Intracranial hemangiopericytoma with right-sided aortic arch:a case report and summary of experience
Tong Ren, Jun-Feng Zhao, Xiang-Yu Li, Wen-Xiao Wu, Tian-Lin Guo, Qun Yu, Xun Wang*
Abstract Hemangiopericytoma is clinically rare and easily confused with meningioma.Right-sided aortic arch is also a rare disease of congenital cardiovascular variability.The intracranial hemangiopericytoma associated with the right-sided aortic arch has not been reported in the literature.We are here to register a case of right aortic arch concurrent with intracranial hemangiopericytoma;the patient was initially thought to be a simple meningioma, but he was eventually diagnosed as a hemangiopericytoma with right aortic arch and multiple intracranial vascular stenosis and malformation.Whether there was a genetic correlation between the two provides a potential research direction for us.Therefore,the diagnosis and treatment of some rare diseases should be a more comprehensive analysis and evaluation.Adequate examination and accurate diagnosis are crucial,which will directly affect the efficacy of surgery and the prognosis of patients.
Keywords:hemangiopericytoma;right-sided aortic arch;examination;diagnosis;surgery
Introduction
Hemangiopericytoma (HPC) is a mesenchymal tumor generally occurring in adults and originating from the pericytes.HPC is clinically rare and easily confused with meningioma [1-2].Right-sided aortic arch (RAA) is also a rare disease of congenital cardiovascular variability with an incidence of only 0.1% [3].RAA is often associated with many secondary vascular mutations.However, the intracranial hemangiopericytoma associated with the right-sided aortic arch has not been reported in the literature.We are here to report a case of right aortic arch concurrent with intracranial hemangiopericytoma: the patient was initially thought to be a simple meningioma, but was eventually diagnosed as a hemangiopericytoma with right aortic arch and multiple intracranial vascular stenosis and malformation.It is very important to identify HPC from meningioma, make a correct therapeutic plan and have an appropriate prediction of prognosis.The diagnostic and therapeutic challenges strongly emphasize the importance of this topic for future investigations.
Case presentation
The patient was a 34-year-old female who has been admitted with reduced binocular vision accompanied by headache and dizziness for three months and has no prior history of the disease.The patient began to have headaches and dizziness three months ago, which appeared intermittently.Since the patient had just completed pregnancy and combined with high blood pressure (Maximum blood pressure: 150/100 mmHg), another hospital initially considered giving antihypertensive treatment for pregnancy combined with hypertension.Due to the progressive aggravation of the symptoms, combined with impaired binocular vision, nausea, vomiting, walking instability and other symptoms.The patient went to our hospital for further diagnosis and treatment.Our CT showed cerebellar space-occupying lesions combined with mild hydrocephalus.Physical examination: Conscious, bilateral pupil diameter was about 4.5 mm, sensitivity to light reflection, papilledema,limb muscle strength was level 5.
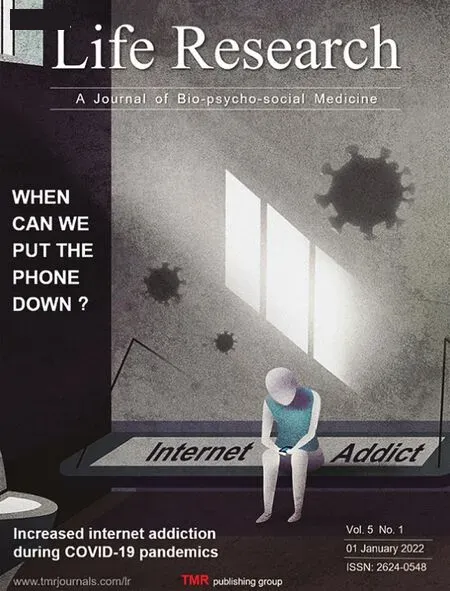
Blood routine examination, biochemical routine examination,hepatorenal function were no abnormalities.Enhanced MRI indicates that there was a space-occupying lesion in the right cerebellum, growth in the tentorial lobes of the cerebellum.The boundary is clear and the enhancement is obvious.The tumor was about 3.5×2.9×4.3 cm,compressing the fourth ventricle and causing a dilation of the bilateral cerebral ventricles.According to this, a high possibility of meningioma was considered (Figure 1).At this moment, we all considered that the patients were simple meningioma complicated with hydrocephalus.The CTA found that the right aortic arch and left sub-clavicular artery were thickened.Second, there was an irregular tumor in the right cerebellum and left cerebellar vein malformation.At last, the left anterior cerebral artery A1 and the vertebral artery were thin.Further DSA revealed that the tumor was abnormally rich in blood supply, and the right posterior cerebral artery branch was more likely to be the blood supply artery for the tumor (Figure 2).At this time, we did not give much consideration to the cause of the tumor.The initial diagnosis was still in favor of meningioma, so there was no tumor embolization performed.Postcranial fossa occupying resection was performed under general anesthesia.Considering that the patient had obstructive hydrocephalus and high intracranial pressure, we performed lateral ventricle puncture and extraventricular drainage during the operation to slowly extract cerebrospinal fluid to reduce intracranial pressure.The bone flap was removed, and brain tissue was separated.The tumor was exposed above and below the tentorium cerebellum, which showed dark purple, soft texture, rich blood circulation, difficulty in hemostasis, and large blood loss.Therefore, the operation time was far beyond the expectation.The tumor was completely removed from the subtentorial and supratentorial parts respectively(Figure 3).The patient recovered well after the operation.Due to the Space Occupying Effect of tumor has resolved, the symptoms of headache and dizziness were improved and the vision gradually recovered.
