Graft rejection after deep anterior lamellar keratoplasty in fellow eye in macular corneal dystrophy:a case report
He Dong, Jian Yu, Xun Wang, Jun-Zhang Li
Abstract Because of the low incidence of immunological rejection, deep anterior lamellar keratoplasty (DALK) is currently the preferred treatment for macular corneal dystrophy(MCD).However,there were few reports about whether the consistent results were obtained when performing DALK in both eyes for MCD, especially when the corneal grafts were taken from different donors.Also, there were few reports about whether the stromal graft rejection occurred typically in both eyes in MCD with DALK.This case may represent the first report of an unusual and misleading manifestation of stromal graft rejection after uneventful DALK with big bubble technique in the fellow eye in MCD.A 32-year-old healthy man with MCD underwent bilateral uneventful DALK with a big bubble technique in the left eye in January and the right eye in July, the corneal grafts were taken from different donors.There was an atypical allograft rejection that occurred in the right eye and none in the left eye; although a timely diagnosis of graft rejection revealed following aqueous determination, it could not be reversed and underwent PK finally.The purpose of this case report is to illustrate the identification of atypical allograft rejection after DALK in the fellow eye,the significance of aqueous detection in the diagnosis of graft rejection,the choosing of grafts,and the timing of bilateral corneal transplantation in patients with MCD.
Keywords:macular corneal dystrophy;deep anterior lamellar keratoplasty;postoperative rejection;viral keratitis
Background
Macular corneal dystrophy (MCD) is a bilateral autosomal recessive hereditary disease that typically progresses to significant corneal opacities and thinning, leading to progressive vision loss.The progressive intra- and extracellular accumulation of glycosaminoglycans in stromal keratocytes,Descemet membrane (DM), and endothelial cells are the main pathogenetic factor of MCD.In these cases, surgical interventions must be considered, such as penetrating keratoplasty (PK) and deep anterior lamellar keratoplasty (DALK).Despite the high success rate, corneal transplantation is still confused by a relevant risk of graft rejection [1].Traditionally, PK has been performed to restore visual acuity with excellent results in MCD.However, due to the risk of endothelial rejection and intraocular complications, anterior lamellar keratoplasty techniques have been described as big bubble DALK.Big bubble DALK is a widespread technique, involving partial-thickness trephination followed by injection of air into the corneal stroma to create a giant bubble between DM and corneal stroma.The latest research shows that when compared with PK, DALK eliminates the possibility of endothelial allograft rejection, which is the main reason for graft failure after PK.More importantly, it has the advantage of lower open sky intraoperative complications and fewer endothelial cell loss [2].Although there is no endothelial immune reaction after uneventful big bubble DALK, stromal graft rejection after DALK can present with the same features as endothelial graft rejection.It should be differentiated from other similar demonstrations such as viral-induced endothelitis.We offered a case of a young man with MCD who developed an unusual and misleading postoperative stromal graft rejection without any neovascularization in the graft and recipient bed following a repeat DALK in the right eye after an initial uneventful DALK in the left eye.The graft rejection was identified by aqueous virology and inflammatory cytokine determination with polymerase chain reaction (PCR) and cytometric bead array (CBA)(Beijing GIANTMED medical diagnostics lab), it was irreversible, and a second penetrating keratoplasty was performed to significant visual improvement.
Case Presentation
A 32-year-old man with a gradual decrease in vision in both eyes for 7 years was referred to our hospital on December 29, 2018.The patient did not have a relevant family history.The best-corrected visual acuity(BCVA) was 0.2 for the right eye and 0.25 for the left eye, respectively.The intraocular pressure (IOP) in both eyes was 12 mmHg.The axial length was 27.28 mm for the right eye and 27.13 mm for the left eye as measured by an IOL Master (Carl Zeiss).On slit-lamp biomicroscopic examination, conjunctival congestion, multiple, diffuse, indistinct,underlying stromal opacities located in the central cornea in both eyes(Fig.1a and b).Anterior segment optical coherence tomography (AS-OCT,Visante, Carl Zeiss) revealed smooth DM and endothelium.Confocal microscopy (HRT3, Heidelberg Engineering GmbH) revealed the granular,hyperreflective appearance of the corneal stroma with multiple, differently oriented dark striae.Combined with the results of OCT and confocal microscopy of the patient’s anterior segment, the diagnosis of MCD was made, with the patient’s informed consent, the tents of the Declaration of Helsinki were followed, DALK was performed in the left eye in January and the right eye in July.The 0.5% levofloxacin was prescribed for 1 week preoperation, and the corneal donors were all cryopreserved (stored at pure glycerin -20℃).Anterior lamellar of the cornea was removed down to the DM with a big bubble technique and it was found that the lesion did not affect the DM and endothelium.Finally, DALK were completed in both eyes (Fig.1c and d).The postoperative regimen included a combination of topical antibiotics, topical and systemic steroids.Systemic hydrocortisone was used for 5 days and then changed to oral prednisone tablets, 70 mg taken at a draught in the morning, and was tapered and continued for 3 months.Topical prednisolone acetate 1%was applied four times per day and used for at least 6 months.The topical tacrolimus 0.1% was applied two times per day when corneal epithelial wound healing.Topical Ofloxacin 0.3% was prescribed for 2 weeks, and the preservative-free artificial tears were also applied.
