Low expression of novel biomarker RCSD1 predicts poor prognosis of lung adenocarcinoma
Gui-Jin Fang, Sheng-Ming Liu*
Abstract Lung adenocarcinoma (LUAD) is a highly malignant lung tumor.In patients with acute lymphoblastic leukemia, the RCSD domain containing 1(RCSD1) gene is translocated and fused with the ABL1 gene to form the RCSD1-ABL1 fusion gene, resulting in high chromosome instability.However, the role of RCDS1 in lung adenocarcinoma remains unclear.This study aimed to evaluate the relationship between the expression of RCSD1 in lung adenocarcinoma, clinical prognosis, biological processes involved, and immune infiltration.The lung cancer explorer database was used to conduct a meta-analysis on the study of RCSD1 in lung adenocarcinoma.We downloaded the sequencing data of the RCSD1 gene in lung adenocarcinoma for prognostic analysis.A receiver operating characteristic(ROC)curve was drawn to assess the diagnostic value of RCSD1 expression in LUAD.Using R language,univariate and multivariate COX regression analysis of the clinical data of RCSD1 in lung adenocarcinoma was carried out.The molecular biological process of RCSD1 in lung adenocarcinoma and the relationship between RCSD1 expression level and immune infiltration were analyzed.Different from the normal lung tissue,the expression level of RCSD1 in lung adenocarcinoma is decreased.Low expression of RCSD1 is related to different clinicopathological characteristics.RCSD1 participates in multiple immune-related pathways and is positively correlated with tumor immune infiltrating cells,immune phenotypes,and immune checkpoint expression.We reveal for the first time the prognostic role of RCSD1 in lung adenocarcinoma.Its mechanism of action may be involved in regulating immune infiltration and can serve as a potential biomarker of lung adenocarcinoma.
Keywords:lung adenocarcinoma;RCSD1;immune infiltration;survival analysis
Introduction
Lung cancer is the world’s most common cancer, with 1.8 million deaths due to lung cancer each year [1].This brings huge a financial burden to the world.The incidence of lung cancer is closely related to many risk factors such as ionizing radiation [2], smoking [3], air pollution [4], and so on.About 85% of lung cancers are non-small cell lung cancer(NSCLC) [5], of which the most common pathological type is lung adenocarcinoma.Some patients with lung adenocarcinoma were already in the advanced stage when they first got clinical treatment.Thus, early intervention is particularly essential for the pathogenic mechanism of lung adenocarcinoma.After decades of research, targeted therapy and immunotherapy have gradually become one of the main treatments [6].Immune cells in the tumor microenvironment (TME) contribute to the development of lung adenocarcinoma and affect the survival time of patients [7].The sequencing of tumor suppressor genes and oncogenes provides a basis for the precise treatment of patients with lung adenocarcinoma, but there are still many immune-related genes that may affect TME that have not yet been discovered.Immune checkpoints such as PDCD1, CD274, and CTLA4 have been confirmed to be related to the survival of patients with lung adenocarcinoma.Immune checkpoint inhibitors have been used in immunotherapy and have achieved good results [7].ABL1 is a common immune-related pathogenic gene in leukemia and fused with the BCR gene to form the BCR-ABL1 fusion gene to promote the progression of leukemia.The fusion of the RCSD1 gene with the ABL1 gene to form the RCSD1-ABL1 fusion gene was found in a few patients with acute lymphoblastic leukemia [8], suggesting that the RCSD1 gene may be involved in the process related to tumor immune regulation.The human lung cancer database (HLungDB) is a comprehensive portal focusing on lung cancer gene research [9], and we identified RCSD1 as a potential driver gene for lung adenocarcinoma from the HLungDB database.Because RCSD1 may be involved in tumor immune regulation in leukemia, it is of interest to investigate whether the RCSD1 gene affects the immune microenvironment of lung adenocarcinoma and the relationship between RCSD1 and immune infiltration.In this study, we initially investigated the prognostic role of RCSD1 in lung adenocarcinoma and its relationship with immune infiltration.The expression of RCSD1 in lung cancer was positively correlated with a variety of immune cells and immune checkpoints, and low expression of RCSD1 could be used as a potential prognostic marker in lung adenocarcinoma.
Methods
Expression analysis and clinicopathologic features
Lung cancer explorer (LCE) is a public website covering lung cancer gene expression and clinical data from 23 gene platforms [10].First, a metaanalysis of RCSD1 mRNA expression in LUAD was performed through the lung cancer explorer website and a forest map was drawn.Then, we downloaded RNA sequencing (RNA-seq) and clinicopathological data(including age, gender, TNM stage, primary therapy outcome,pathological stage) of 594 LUAD patients from The Cancer Genome Atlas(TCGA)database and performed comprehensive bioinformatics analysis.