Postoperative pathology indicated hemangiopericytoma.Immunohistochemical: CD34 (+), CK (-), EMA (-), Ki67 (3-5%), S100 (-),Vim(+)(Figure 4).
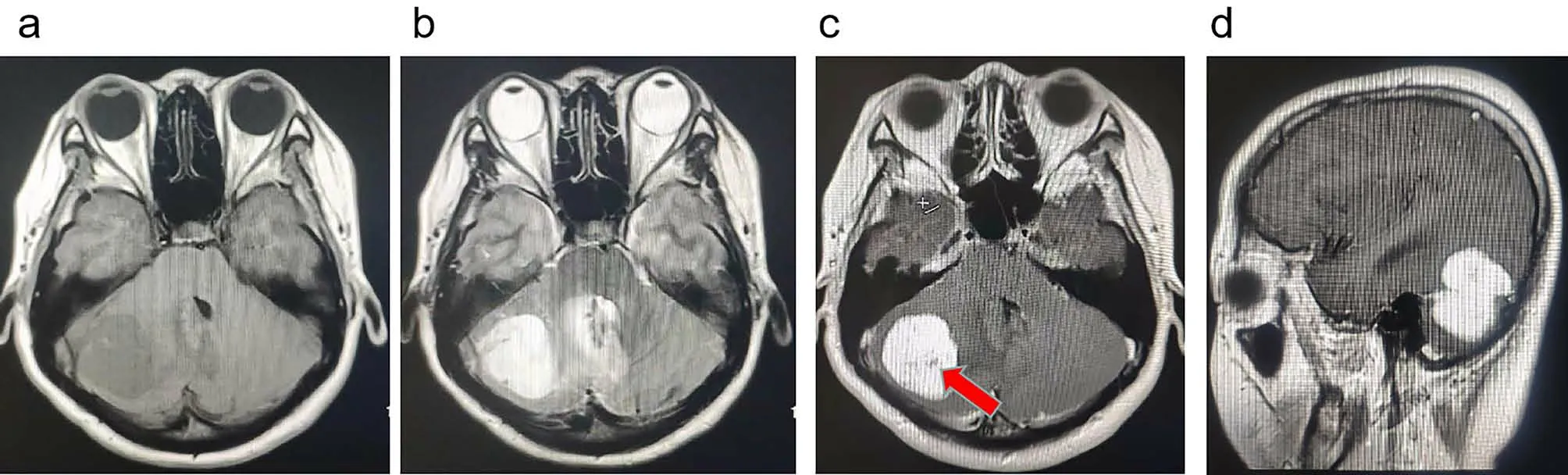
Figure 1.Enhanced MRI indicated that there was a space-occupying lesion in the right cerebellum.(a)Axial T1-weighted image showed an isointense tumor in the right cerebellum.(b)Axial T2-weighted image showed that the tumor was hyperintense.(c)The tumor had enhanced and showed a flow void effect(red arrow)in the part of the tumor.(d)The tumor had enhanced in sagittal MRI.
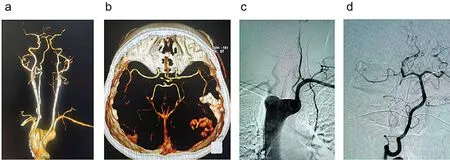
Figure 2.Artery imaging.(a)The CTA found that the right aortic arch and left sub-clavicular artery were thickened.(b)The CTA found that an irregular tumor in the right cerebellum and left cerebellar vein malformation.(c)DSA showed that the right aortic arch.(d)DSA showed that the right posterior cerebral artery branch was more likely to be the blood supply arteries for the tumor.