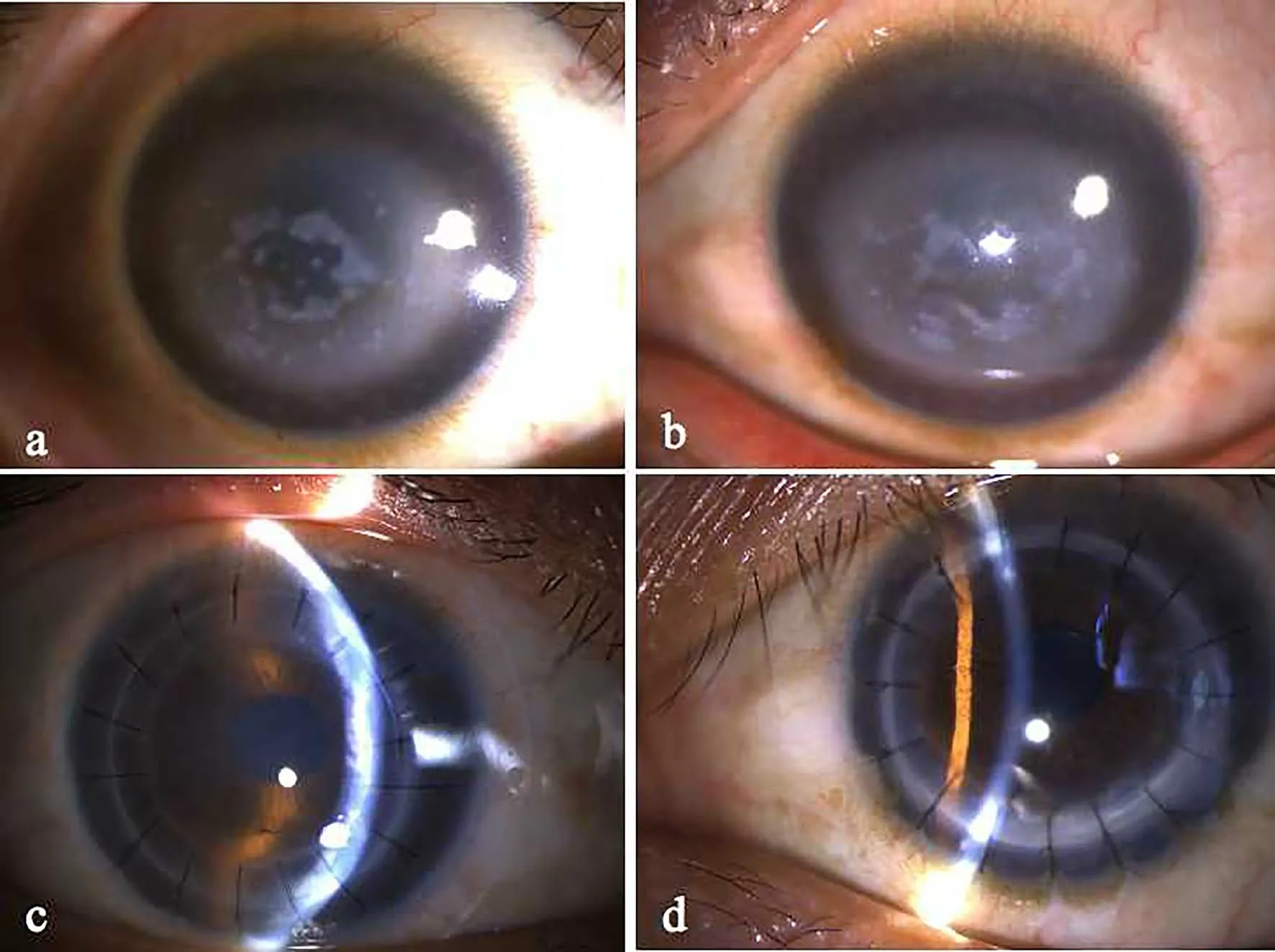
Figure 1.Representative slit-lamp photographs(BQ900,Haag-Streit AG,CSO,Italy;magnification 10×)of the right eye(a,c)and left eye(b,d).(a,b)Multiple,diffuse,grayish, indistinct, deeper corneal opacities accompanied by subepithelial are visible.The severity of the corneal changes was comparable between the eyes.(c, d) Clear grafts 1 week after DALK.