Survival analysis and ROC curve
TCGA Pan-Cancer Clinical Data Resource (TCGA-CDR) is a standardized data set containing the four main clinical outcomes of tumors developed based on the TCGA database [11].We downloaded the TCGA-CDR data to evaluate the association of RCSD1 expression with overall survival (OS) in LUAD patients.The expression level was divided by 50%.Receiver operating characteristic (ROC) curve is a common tool for judging the possibility of a certain disease in the body based on markers [12].Therefore, we plotted the ROC curve of RCSD1 in LUAD patients to judge the diagnostic value of RCSD1.
Univariate and multivariate cox analysis
Survival data of LUAD patients were analyzed using the “survival” R package.The prognostic variables of lung adenocarcinoma were determined by univariate Cox regression analysis and multivariate Cox analysis.
Biological function analysis of RCSD1 co-expression gene
With |corpearson|>0.7 and p<0.05 as the thresholds, 140 genes coexpressed positively with RCSD1 were screened out.We performed gene ontology (GO) annotation analysis and Kyoto encyclopedia of genes and genomes (KEGG) pathway analysis on these co-expressed genes.GO annotation analysis covers biological processes (BP), molecular functions(MF),and cellular components(CC).
The relationship of RCSD1 mRNA expression and immune infiltra‐tion
Single-sample gene-set enrichment analysis (ssGSEA) is built into Gene Set Variation Analysis (GSVA) [13] and applied to analyze the relationship between gene expression and immune infiltration [14].We used ssGSEA to analyze the immune infiltration of RCSD1 and 24 kinds of immune cells.TISIDB (http://cis.hku.hk/TISIDB/index.php) integrates a lot of tumor immunological data and is often used to analyze the correlation between tumors and human immune characteristics [15].We log on to the TISIDB website to analyze the correlation between RCSD1 and different immune phenotypes (including immunostimulants,immunosuppressants, chemokines).We finally investigated the coexpression relationship between RCSD1 and immune checkpoints.
Results
Decreased expression of RCSD1 in LUAD
The forest plot (Fig.1) shows that, unlike normal lung tissue, a decrease in the expression of RCSD1 in lung adenocarcinoma tissue has been observed in multiple studies (P=1.3e-30, I2=19%).Data from the TCGA database indicated that in the unpaired t-test, RCSD1 expression was lower in 535 LUAD tissues than in 59 normal tissues (P<0.001;Fig.2a).The paired t-test was also lower in 57 LUAD tissues than in paired normal tissues (P<0.001; Fig.2b).Combining the research results of the lung cancer explorer database and TCGA database, RCSD1 expression is reduced in lung adenocarcinoma tissues.
Survival curve and ROC curve of RCSD1 expression
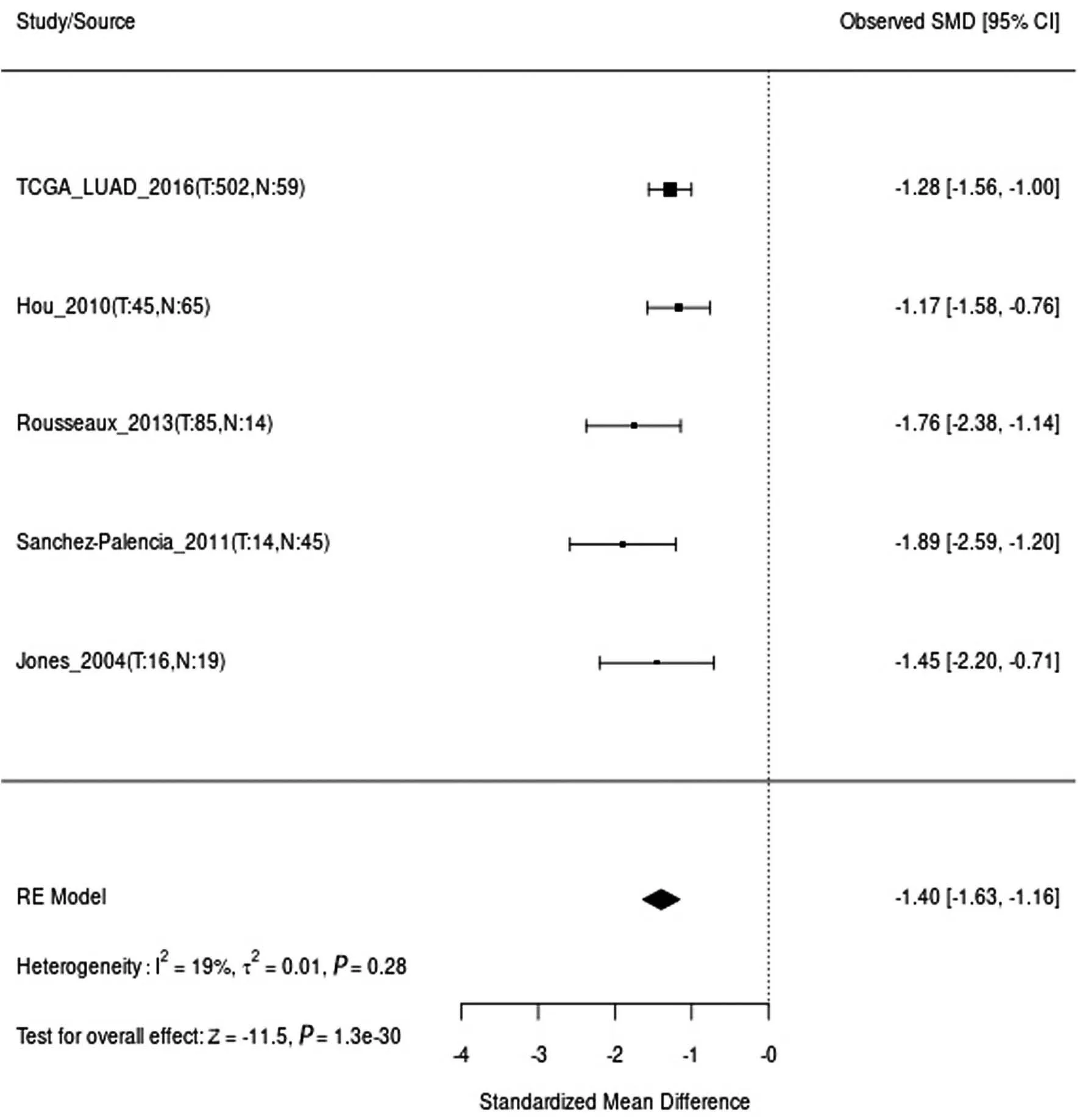
Figure 1.Results of a meta-analysis of RCSD1 mRNA expression in lung cancer explorer database.