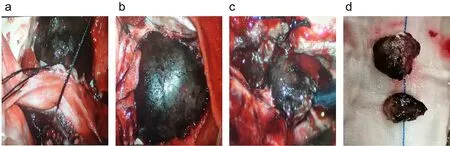
Figure 3.The tumor in operation.(a)The tumor was bestriding above and below the tentorium cerebellum.(b)The tumor showed dark purple.(c)The tumor showed soft texture and rich blood circulation.(d)The tumor was completely removed from the subtentorial and supratentorial parts respectively.
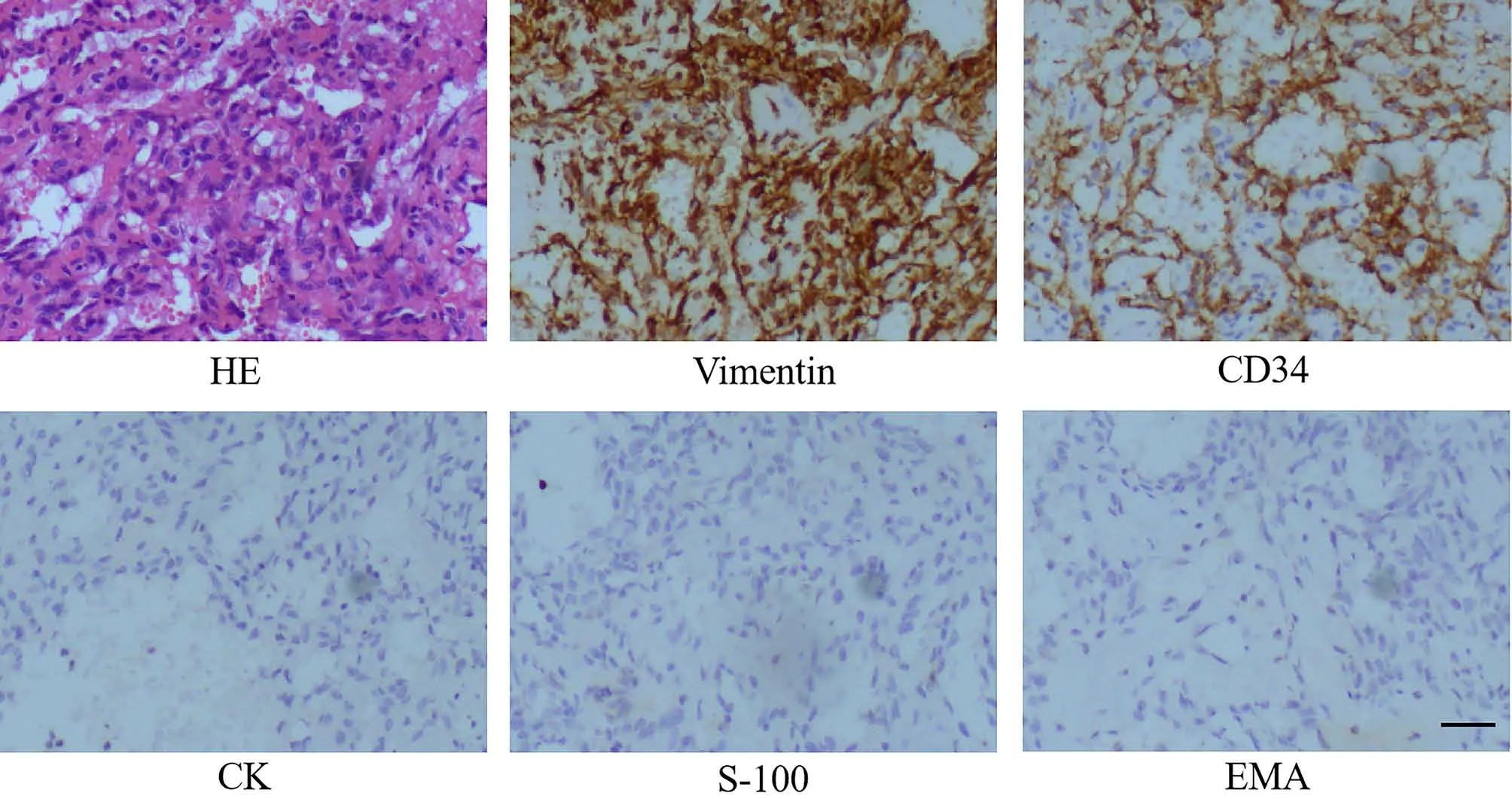
Figure 4.Histopathological examination of the resected tissue was taken for biopsy after the operation (scale bar, 50 μm).Immunohistochemical analysis further indicated that the tumor was immunopositive for Vimentin(+),CD34(+),CK(-),S-100(-),and EMA(-).