One month after surgery in the right eye, the patient presented to our department with complaints of ocular discomfort, red-eye and decreased vision in the right eye.The IOP of his right eye was 50 mmHg.Slit-lamp examination showed conjunctival congestion, edema of graft stroma.There were few very fine keratic precipitates (KPs) in the allograft and the recipient bed.Anterior chamber (AC) inflammation with cells and flair without any vascularization in the graft and recipient bed, and without any infiltration or loosening of the sutures.He was admitted to the hospital with secondary glaucoma, was managed with mannitol 20%intravenously once per day and routine topical medications to control intraocular pressure such as brinzolamide, latanoprost, carteolol.Topical prednisolone acetate 1%, and tacrolimus 0.1% eye drops combined with preservative-free artificial tears were used for treatment.The IOP was decreased to 17 mmHg after 3 days and observed to be stable after discharge.The stromal edema was markedly reduced after 6 days and was resolved within 14 days, accompanied by regression of KPs and AC inflammation.After 3 weeks, there was a clear graft with BCVA 20/40.The topical corticosteroid was tapered and continued.
Six months after the surgery in the right eye, the patient was referred with the same signs and symptoms with graft edema.KPs were limited to the graft location.IOP was 19 mmHg.The BCVA was CF/30 cm in his right eye.Slit-lamp biomicroscopy showed that the graft was edematous and there was moderate conjunctive congestion with KPs and cells in the AC of the right eye.The fresh and fine size KPs were localized to the area of stromal edema of the graft without any vascularization in the graft and recipient bed without any infiltration or loosening of the sutures (Fig.2a).AS-OCT revealed that the corneal endothelium was smooth.To distinguish it from viral keratitis, PCR and CBA analysis were performed on an aqueous sample, which was negative for herpes simple virus (HSV),cytomegalovirus (CMV), varicella zoster virus (VZV) and Epstein-Barr virus (EBV), and there was a significant increase in the levels of interleukin-6 (IL-6) and interleukin-8 (IL-8).Table 1 presents the PCR and CBA analysis of the aqueous sample.Furthermore, a clinical diagnosis of postoperative graft rejection was made.The patient was managed withtopical prednisolone acetate 1% eye drops hourly, tacrolimus 0.1% eye drops four times per day.Systemic hydrocortisone was used for 5 days and then changed to oral prednisone tablets, 50 mg taken at a draught in the morning, and was tapered and continued for 3 months.After 1 month,it was resolved and there was an opacity graft with BCVA 20/200.