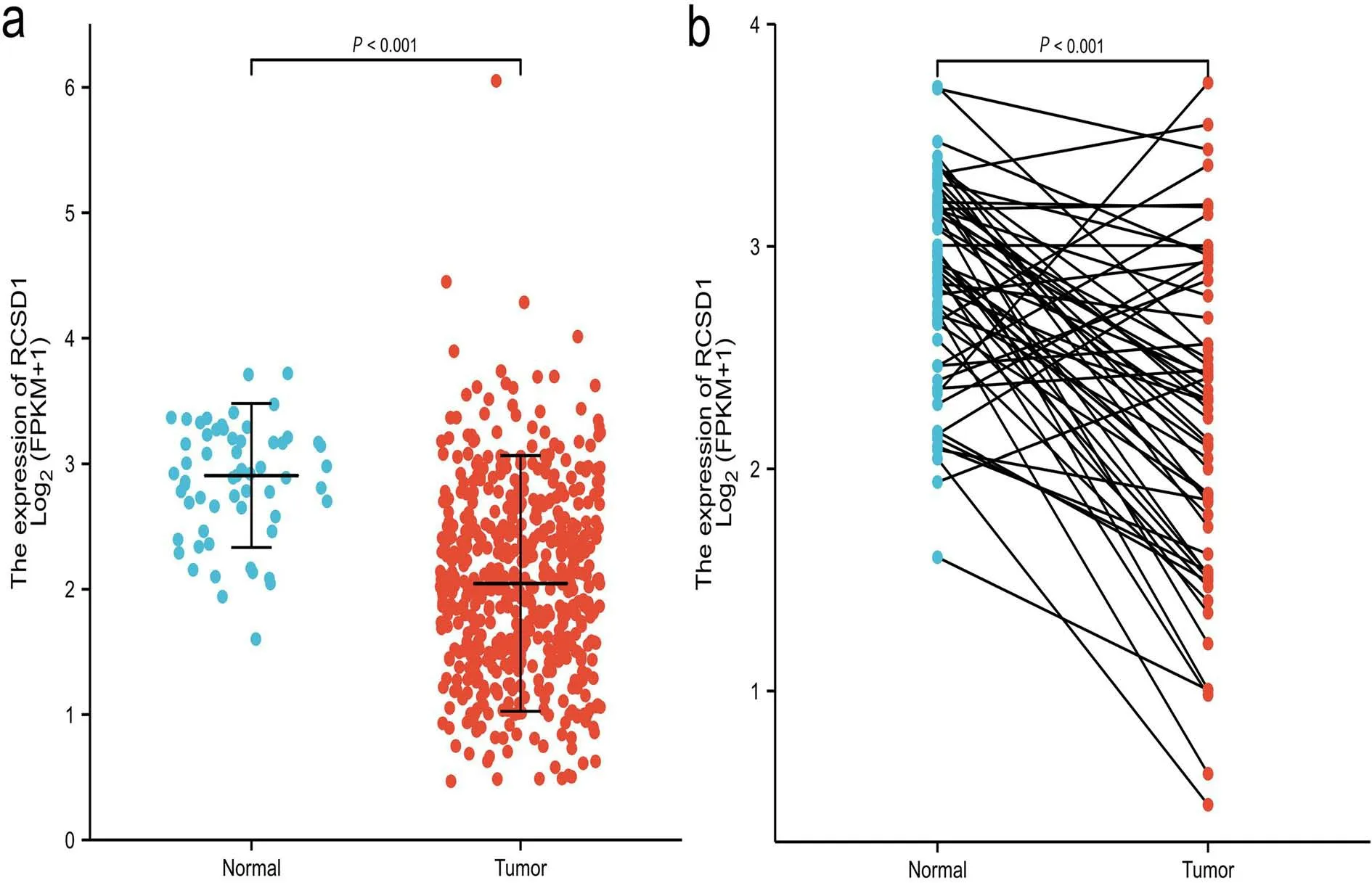
Figure 2.Unpaired and matched t-test of RCSD1 mRNA expression in patients with lung adenocarcinoma.
