 patients who underwent radiofrequency ablation for recurrence of hepatocellular carcinoma[82]. Later,others reports have confirmed the efficacy and safety of lusutrombopag in real life in patients with thrombocytopenia due to chronic liver disease. In a case report, Kanekoet al[83] showed lusutrombopag to be a successful substitute for platelet transfusion in a patient with chronic liver disease undergoing endoscopic spinal surgery. Kawataet al[84] reported three patients treated with lusutrombopag before tooth extraction: Platelet count increased, preventing the need for transfusion in two of three cases.There were no adverse events. In addition, the efficacy and safety of the drug have been confirmed in a retrospective Japanese study based on hospital administrative databases. Here the incidence of bleeding events was lower in the lusutrombopag group than in the platelet transfusion group (3.7%vs8.2%,P<0.001), with a consequently lower average medical cost[85]. Finally, real-world data for adverse events(spontaneously reported by healthcare professionals and consumers in a database including about 4000 patients exposed to lusutrombopag from December 2015 to April 2018) confirm the efficacy and the safety of the drug (93% of patients did not require pre-procedural platelet transfusion; 1.2% of serious adverse events, with 0.4% cases of portal vein thrombosis)[86].
CONCLUSlON
Thrombocytopenia represents one of the main coagulation disorders in patients with chronic liver disease. Recent awareness in its physiopathology shed light on the central role of TPO. The development of TPO receptor agonists has opened a new scenario in the management of patients with liver disease who need invasive procedures (Figure 4). Avatrombopag and lusutrombopag have demonstrated their efficacy and safety in increasing platelet count without an increased risk of thrombosis. Moreover, they reduce the overall clinical risk associated with platelet transfusion without any delay in the management of these patients. With careful logistical planning and coordination between drug availability and medical procedures, patients with chronic liver disease and severe thrombocytopenia should now be able to undergo more easily invasive procedures.
FOOTNOTES
Author contributions:Vespasiani-Gentilucci U and Gallo P conceived the study; Gallo P, Terracciani F, Di Pasquale G, and Esposito M wrote the manuscript; Picardi A and Vespasiani-Gentilucci U helped in drafting and revising the manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORClD number:Paolo Gallo 0000-0001-8292-1134; Francesca Terracciani 0000-0002-4778-4194; Giulia Di Pasquale 0000-0001-8872-6815; Matteo Esposito 0000-0003-0609-6333; Antonio Picardi 0000-0002-0230-218X; Umberto Vespasiani-Gentilucci 0000-0002-1138-1967.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Wang JJ
 World Journal of Gastroenterology2022年30期
World Journal of Gastroenterology2022年30期
- World Journal of Gastroenterology的其它文章
- Role of one-step nucleic acid amplification in colorectal cancer lymph node metastases detection
- Current perspectives on the role of liver transplantation for Langerhans cell histiocytosis: A narrative review
- Gut microbiota, inflammatory bowel disease and colorectal cancer
- P2X7 receptor blockade decreases inflammation, apoptosis, and enteric neuron loss during Clostridioides difficile toxin A-induced ileitis in mice
- Serological profiling of Crohn’s disease and ulcerative colitis patients reveals anti-microbial antibody signatures
- Trends in medication use and treatment patterns in Chinese patients with inflammatory bowel disease