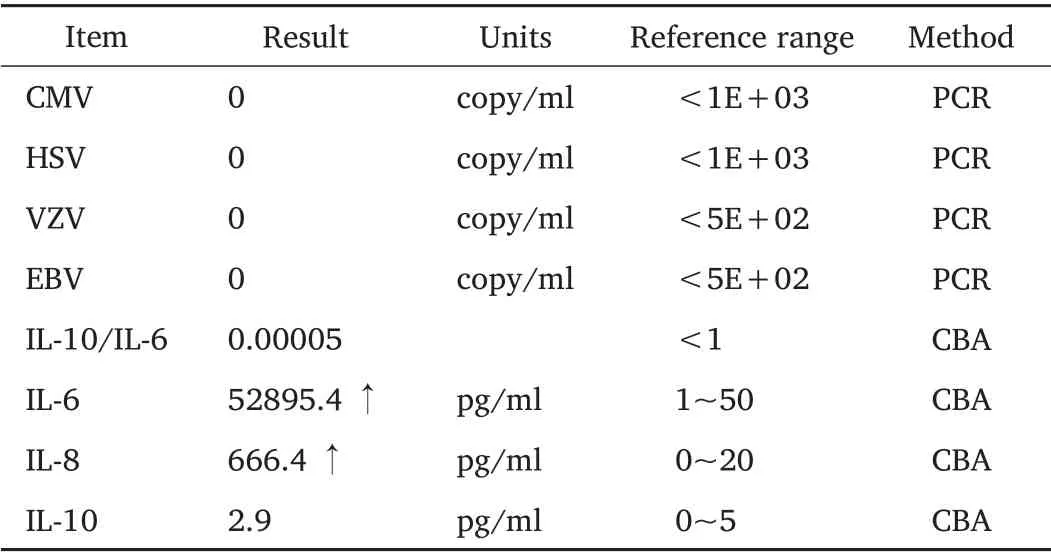
Table 1
Eleven months after the surgery in the right eye, the patient was referred again with the same complaints.Slit-lamp biomicroscopy revealed the presence of acute corneal graft edema and infiltration with KPs.The sutures were loosened and without evidence of any vascularization in the graft and recipient bed.Accompanied inflammation with cells and flair in the AC (Fig.2b).The best-corrected visual acuity (BCVA) was HM/20 cm.The IOP was 16 mmHg using an applanation tonometer.He received the same topical and systemic medications as before, but the inflammatory response and edema of the allograft were irreversible.Therefore, with the patient’s informed consent, the DALK was proposed.However, spontaneous rupture of the DM occurred during the operation,and the PK was performed.After 2 months, there was a clear graft with BCVA 20/40 in the right eye(Fig.2c).
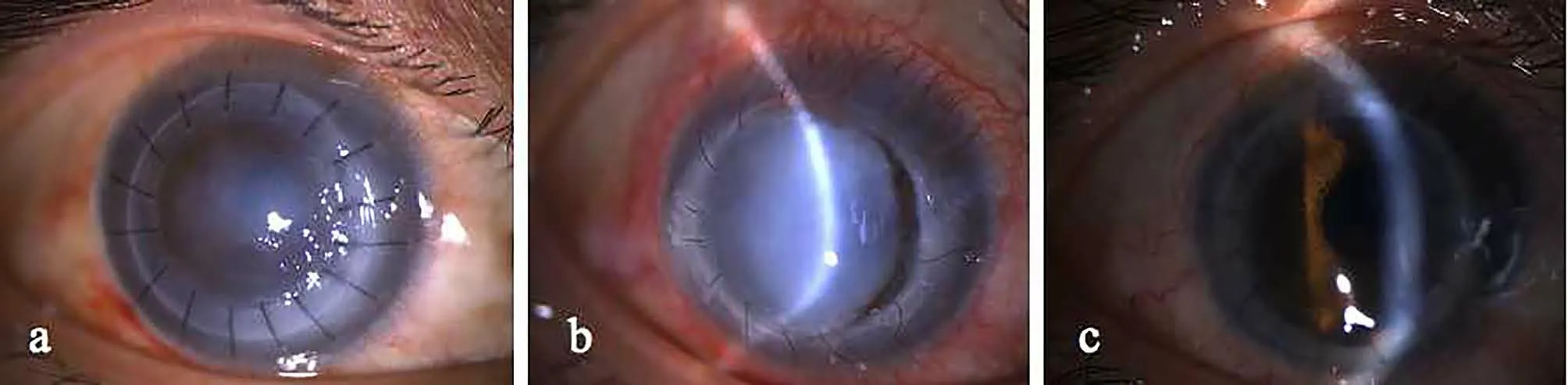
Figure 2.Representative slit-lamp photographs (BQ900, Haag-Streit AG, CSO, Italy; Magnification 10 ×) of the right eye.(a) 6 months after DALK.(b) 11 months after DALK.(c)2 months after PK.