To further assess the relationship between RCSD1 expression and OS in lung adenocarcinoma.We downloaded prognostic data for lung adenocarcinoma from TCGA-CDR.The Kaplan-Meier curve (Fig.3a)suggests that the lower the expression of RCSD1, the shorter the OS of LUAD patients (OS: HR = 0.59, P<0.001).ROC curve was plotted based on the expression of RCSD1 (Fig.3b).The area under the ROC curve
RCSD1 mRNA expression and clinicopathological features
The expression of the RCSD1 gene is different in different groups of lung adenocarcinoma patients.(Fig.4).The expression of RCSD1 was lower in younger patients (age<=65 years) than in older patients (P=0.01;Fig.4a).The expression of RCSD1 in female patients was higher than that in male patients (P = 0.04; Fig.4b).The expression of RCSD1 in patients with T1/T2 stage was higher than that in patients with T3/T4 stage (P =0.04; Fig.4c).The expression of RCSD1 in patients with lung adenocarcinoma of N1/N2/N3 stage was lower than that of patients with N0 stage (P = 6.4e-03; Fig.4d).The expression of RCSD1 was higher in the PR and CR groups with better treatment effects than the PD and SD
The relationship between RCSD1 and immune infiltration
Biological functional analysis revealed that RCSD1 may regulate tumor immune infiltration, so it would be meaningful to elucidate the association between immune cell aggregation and RCSD1 expression.Through SSGSEA analysis, the correlation between RCSD1 and 24 kinds of immune cell subsets was investigated and expressed using the spearman correlation coefficient.RCSD1 and T cells, Th1 cells, Cytotoxic cells, B cells, macrophages, T helper cells, DC, iDC, aDC, macrophages, Treg, pDC,CD8 T cells, Tem, mast cells, neutrophils, Tcm, eosinophils, NK CD56dim cells, NK cells, Tgd and Th17 cells were positively correlated (Fig.6).To further clarify the potential relationship between RSCD1 and various immune phenotypes, we used the TISDIB database to obtain correlations between RSCD1 and immunostimulants, immunosuppressants, and chemokines.As shown in Fig.7, the expression of immunostimulants,immunosuppressants, and chemokines were significantly and positively correlated with the expression of RCSD1 in lung adenocarcinoma.Immune checkpoints have been clinically proven to affect the efficacy of cancer patients.We analyzed the correlation between RCSD1 and the immune checkpoints programmed cell death 1 (PDCD1), programmed(AUC) of RCSD1 in lung adenocarcinoma is 0.821 (CI: 0.775-0.861).The lower the expression of RCSD1, the worse the prognosis of lung adenocarcinoma, which suggests that the decreased expression of RCSD1 may promote the evolution of lung adenocarcinoma.
groups with poor treatment effects (P = 0.04; Fig.4e).Patients with high clinical stage had higher RCSD1 expression than patients with the low clinical stage (P = 1.9e-03; Fig.4f).The difference in RCSD1 expression has nothing to do with lymph node metastasis (P = 0.16; Fig.4g).As shown in Table 1, univariate Cox regression analyses show that T stage(P <0.001), N stage (P <0.001), pathologic stage (P <0.001), primary therapy outcome (P <0.001), residual tumor (P <0.001), and low expression of RCSD1 (P <0.001) are important risk factors affecting the survival time of LUAD patients.Multivariate Cox regression analysis indicates that low expression of RCSD1was an independent predictor of poor prognosis of lung adenocarcinoma(P=0.018).