Follow-Up
After 3 months of follow-up, the patient showed good clinical condition without obvious symptoms of headache, dizziness, nausea and vomiting.Instead, steady walking, improved vision compared with preoperative,normal blood pressure and no need for antihypertensive treatment were present in the follow-up as well.No obvious recurrence was observed in the imaging examination.
Discussion
HPC is a rare intracranial tumor, and the differential diagnosis of HPC and meningioma is likely to be confused.First, the common sites of HPC and meningioma are very similar in that both tend to occur in the brain’s convex surface, next to the falx cerebri and basis cranii.Both HPC and meningioma have an abundant blood supply and the MRI enhancement shows a significant enhancement effect on tumor entities, which is more difficult to distinguish when meningiomas tend to be malignant.Accurate diagnosis can make the most suitable treatment and surgical method,which directly affects the success rate of surgery and the prognosis of patients.Currently, some clinical identification methods have been summarized, such as tumor shape of HPC is primarily lobulated change and meningioma edge is relatively smooth, lobulated rare, mostly circular.In terms of imaging findings, cystic degeneration and necrosis of HPC were common, and T2WI signals and DWI signals of HPC were usually mixed.The signal intensity of DWI and the apparent diffusion coefficient within the tumor is one of the important factors for differentiating HPC from meningioma [4].HPC mainly presents high signal changes on DWI,while meningioma mainly presents low signal or iso-intense signal changes.At the same time, the blood vessels of HPC were more abundant than those of meningioma, and the blood vessels in HPC were often left empty shadows [2,5].Previously, patients with simple meningioma are often directly treated with enhanced MRI only.In this case, hemostasis and separation difficulties occurred during the operation, which greatly exceeded our expectations.Due to inaccurate diagnosis can not make the best treatment, increase the difficulty of operation, and affect the prognosis of patients, after this case, we learned the following experiences:(1) More comprehensive and perfect preoperative examination, such as adding MRI-DWI images.(2) We should consider the possibility of partial embolization of the tumor’s supplying artery before the surgery.(3) The case of rare diseases should be fully considered, especially in patients with congenital vascular dysplasia.RAA is a congenital aortic arch variation,which can exist in isolation or can be combined with intracardiac and extracardiac malformations [6], such as ventricular septal defect, aortic straddle, endocardial pad defect, permanent left superior vena cava,transposition of the great artery, tetralogy of Fallot, cleft lip and palate,nasal bone dysplasia, etc.However, there are a few reports on RAA complicated with neurosurgical diseases.In addition to RAA and HPC,this patient also had multiple intracranial vascular abnormalities.First,RAA leads to intracranial hemodynamic changes, which may cause multiple variations of intracranial blood vessels in patients, such as vascular thinning and vascular malformation.It has been reported that the pathogenesis of RAA is related to the chromosomal 22q11.2 microdeletion to some degree [7-8].We also found that the pathogenesis of HPC is related to the complementary translocation of 13q22 and 22q11, which may involve the oncogene and fragile site of chromosome 22 [9].Many reciprocal translocations in tumors are difficult to detect by routine cytogenetic analysis, but the application of techniques such as spectral karyotyping, FISH, and chromosome microdissection/reverse in situ hybridization may yet reveal shared specific translocations in HPC[10].Whether there is a genetic correlation between the two provides a potential research direction for us on if patients with RAA should be highly alert to the possibility of coexistence of intracranial lesions.
In conclusion, the diagnosis and treatment of some rare diseases should be a more comprehensive analysis and evaluation.Hence, perfect examination and accurate diagnosis are crucial, directly affecting the efficacy of surgery and the prognosis of patients.
- Life Research的其它文章
- Increased internet addiction during COVID-19 pandemics
- Advances of biodegradable magnesium-based implants for orthopaedics
- Low expression of novel biomarker RCSD1 predicts poor prognosis of lung adenocarcinoma
- Graft rejection after deep anterior lamellar keratoplasty in fellow eye in macular corneal dystrophy:a case report
- Utility of convalescent plasma for addressing the COVID-19 infection:brief review and case reports
- Molecular mechanism of different viruses associated with autoimmunity