Discussion and Conclusions
DALK is considered an alternative to PK in MCD without DM or endothelium involvement.Although there is no endothelial immune reaction after DALK, stromal graft rejection after DALK can occur and present typically with graft stromal edema and stromal haze occurring especially near the blood vessels and interface neovascularization, that the same features as other similar demonstrations such as viral-induced endothelitis, it is difficult to distinguish them.Moreover, there was no general consensus of surgery regarding the choice of donors and ideal timing on both eyes in MCD.Graft rejection incidence varies considerably among studies and about the specific surgical technique evaluated.Williams et al.reported that the failure of the graft due to irreversible rejection was 28% for PK (n=5687), 1.7% for DALK (n=113) from a consecutive cohort of 33000 grafts since May 1985 [3].The graft endothelium may play an essential role in rejection and maintaining of T-cell activation via the direct and/or the indirect pathways of allorecognition [4].The main factor for lower rejection rates of DALK than PK is considered that DALK is based on traditional lamellar keratoplasty, the pathological corneal stroma tissue of the recipient was removed completely down to the DM, and the donor corneal graft without DM and endothelium was transplanted on the recipient bed [5].Although there is no endothelial immune reaction after DALK, epithelial,subepithelial and stromal rejection can occur after DALK [6].The classic“corneal limbus approach” theory of immune rejection can explain the clinical phenomenon of epithelial, subepithelial and stromal graft rejection.After the corneal transplantation, the donor-derived antigens were recognized by the antigen-presenting cells of the recipient’s limbus and further presented to and activated by the recipient’s T cells [7].The activated T cells undergo systemic circulation and the corneal neovascularization and lymphatic vessels reach the cornea, which will damage the allogeneic corneal grafts and cause immune rejection[8,9].
The typical allograft stromal rejection following DALK may present as corneal edema, hazy and partial stromal infiltration with neovascularization limited to the graft area.The contributing factors of allograft rejection after DALK are loose sutures, previous vascularization and vernal keratoconjunctivitis, and PK in the fellow eye.For our studied patient, DALK with giant bubble technique surgery and antirejection therapy were performed at the same condition in both eyes, but the corneal grafts were taken from different donors.The left eye did not appear any rejection.Whereas the right eye presented an atypical allograft rejection at six months after surgery that appeared with stromal edema without neovascularization.The edema gradually spread over the entire stroma at eleven-month after surgery.The inflammatory of the stroma may be disturbed endothelial function and cause stromal edema.The inflammation reaction of the AC may be secondary to the occurrence of stromal inflammation and its spillover.According to “the classical theory”, a possible explanation is that the T cells in the recipients can be activated after the first corneal transplantation, and then the activated T cells attack the antigen of the allogeneic corneal graft, leading to rejection after corneal transplantation in the fellow eye.Most of the rejection after DALK can be eliminated by steroid hormones, but in our case, the rejection was irreversible, corneal transplantation was finally performed again.It is probable that taking corneal grafts from the same donor may reduce the allograft rejection in DALK with MCD in both eyes.
Timely diagnosis of allograft stromal rejection after DALK and its prompt and meticulous management is mandatory in order to prevent the consequences of untreated stromal rejection, including vascularization and opacification of the graft, which results in permanent stromal scarring may lead to profound visual loss.Allograft stromal rejection can present with the same features as virus-induced keratitis or endothelial rejection,such as in our case.Our patient had no previous history of allergic keratoconjunctivitis and herpes simplex virus keratitis, timely diagnosis of allograft rejection was clarified by an aqueous sample determination with PCR and CBA, and active anti-rejection treatment with glucocorticoid was recommended immediately.However, the allograft rejection was irreversible with the management of medicines, a repeat corneal transplant was performed eventually.
In conclusion, allograft stromal rejection remains a significant complication after DALK,especially in the fellow eye in patients with MCD.In this condition, the choice of grafts from the same donor and the timing of bilateral DALK before the lesions involved DM and endothelium should be preferred.This unusual presentation of allograft stromal rejection should be differentiated from similar presentations such as viralinduced keratitis, and aqueous detection is an effective method for timely identification.
- Life Research的其它文章
- Increased internet addiction during COVID-19 pandemics
- Intracranial hemangiopericytoma with right-sided aortic arch:a case report and summary of experience
- Advances of biodegradable magnesium-based implants for orthopaedics
- Low expression of novel biomarker RCSD1 predicts poor prognosis of lung adenocarcinoma
- Utility of convalescent plasma for addressing the COVID-19 infection:brief review and case reports
- Molecular mechanism of different viruses associated with autoimmunity