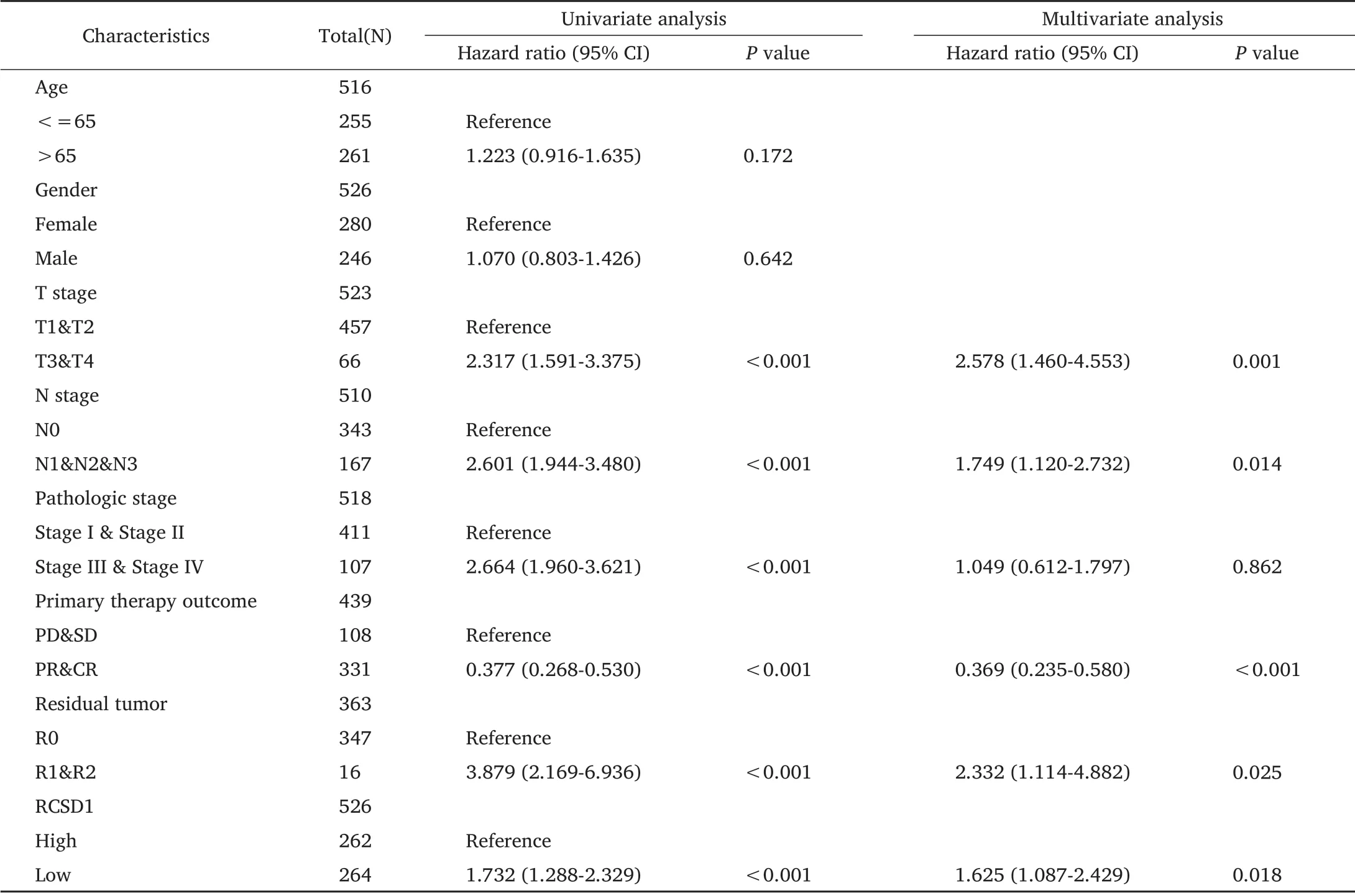
Table 1 Univariate and multivariate Cox regression analyses of RCSD1.
death-ligand 1 (PDL1, CD274), cytotoxic lymphocyte antigen 4 (CTLA4),which are of concern to clinicians.As shown in Fig.8, RCSD1 is positively correlated with PDCD1 (r=0.590), CD274 (r=0.500) and CTLA4 (r=0.690).Combined with the results of GO, KEGG, and TISDIB database analysis, RSCD1 interacts with the immune infiltration in LUAD to affect patients’survival.
Correlation between RCSD1 gene and ABL1 gene
We searched PubMed for literature on RCSD1 only found the presence of RCSD1-ABL1 fusion gene in leukemia patients.The presence of the RCSD1-ABL1 fusion gene in lung adenocarcinoma is a controversial issue.We analyzed the correlation between the RCSD1 gene and the ABL1 gene using lung adenocarcinoma sequencing data from the TCGA database.The result of the analysis (Fig.8d) suggested that there was no correlation between RCSD1 and ABL1 expression in lung adenocarcinoma(r=0.048,P=0.273).Therefore, it is reasonable to conclude that the expression of the RCSD1 gene in lung adenocarcinoma is unrelated to the presence of the ABL1 gene.RCSD1-ABL1 fusion gene does not exist in lung adenocarcinoma.
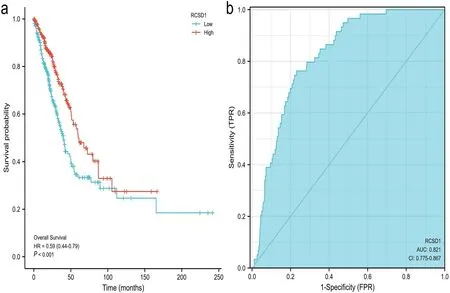
Figure 3.RCSD1 mRNA expression and prognosis of LUAD.(a) Comparison of overall survival of patients with high and low expression of RCSD1 mRNA.(b) Relationship between mRNA expression and patient prognosis.ROC,receiver operating characteristic curve;AUC,area under the curve;CI,confidence interval.
Discussion
Although the diagnosis and treatment strategies for LUAD have improved significantly over the past few decades, the prognosis for patients with LUAD remains dismal.Appropriate prognostic biomarkers predict treatment outcomes and clinical outcomes in patients who have not yet received treatment.Nowadays, more and more attention has been paid to precision medicine.Targeted therapy for prognostic markers can improve clinical efficacy and reduce the side effects of chemotherapy drugs.Previous studies have confirmed that RCSD1 promotes the onset and progression of acute leukemia, but we still know little about its clinical value in LUAD.This research suggests that low RCSD1 expression is a reliable biomarker of the clinical outcome of LUAD.
Bioinformatics analysis was used to evaluate the relationship between the prognostic role of RCSD1 in LUAD and the relationship between immune infiltration.Different from normal lung samples, the expression of RCSD1 is highly reduced in LUAD tumor tissue and is associated with a variety of clinicopathologic factors with a poor prognosis, suggesting that low RCSD1 expression promotes the progression of lung adenocarcinoma.We infer that RCSD1 can be used as a biomarker of LUAD.
To predict the pathologic mechanisms and pathways involved in low RCSD1 expression in lung adenocarcinoma, we used TCGA data to find out the co-expression of RCSD1 and other genes in the lung adenocarcinoma.The first 140 genes co-expressed with RCSD1 were selected for gene enrichment analysis.RCSD1 co-expressed genes mainly regulate T cell activation and other pathways related to immune infiltration.T cell activation induces the expression of PD1, and the combination of PD1 and PDL1 leads to a decrease in the anti-tumor immunity of lymphocytes [16].CD28 and B7 (including B7-1 and B7-2)work together to participate in the anti-tumor immune response.CTLA4 has a stronger affinity with B7 than CD28, and the expression of CTLA4 interferes with the interaction between CD28 and B7 [17].After T cells are activated, lymphocytes begin to express CTLA4.CTLA4 binds to B7 molecules on antigen-presenting cells (APC), thereby preventing them from binding to CD28 and reducing the activation state of T cells, which promotes tumor immune tolerance[18].
Different immune cells in the immune microenvironment influence each other and jointly regulate the body’s anti-tumor effect.In the pathological tissues of LUAD, the higher the expression of RCSD1, the more T cells, Cytotoxic cells, Macrophages, Treg, NK CD56dim cells, and other tumor immune infiltrating cells were found.Cytotoxic cells can recognize tumor cells that evade immunity and play an anti-tumor effect through the Fas Ligand (FasL)/Fas interaction [19].By preventing excessive immune activation, Treg cells maintain immune homeostasis in the human body.Excessive Treg activity will accelerate the formation of a variety of tumors [20].One study found that an increase in the number of tumor Treg cells increased the risk of recurrence of nonsmall cell lung cancer [21].The study found that after neoadjuvant chemoimmunotherapy for NSCLC patients, the reduction of Treg cells is significantly related to the clinical efficacy of the patients [22].The activation failure of NK cells may hinder the body's adaptive immunity,and activation of NK cells may have clinical benefits for patients with lung cancer[23].
In LUAD, RCSD1 is significantly positively correlated with immunostimulants (CD48, CD28, CD40LG), immunosuppressive agents(BTLA, CD96, TIGIT), chemokines (CCL19, CCL5, CXCL9), and other immunophenotypes.CD48 and CCL19 genes were found to promote brain metastasis of lung cancer [24].In young patients with lung adenocarcinoma, when CD28 is highly expressed, the DFS of the patient is shorter but the OS is longer, possibly because CD28 is involved in different stages of tumor microenvironment regulation [25].As an immunosuppressive molecule, BTLA mediates the immune evasion of hematological tumors by down-regulating the proximal T cell receptor signaling cascade [26].In NSCLC, high expression of BTLA may predict adverse outcomes for patients [27].TIGHT is a co-inhibitory receptor that promotes the up-regulation of TIM3 expression on Treg cells and works with TIM3 to inhibit tumor immune response [28].A previous study has found that the direct interaction between CD96 and CD155 can promote immunosuppression of lung adenocarcinoma [29].CCL5 promotes lung adenocarcinoma migration by increasing the expression of alphavbeta3 integrin on human lung adenocarcinoma cells (A549 cells) [30].In mouse lung cancer cells, the CXCL9 gene can play an anti-cancer effect, which does not depend on blocking tumor angiogenesis [31].After surgery,compared with relapsed patients, the CXCL9 concentration in the tumor blood of non-recurring NSCLC patients was lower than the peripheral blood concentration [32].This suggests that it may be possible to detect tumor recurrence by detecting the concentration of CXCL9 in the peripheral blood.
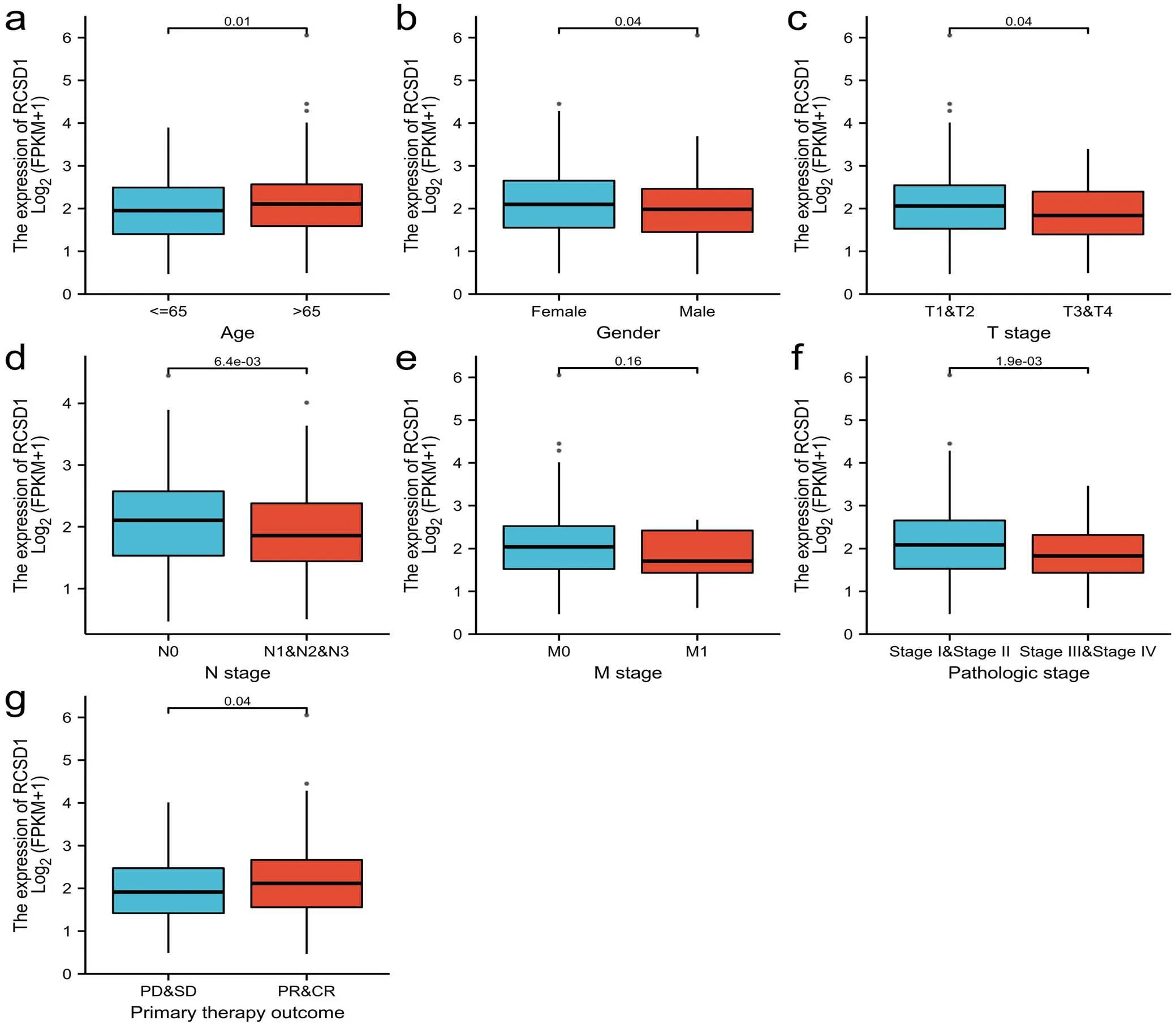
Figure.4 RCSD1 expression and clinical characteristics.(a) age.(b) gender.(c) T stage.(d) N stage.(e) M stage.(f) pathologic stage.(g) primary therapy outcome.PD,disease progression;SD,stable disease;PR,partial relief;CR,complete remission.
We found that common immune checkpoints such as PDCD1,PDL1, CTLA4, and RCSD1 are positively correlated.Due to the association between immune checkpoints and RCSD1 in LUAD, immune checkpoint inhibitors may also affect the expression of RCSD1 in lung adenocarcinoma and help improve LUAD treatment and prognosis.Based on the analysis results, the regulation of immune infiltration may be a key factor for the poor prognosis and poor survival rate of LUAD patients caused by the low expression of RCSD1.
Our study initially revealed the relationship between RCSD1 and LUAD patients’ prognosis and immune infiltration, but it is undeniable that there are certain limitations.This study mainly relies on bioinformatics analysis.The mechanism of RCSD1 in lung adenocarcinoma needs to be verified by further cell experiments.The effect of RCSD1 expression on the anti-tumor effect of immune cells needs to be further confirmed by subsequent studies.
Conclusion
Our research reveals the potential role of RCSD1 in tumor immunology.RCSD1 can be used as a new biomarker to assess the status of the tumor microenvironment and a potential immunotherapy target for LUAD patients.
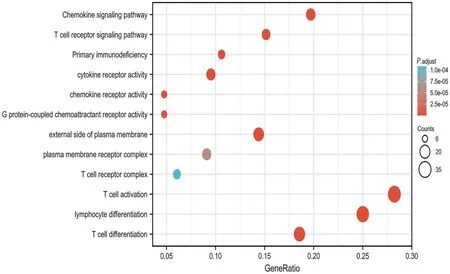
Figure 5.GO and KEGG analysis of RCSD1 co-expression genes.GO, gene ontology; KEGG, Kyoto encyclopedia of genes and genomes; BP, biological process; MF,molecular function;CC,cellular component.

Figure 6.Correlations between RCSD1 expression and immune cells.
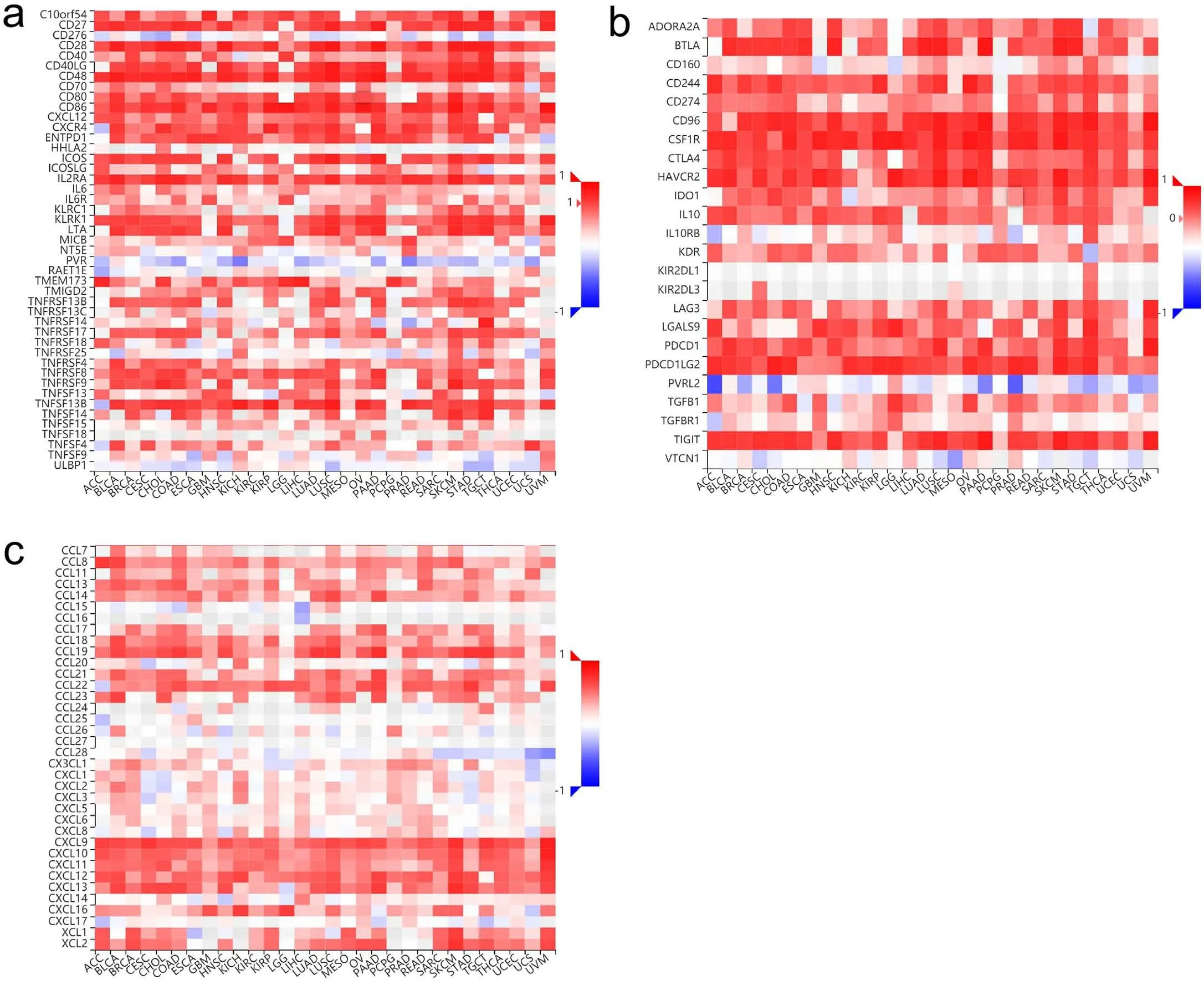
Figure 7.Correlation of RSCD1 gene with immunostimulants,immunosuppressants and chemokines.
- Life Research的其它文章
- Increased internet addiction during COVID-19 pandemics
- Intracranial hemangiopericytoma with right-sided aortic arch:a case report and summary of experience
- Advances of biodegradable magnesium-based implants for orthopaedics
- Graft rejection after deep anterior lamellar keratoplasty in fellow eye in macular corneal dystrophy:a case report
- Utility of convalescent plasma for addressing the COVID-19 infection:brief review and case reports
- Molecular mechanism of different viruses associated with autoimmunity